Urology
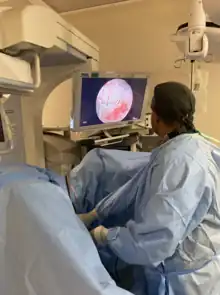 Urologist performing a TURP | |
| Occupation | |
|---|---|
Occupation type | Specialty |
Activity sectors | Medicine, surgery |
| Description | |
Education required | |
Fields of employment | Hospitals, clinics |
Urology (from Greek οὖρον ouron "urine" and -λογία -logia "study of"), also known as genitourinary surgery, is the branch of medicine that focuses on surgical and medical diseases of the male and female urinary-tract system and the male reproductive organs. Organs under the domain of urology include the kidneys, adrenal glands, ureters, urinary bladder, urethra, and the male reproductive organs (testes, epididymis, vas deferens, seminal vesicles, prostate, and penis).
The urinary and reproductive tracts are closely linked, and disorders of one often affect the other. Thus a major spectrum of the conditions managed in urology exists under the domain of genitourinary disorders. Urology combines the management of medical (i.e., non-surgical) conditions, such as urinary-tract infections and benign prostatic hyperplasia, with the management of surgical conditions such as bladder or prostate cancer, kidney stones, congenital abnormalities, traumatic injury, and stress incontinence.[1]
Urological techniques include minimally invasive robotic and laparoscopic surgery, laser-assisted surgeries, and other scope-guided procedures. Urologists receive training in open and minimally invasive surgical techniques, employing real-time ultrasound guidance, fiber-optic endoscopic equipment, and various lasers in the treatment of multiple benign and malignant conditions.[2][3] Urology is closely related to (and urologists often collaborate with the practitioners of) oncology, nephrology, gynaecology, andrology, pediatric surgery, colorectal surgery, gastroenterology, and endocrinology.
Urology is one of the most competitive and highly sought surgical specialties for physicians, with new urologists comprising less than 1.5% of United States medical-school graduates each year.[4][5]
Urologists are physicians which have specialized in the field after completing their general degree in medicine. Upon successful completion of a residency program, many urologists choose to undergo further advanced training in a subspecialty area of expertise through a fellowship lasting an additional 12 to 36 months. Subspecialties may include: urologic surgery, urologic oncology and urologic oncological surgery, endourology and endourologic surgery, urogynecology and urogynecologic surgery, reconstructive urologic surgery (a form of reconstructive surgery), minimally-invasive urologic surgery, pediatric urology and pediatric urologic surgery (including adolescent urology, the treatment of premature or delayed puberty, and the treatment of congenital urological syndromes, malformations, and deformations), transplant urology (the field of transplant medicine and surgery concerned with transplantation of organs such as the kidneys, bladder tissue, ureters, and, recently, penises), voiding dysfunction, paruresis, neurourology, and androurology and sexual medicine. Additionally, some urologists supplement their fellowships with a master's degree (2–3 years) or with a Ph.D. (4–6 years) in related topics to prepare them for academic as well as focused clinical employment.
Training
United States
In 2014, there were 126 residency programs that offered 296 categorical positions.[6] Urology is one of the early match programs, with results given to applicants by late January (6 weeks before NRMP match). Applications are accepted starting Sep 1, with some programs accepting applications until early Jan.[7]
It is a relatively competitive specialty to match into, with only 68% to 77% of US seniors matching between 2012 and 2015.[6] The number of positions has grown from 278 in 2012 to 296 in 2015. Matching is significantly more difficult for IMGs and students who have a year or more off before residency - match rates were 27% and 55% respectively in 2012.[8]
The medical school environment may also be a factor. A study in 2012 also showed after an analysis of match rates from schools between 2005 and 2009 that 20 schools sent more than 15 students into urology (1 standard deviation above the median), with Northwestern University sending 44 students over those 5 years.[9]
After urology residency, there are seven subspecialties recognized by the AUA (American Urological Association):
- Oncology
- Calculi
- Female Urology
- Infertility
- Pediatrics
- Transplant (renal)
- Neurourology.[10]
Australia
Training is completed through the Royal Australasian College of Surgeons[11] (RACS). The program requires six years of full-time training (for those who commenced prior to 2016), or five years for those who commenced after 2016.[12] The program is accredited by the Australian Medical Council.[11]
Pre-requisites include:[13]
- Australian Citizenship, New Zealand Citizenship or Australian Permanent Residency
- General medical registration
- Completion of PGY2 (see: Medical education in Australia)
- Completion of the RACS Hand Hygiene Learning Module
Nepal
In Nepal, the formal urologist degree awarded is MCh (Magister Chirurgiae).[14] This is a three years course post masters and includes thesis and a mandatory publication. This degree is awarded after completing MBBS (four and half year plus a one-year rotatory internship) and MS (Mastery of surgery) in general surgery (three years course). Till now two Universities Tribhuvan University and Kathmandu University as well as two Autonomous institutes BP Koirala Institute of health sciences and National Academy of Medical Sciences (Bir Hospital) run the MCh Urology programme.19, 20 This degree is equivalent to Clinical PhD and called as "Chikitsa Bidhyabaridhi" by Tribhuvan University (Government University) and is considered to be the highest degree among the surgical discipline degrees. Besides Urology, Cardiothoracic and Vascular Surgery, Surgical Gastroenterology, Plastic Surgery, and Neurosurgery MCh programmes also run in the country.
Ethiopia
Urology is a relatively new field in Ethiopia. By 2001, there were only five qualified Urologists in the country. All trained abroad, in countries like India, Tanzania and Hungary. Before this chapter all Urology cases were managed by General surgeons. The only Urological Unit in the country was at Tikur Anbessa Tertiary Hospital. The services provided included ESWL and Endo- urology. The Urology training program was started in 2009 with a curriculum for General Surgeons which had a three-year training program. Up to 2019 six Urologists have graduated by this program for General surgeons. The first residency program started accepting General practitioners in 2010 for a five-year program. [15] The first two years were trainings in General surgery, the next three years were dedicated urology training program, which included the same three year training as of the General surgeons three year curriculum. It started with two residents who graduated in 2015 with a certificate in specialty of Urology. Up to 2019 seventeen Urologists have graduated from this five year residency program. From the start these programs in 2009 up to 2019, a total of 23 urologists have been trained in Tikur Anbessa Tertioary Hospital. Currently there are 26 trainees in the program. One General surgeon who is in the 2nd year of the three year program and 25 residents who completed two years of general surgery training, as of 2020, 6 are in PGY3, 10 PGY4 and 9 PGY5. All of the Urologists who graduated from Tikur Anbessa Tertioary Hospital are currently working in different parts of the country[15]
Subdisciplines
As a medical discipline that involves the care of many organs and physiological systems, urology can be broken down into several subdisciplines. At many larger academic centers and university hospitals that excel in patient care and clinical research, urologists often specialize in a particular sub discipline.
Endourology
Endourology is the branch of urology that deals with the closed manipulation of the urinary tract.[16] It has lately grown to include all minimally invasive urologic surgical procedures. As opposed to open surgery, endourology is performed using small cameras and instruments inserted into the urinary tract. Transurethral surgery has been the cornerstone of endourology. Most of the urinary tract can be reached via the urethra, enabling prostate surgery, surgery of tumors of the urothelium, stone surgery, and simple urethral and urethral procedures. Recently, the addition of laparoscopy and robotics has further subdivided this branch of urology.
Laparoscopy
Laparoscopy is a rapidly evolving branch of urology and has replaced some open surgical procedures. Robot-assisted surgery of the prostate, kidney, and ureter has been expanding this field. Today, many prostatectomies in the United States are carried out by so-called robotic assistance. This has created controversy, however, as robotics greatly increase the cost of surgery and the benefit for the patient may or may not be proportional to the extra cost. Moreover, current (2011) market situation for robotic equipment is a de facto monopoly of one publicly held corporation[17] which further fuels the cost-effectiveness controversy.
Urologic oncology
Urologic oncology concerns the surgical treatment of malignant genitourinary diseases such as cancer of the prostate, adrenal glands, bladder, kidneys, ureters, testicles, and penis, as well as the skin and subcutaneous tissue and muscle and fascia of those areas (that particular subspecialty overlaps with dermatological oncology and related areas of oncology). The treatment of genitourinary cancer is managed by either a urologist or an oncologist, depending on the treatment type (surgical or medical). Most urologic oncologists in Western countries use minimally invasive techniques (laparoscopy or endourology, robotic-assisted surgery) to manage urologic cancers amenable to surgical management.
Neurourology
Neurourology concerns nervous system control of the genitourinary system, and of conditions causing abnormal urination. Neurological diseases and disorders such as a stroke, multiple sclerosis, Parkinson's disease, and spinal cord injury can disrupt the lower urinary tract and result in conditions such as urinary incontinence, detrusor overactivity, urinary retention, and detrusor sphincter dyssynergia. Urodynamic studies play an important diagnostic role in neurourology. Therapy for nervous system disorders includes clean intermittent self-catheterization of the bladder, anticholinergic drugs, injection of Botulinum toxin into the bladder wall and advanced and less commonly used therapies such as sacral neuromodulation. Less marked neurological abnormalities can cause urological disorders as well—for example, abnormalities of the sensory nervous system are thought by many researchers to play a role in disorders of painful or frequent urination (e.g. painful bladder syndrome also known as interstitial cystitis).
Pediatric urology
Pediatric urology concerns urologic disorders in children. Such disorders include cryptorchidism (undescended testes), congenital abnormalities of the genitourinary tract, enuresis, underdeveloped genitalia (due to delayed growth or delayed puberty, often an endocrinological problem), and vesicoureteral reflux.
Andrology
Andrology is the medical specialty that deals with male health, particularly relating to the problems of the male reproductive system and urological problems that are unique to men such as prostate cancer, male fertility problems, and surgery of the male reproductive system. It is the counterpart to gynaecology, which deals with medical issues that are specific to female health, especially reproductive and urologic health.
Reconstructive urology
Reconstructive urology is a highly specialized field of male urology that restores both structure and function to the genitourinary tract. Prostate procedures, full or partial hysterectomies, trauma (auto accidents, gunshot wounds, industrial accidents, straddle injuries, etc.), disease, obstructions, blockages (e.g., urethral strictures), and occasionally, childbirth, can necessitate reconstructive surgery. The urinary bladder, ureters (the tubes that lead from the kidneys to the urinary bladder) and genitalia are other examples of reconstructive urology.
Female urology
Female urology is a branch of urology dealing with overactive bladder, pelvic organ prolapse, and urinary incontinence. Many of these physicians also practice neurourology and reconstructive urology as mentioned above. Female urologists (many of whom are men) complete a 1–3-year fellowship after completion of a 5–6-year urology residency.[18] Thorough knowledge of the female pelvic floor together with intimate understanding of the physiology and pathology of voiding are necessary to diagnose and treat these disorders. Depending on the cause of the individual problem, a medical or surgical treatment can be the solution. Their field of practice heavily overlaps with that of urogynecologists, physicians in a sub-discipline of gynecology, who have done a three-year fellowship after a four-year OBGYN residency.[18]
Journals and organizations
There are a number of peer-reviewed journals and publications about urology, including The Journal of Urology, European Urology, the African Journal of Urology, British Journal of Urology International, BMC Urology, Indian Journal of Urology, Nature Reviews Urology, and Urology.
There are national organizations such as the American Urological Association, the American Association of Clinical Urologists,[19] European Association of Urology, the Large Urology Group Practice Association (LUGPA),[19] and The Society for Basic Urologic Research. Urology is also included under the auspices of the International Continence Society.
Teaching organizations include the European Board of Urology, as well as the Vattikuti Urology Institute in Detroit, which also hosts an annual International Robotic Urology Symposium devoted to new technologies. The American non-profit IVUMed teaches urology in developing countries.
Urology in the COVID19 pandemic
During the COVID-19 pandemic, urology services around the globe suspended their activities in affected countries and regions. International Associations (such as European Association of Urology, New Zealand and Australia Association of Urology) and urology departments from universities (Cleveland Clinic and others) have provided guidelines and recommendations on which urological procedures should or should not be prioritized during the pandemic. Optimizing resources and preventing patients with priority diseases from being negatively impacted. A systematic review was published in the journal European Urology Focus, summarizing such recommendations.[20]
List of urological topics
- Benign prostatic hyperplasia
- Bladder stones
- Bladder cancer
- Cystitis
- Development of the urinary and reproductive organs
- Epididymitis
- Erectile dysfunction
- Interstitial cystitis
- Kidney transplant
- Kidney cancer
- Kidney stone
- Postorgasmic illness syndrome
- Prostatitis
- Prostate cancer
- Retrograde pyelogram
- Retrograde ureteral
- Testicular cancer
- Vasectomy
- Vasectomy reversal
See also
- Category:Urology journals
- Category:Urology organizations
- Urology: COVID-19 pandemics
References
- ↑ "Urology". American Medical Association. Retrieved 28 April 2020.
- ↑ "Urologist in Noida". Full Details Information. 27 March 2019.
- ↑ Marks AJ; Teichman JM (2007). "Lasers in clinical urology: State of the art and new horizons". World Journal of Urology. 25 (3): 227–233. doi:10.1007/s00345-007-0163-x. PMID 17393172. S2CID 23167891.
- ↑ Ahmed K; Jawad M; Dasgupta P; Darzi A; et al. (2010). "Assessment and maintenance of competence in urology". Nat Rev Urol. 7 (7): 403–13. doi:10.1038/nrurol.2010.81. PMID 20567253. S2CID 24794856.
- ↑ "Facts: Applicants, Matriculants, Enrollment, Graduates, MD/PhD, and Residency Applicants Data - Data and Analysis". AAMC. Retrieved 2013-09-01.
- 1 2 https://residency.wustl.edu/Choosing/SpecDesc/Pages/Urology.aspx
- ↑ "American Urological Association - Accredited U.S. Urology Residency Programs". www.auanet.org.
- ↑ "Urology Residency Guide - Urology Match". www.urologymatch.com.
- ↑ Kutikov, A; Bonslaver, J; Casey, J. T.; Degrado, J; Dusseault, B. N.; Fox, J. A.; Lashley-Rogers, D; Richardson, I; Smaldone, M. C.; Steinberg, P. L.; Trivedi, D. B.; Routh, J. C. (2010). "The Gatekeeper Disparity: Why Do Some Medical Schools Send More Medical Students into Urology?". The Journal of Urology. 185 (2): 647–652. doi:10.1016/j.juro.2010.09.113. PMC 3058515. PMID 21168862.
- ↑ "Urology - An Overview - Urology Match". www.urologymatch.com.
- 1 2 (RACS), Royal Australasian College of Surgeons. "Urology". www.surgeons.org. Retrieved 2018-01-24.
- ↑ "Overview - Urological Society of Australia and New Zealand". www.usanz.org.au. Retrieved 2018-01-24.
- ↑ "Urology". Australian Medical Association. 2016-02-17. Retrieved 2018-01-24.
- ↑ "Department of Urology and Kidney Transplant Surgery". TUTH. Tribhuvan University Teaching Hospital. Retrieved 6 February 2021.
- 1 2 "College of Health Sciences | Addis Ababa University Sites site".
- ↑ "Website of the Endourologic Society". Endourology.org. Retrieved 2013-09-01.
- ↑ "Intuitive Surgical, Inc". Intuitivesurgical.com. Retrieved 2013-09-01.
- 1 2 http://sufuorg.com/Professional-Resources/Fellowships/Fellowship-Programs.aspx
- 1 2 "Clinical Urologists Group Supports Genomic Testing for Prostate Cancer". ClinicalOMICs. 6 March 2018. Retrieved 9 March 2018.
The Association, which represents nearly 4,000 member urologists nationwide, said in the one-page statement.... The AACU’s statement has won support from the Large Urology Group Practice Association (LUGPA), which represents more than 2,300 physicians who make up more than 25% of the nation’s practicing urologists.
- ↑ Heldwein, Flavio Lobo; Loeb, Stacy; Wroclawski, Marcelo Langer; et al. (2020-06-05). "A Systematic Review on Guidelines and Recommendations for Urology Standard of Care During the COVID-19 Pandemic". European Urology Focus. 6 (5): 1070–1085. doi:10.1016/j.euf.2020.05.020. ISSN 2405-4569. PMC 7274599. PMID 32532703.
19. https://nams.org.np/about.php 20. http://www.iom.edu.np/?page_id=21