Cardiology
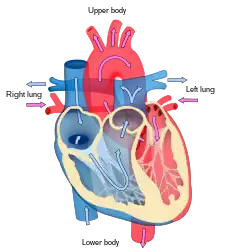 Blood flow diagram of the human heart. Blue components indicate de-oxygenated blood pathways and red components indicate oxygenated blood pathways. | |
| System | Cardiovascular |
|---|---|
| Subdivisions | Interventional, Nuclear |
| Significant diseases | Heart disease, Cardiovascular disease, Atherosclerosis, Cardiomyopathy, Hypertension (High Blood Pressure) |
| Significant tests | Blood tests, electrophysiology study, cardiac imaging, ECG, echocardiograms, stress test |
| Specialist | Cardiologist |
| Glossary | Glossary of medicine |
Cardiology (from Greek καρδίᾱ kardiā, "heart" and -λογία -logia, "study") is a branch of medicine that deals with the disorders of the heart as well as some parts of the circulatory system. The field includes medical diagnosis and treatment of congenital heart defects, coronary artery disease, heart failure, valvular heart disease and electrophysiology. Physicians who specialize in this field of medicine are called cardiologists, a specialty of internal medicine. Pediatric cardiologists are pediatricians who specialize in cardiology. Physicians who specialize in cardiac surgery are called cardiothoracic surgeons or cardiac surgeons, a specialty of general surgery.
Although the cardiovascular system is inextricably linked to blood, cardiology is relatively unconcerned with hematology and its diseases. Some obvious exceptions that affect the function of the heart would be blood tests (electrolyte disturbances, troponins), decreased oxygen carrying capacity (anemia, hypovolemic shock), and coagulopathies.
Specializations
All cardiologists study the disorders of the heart, but the study of adult and child heart disorders are through different training pathways. Therefore, an adult cardiologist (often simply called "cardiologist") is inadequately trained to take care of children, and pediatric cardiologists are not trained to take care of adult heart disease. The surgical aspects are not included in cardiology and are in the domain of cardiothoracic surgery. For example, coronary artery bypass surgery (CABG), cardiopulmonary bypass and valve replacement are surgical procedures performed by surgeons, not cardiologists. However the insertion of stents and pacemakers is performed by cardiologists
Adult cardiology
Cardiology is a specialty of internal medicine. To be a cardiologist in the United States, a three-year residency in internal medicine is followed by a three-year fellowship in cardiology. It is possible to specialize further in a sub-specialty. Recognized sub-specialties in the United States by the ACGME are cardiac electrophysiology, echocardiography, interventional cardiology, and nuclear cardiology. Recognized subspecialties in the United States by the American Osteopathic Association Bureau of Osteopathic Specialists (AOABOS) include clinical cardiac electrophysiology and interventional cardiology. [1] [2] While in India, a person needs to undergo three years of residency in General Medicine or Pediatrics after M.B.B.S and then three years of residency in Cardiology to be a D.M/Diplomate of National Board (DNB) in Cardiology.
Per doximity, adult cardiologists make an average of $436,849 in the United States.[3]
Cardiac electrophysiology
Cardiac electrophysiology is the science of elucidating, diagnosing, and treating the electrical activities of the heart. The term is usually used to describe studies of such phenomena by invasive (intracardiac) catheter recording of spontaneous activity as well as of cardiac responses to programmed electrical stimulation (PES). These studies are performed to assess complex arrhythmias, elucidate symptoms, evaluate abnormal electrocardiograms, assess risk of developing arrhythmias in the future, and design treatment. These procedures increasingly include therapeutic methods (typically radiofrequency ablation, or cryoablation) in addition to diagnostic and prognostic procedures. Other therapeutic modalities employed in this field include antiarrhythmic drug therapy and implantation of pacemakers and automatic implantable cardioverter-defibrillators (AICD).[4][5]
The cardiac electrophysiology study (EPS) typically measures the response of the injured or cardiomyopathic myocardium to PES on specific pharmacological regimens in order to assess the likelihood that the regimen will successfully prevent potentially fatal sustained ventricular tachycardia (VT) or ventricular fibrillation (VF) in the future. Sometimes a series of EPS drug trials must be conducted to enable the cardiologist to select the one regimen for long-term treatment that best prevents or slows the development of VT or VF following PES. Such studies may also be conducted in the presence of a newly implanted or newly replaced cardiac pacemaker or AICD.[4]
Clinical cardiac electrophysiology
Clinical cardiac electrophysiology is a branch of the medical specialty of cardiology and is concerned with the study and treatment of rhythm disorders of the heart. Cardiologists with expertise in this area are usually referred to as electrophysiologists. Electrophysiologists are trained in the mechanism, function, and performance of the electrical activities of the heart. Electrophysiologists work closely with other cardiologists and cardiac surgeons to assist or guide therapy for heart rhythm disturbances (arrhythmias). They are trained to perform interventional and surgical procedures to treat cardiac arrhythmia.
The training required to become an electrophysiologist is long and requires 7 to 8 years after medical school (within the U.S.). Three years of internal medicine residency, three years of Clinical Cardiology fellowship, and one to two (in most instances) years of clinical cardiac electrophysiology.
Cardiogeriatrics
Cardiogeriatrics, or geriatric cardiology, is the branch of cardiology and geriatric medicine that deals with the cardiovascular disorders in elderly people.
Cardiac disorders such as coronary heart disease, including myocardial infarction, heart failure, cardiomyopathy, and arrhythmias such as atrial fibrillation, are common and are a major cause of mortality in elderly people.[6] Vascular disorders such as atherosclerosis and peripheral arterial disease cause significant morbidity and mortality in aged people.[7][8]
Echocardiography
Echocardiography uses standard two-dimensional, three-dimensional, and Doppler ultrasound to create images of the heart.
Echocardiography has become routinely used in the diagnosis, management, and follow-up of patients with any suspected or known heart diseases. It is one of the most widely used diagnostic tests in cardiology. It can provide a wealth of helpful information, including the size and shape of the heart (internal chamber size quantification), pumping capacity, and the location and extent of any tissue damage. An echocardiogram can also give physicians other estimates of heart function, such as a calculation of the cardiac output, ejection fraction, and diastolic function (how well the heart relaxes).
Echocardiography can help detect cardiomyopathies, such as hypertrophic cardiomyopathy, dilated cardiomyopathy, and many others. The use of stress echocardiography may also help determine whether any chest pain or associated symptoms are related to heart disease. The biggest advantage to echocardiography is that it is not invasive (does not involve breaking the skin or entering body cavities) and has no known risks or side effects.
Interventional cardiology
Interventional cardiology is a branch of cardiology that deals specifically with the catheter based treatment of structural heart diseases. A large number of procedures can be performed on the heart by catheterization. This most commonly involves the insertion of a sheath into the femoral artery (but, in practice, any large peripheral artery or vein) and cannulating the heart under X-ray visualization (most commonly Fluoroscopy).
The main advantages of using the interventional cardiology or radiology approach are the avoidance of the scars and pain, and long post-operative recovery. Additionally, interventional cardiology procedure of primary angioplasty is now the gold standard of care for an acute Myocardial infarction. This procedure can also be done proactively, when areas of the vascular system become occluded from Atherosclerosis. The Cardiologist will thread this sheath through the vascular system to access the heart. This sheath has a balloon and a tiny wire mesh tube wrapped around it, and if the cardiologist finds a blockage or Stenosis, they can inflate the balloon at the occlusion site in the vascular system to flatten or compress the plaque against the vascular wall. Once that is complete a Stent is placed as a type of scaffold to hold the vasculature open permanently.
Preventive Cardiology and Cardiac Rehabilitation
In recent times, the focus is gradually shifting to Preventive cardiology due to increased Cardiovascular Disease burden at an early age. As per WHO, 37% of all premature deaths are due to cardiovascular diseases and out of this, 82% are in low and middle income countries.[9] Clinical cardiology is the sub specialty of Cardiology which looks after preventive cardiology and cardiac rehabilitation. Preventive cardiology also deals with routine preventive checkup though non invasive tests specifically Electrocardiography, Stress Tests, Lipid Profile and General Physical examination to detect any cardiovascular diseases at an early age while cardiac rehabilitation is the upcoming branch of cardiology which helps a person regain his overall strength and live a normal life after a cardiovascular event. A subspecialty of Preventive Cardiology is Sports Cardiology.
Children
Helen B. Taussig is known as the founder of pediatric cardiology. She became famous through her work with Tetralogy of Fallot, a congenital heart defect in which oxygenated and deoxygenated blood enters the circulatory system resulting from a ventricular septal defect (VSD) right beneath the aorta. This condition causes newborns to have a bluish-tint, cyanosis, and have a deficiency of oxygen to their tissues, hypoxemia. She worked with Alfred Blalock and Vivien Thomas at the Johns Hopkins Hospital where they experimented with dogs to look at how they would attempt to surgically cure these "blue babies." They eventually figured out how to do just that by the anastomosis of the systemic artery to the pulmonary artery and called this the Blalock-Taussig Shunt.[10]
Tetralogy of Fallot, pulmonary atresia, double outlet right ventricle, transposition of the great arteries, persistent truncus arteriosus, and Ebsteins anomaly are various congenital cyanotic heart diseases. Congenital cyanotic heart diseases is where something is wrong with the heart of a newborn and it is not oxygenating the blood efficiently.

Tetralogy of Fallot
Tetralogy of Fallot is the most common congenital heart disease arising in 1–3 cases per 1,000 births. The cause of this defect is a ventricular septal defect (VSD) and an overriding aorta. These two defects combined causes deoxygenated blood to bypass the lungs and going right back into the circulatory system. The modified Blalock-Taussig shunt is usually used to fix the circulation. This procedure is done by placing a graft between the subclavian artery and the ipsilateral pulmonary artery to restore the correct blood flow.
Pulmonary Atresia
Pulmonary Atresia happens in 7–8 per 100,000 births and is characterized by the aorta branching out of the right ventricle. This causes the deoxygenated blood to bypass the lungs and enter the circulatory system. Surgeries can fix this by redirecting the aorta and fixing the right ventricle and pulmonary artery connection.
There are two types of pulmonary atresia, classified by whether or not the baby also has a ventricular septal defect.[11][12]
- Pulmonary atresia with an intact ventricular septum: This type of pulmonary atresia is associated with complete and intact septum between the ventricles.[12]
- Pulmonary atresia with a ventricular septal defect: This type of pulmonary atresia happens when a ventricular septal defect allows blood to flow into and out of the right ventricle.[12]
Double Outlet Right Ventricle (DORV)
Double outlet right ventricle is when both great arteries, the pulmonary artery and the aorta, are connected to the right ventricle. There is usually a VSD in different particular places depending on the variations of DORV, typically 50% are subaortic and 30%. The surgeries that can be done to fix this defect can vary due to the different physiology and blood flow in the defected heart. One way it can be cured is by a VSD closure and placing conduits to restart the blood flow between the left ventricle and the aorta and between the right ventricle and the pulmonary artery. Another way is systemic-to-pulmonary artery shunt in cases associated with pulmonary stenosis. Also, a balloon atrial septostomy can be done to fix DORV with the Taussig-Bing anomaly.
Transposition of Great Arteries
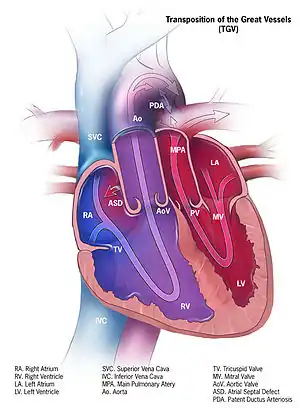
There are two different types of transposition of the great arteries, Dextro-transposition of the great arteries and Levo-transposition of the great arteries, depending on where the chambers and vessels connect. Dextro-transposition happens in about 1 in 4,000 newborns and is when the right ventricle pumps blood into the aorta and deoxygenated blood enters the blood stream. The temporary procedure is to create an atrial septal defect (ASD). A permanent fix is more complicated and involves redirecting the pulmonary return to the right atrium and the systemic return to the left atrium, which is known as the Senning procedure. The Rastelli procedure can also be done by rerouting the left ventricular outflow, dividing the pulmonary trunk, and placing a conduit in between the right ventricle and pulmonary trunk. Levo-transposition happens in about 1 in 13,000 newborns and is characterized by the left ventricle pumping blood into the lungs and the right ventricle pumping the blood into the aorta. This may not produce problems at the beginning, but will eventually due to the different pressures each ventricle uses to pump blood. Switching the left ventricle to be the systemic ventricle and the right ventricle to pump blood into the pulmonary artery can repair levo-transposition.
Persistent Truncus Arteriosis
Persistent truncus arteriosus is when the truncus arteriosus fails to split into the aorta and pulmonary trunk. This occurs in about 1 in 11,000 live births and allows both oxygenated and deoxygenated blood into the body. The repair consists of a VSD closure and the Rastelli procedure.
Ebstein Anomaly
Ebstein's anomaly is characterized by a right atrium that is significantly enlarged and a heart that is shaped like a box. This is very rare and happens in less than 1% of congenital heart disease cases. The surgical repair varies depending on the severity of the disease.[13]
Pediatric cardiology is a sub-specialty of pediatrics. To become a pediatric cardiologist in the United States, one must complete a three-year residency in pediatrics, followed by a three-year fellowship in pediatric cardiology. Per doximity, pediatric cardiologists make an average of $303,917 in the United States.[3]
The heart
As the center focus of cardiology, the heart has numerous anatomical features (e.g., atria, ventricles, heart valves) and numerous physiological features (e.g., systole, heart sounds, afterload) that have been encyclopedically documented for many centuries.
Disorders of the heart lead to heart disease and cardiovascular disease and can lead to a significant number of deaths: cardiovascular disease is the leading cause of death in the United States and caused 24.95% of total deaths in 2008.[14]
The primary responsibility of the heart is to pump blood throughout the body. It pumps blood from the body — called the systemic circulation — through the lungs — called the pulmonary circulation — and then back out to the body. This means that the heart is connected to and affects the entirety of the body. Simplified, the heart is a circuit of the Circulation. While plenty is known about the healthy heart, the bulk of study in cardiology is in disorders of the heart and restoration, and where possible, of function.
The heart is a muscle that squeezes blood and functions like a pump. Each part of the heart is susceptible to failure or dysfunction and the heart can be divided into the mechanical and the electrical parts.
The electrical part of the heart is centered on the periodic contraction (squeezing) of the muscle cells that is caused by the cardiac pacemaker located in the sinoatrial node. The study of the electrical aspects is a sub-field of electrophysiology called cardiac electrophysiology and is epitomized with the electrocardiogram (ECG/EKG). The action potentials generated in the pacemaker propagate throughout the heart in a specific pattern. The system that carries this potential is called the electrical conduction system. Dysfunction of the electrical system manifests in many ways and may include Wolff–Parkinson–White syndrome, ventricular fibrillation, and heart block.
The mechanical part of the heart is centered on the fluidic movement of blood and the functionality of the heart as a pump. The mechanical part is ultimately the purpose of the heart and many of the disorders of the heart disrupt the ability to move blood. Failure to move sufficient blood can result in failure in other organs and may result in death if severe. Heart failure is one condition in which the mechanical properties of the heart have failed or are failing, which means insufficient blood is being circulated.
Coronary circulation
Coronary circulation is the circulation of blood in the blood vessels of the heart muscle (myocardium). The vessels that deliver oxygen-rich blood to the myocardium are known as coronary arteries. The vessels that remove the deoxygenated blood from the heart muscle are known as cardiac veins. These include the great cardiac vein, the middle cardiac vein, the small cardiac vein and the anterior cardiac veins.
As the left and right coronary arteries run on the surface of the heart, they can be called epicardial coronary arteries. These arteries, when healthy, are capable of autoregulation to maintain coronary blood flow at levels appropriate to the needs of the heart muscle. These relatively narrow vessels are commonly affected by atherosclerosis and can become blocked, causing angina or a heart attack. (See also: circulatory system.) The coronary arteries that run deep within the myocardium are referred to as subendocardial.
The coronary arteries are classified as "end circulation", since they represent the only source of blood supply to the myocardium; there is very little redundant blood supply, which is why blockage of these vessels can be so critical.
Cardiac examination
The cardiac examination (also called the "precordial exam"), is performed as part of a physical examination, or when a patient presents with chest pain suggestive of a cardiovascular pathology. It would typically be modified depending on the indication and integrated with other examinations especially the respiratory examination.
Like all medical examinations, the cardiac examination follows the standard structure of inspection, palpation and auscultation.
Heart disorders
Cardiology is concerned with the normal functionality of the heart and the deviation from a healthy heart. Many disorders involve the heart itself but some are outside of the heart and in the vascular system. Collectively, the two together are termed the cardiovascular system and diseases of one part tend to affect the other.
Hypertension
Hypertension, also known as "high blood pressure"", is a long term medical condition in which the blood pressure in the arteries is persistently elevated.[16] High blood pressure usually does not cause symptoms.[17] Long term high blood pressure, however, is a major risk factor for coronary artery disease, stroke, heart failure, peripheral vascular disease, vision loss, and chronic kidney disease.[18][19]
Lifestyle factors can increase the risk of hypertension. These include excess salt in the diet, excess body weight, smoking, and alcohol.[17][20] Hypertension can also be caused by other diseases, or as a side-effect of drugs.
Blood pressure is expressed by two measurements, the systolic and diastolic pressures, which are the maximum and minimum pressures, respectively.[17] Normal blood pressure at rest is within the range of 100–140 millimeters mercury (mmHg) systolic and 60–90 mmHg diastolic.[21] High blood pressure is present if the resting blood pressure is persistently at or above 140/90 mmHg for most adults.[20] Different numbers apply to children.[22] Ambulatory blood pressure monitoring over a 24-hour period appears more accurate than office best blood pressure measurement.[16][20]
Lifestyle changes and medications can lower blood pressure and decrease the risk of health complications.[23] Lifestyle changes include weight loss, decreased salt intake, physical exercise, and a healthy diet.[20] If lifestyle changes are not sufficient then blood pressure medications are used.[23] Up to three medications can control blood pressure in 90% of people.[20] The treatment of moderate to severe high arterial blood pressure (defined as >160/100 mmHg) with medications is associated with an improved life expectancy and reduced morbidity.[24] The effect of treatment of blood pressure between 140/90 mmHg and 160/100 mmHg is less clear, with some reviews finding benefit[25][26] and others finding a lack of evidence for benefit.[27] High blood pressure affects between 16 and 37% of the population globally.[20] In 2010 hypertension was believed to have been a factor in 18% (9.4 million) deaths.[28]
Essential vs Secondary hypertension
Essential hypertension is the form of hypertension that by definition has no identifiable cause. It is the most common type of hypertension, affecting 95% of hypertensive patients,[29][30][31][32] it tends to be familial and is likely to be the consequence of an interaction between environmental and genetic factors. Prevalence of essential hypertension increases with age, and individuals with relatively high blood pressure at younger ages are at increased risk for the subsequent development of hypertension. Hypertension can increase the risk of cerebral, cardiac, and renal events.[33]
Secondary hypertension is a type of hypertension which is caused by an identifiable underlying secondary cause. It is much less common than essential hypertension, affecting only 5% of hypertensive patients. It has many different causes including endocrine diseases, kidney diseases, and tumors. It also can be a side effect of many medications.
Complications of hypertension
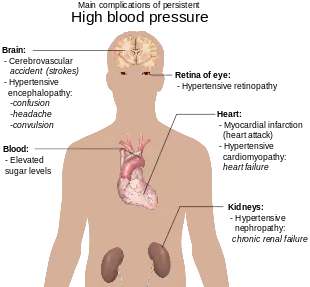
Complications of hypertension are clinical outcomes that result from persistent elevation of blood pressure.[34] Hypertension is a risk factor for all clinical manifestations of atherosclerosis since it is a risk factor for atherosclerosis itself.[35][36][37][38][39] It is an independent predisposing factor for heart failure,[40][41] coronary artery disease,[42][43] stroke,[34] renal disease,[44][45][46] and peripheral arterial disease.[47][48] It is the most important risk factor for cardiovascular morbidity and mortality, in industrialized countries.[49]
Cardiac arrhythmia
Cardiac arrhythmia, also known as "cardiac dysrhythmia" or "irregular heartbeat", is a group of conditions in which the heartbeat is irregular, too fast, or too slow. A heart rate that is too fast – above 100 beats per minute in adults – is called tachycardia and a heart rate that is too slow – below 60 beats per minute – is called bradycardia.[50] Many types of arrhythmia have no symptoms. When symptoms are present these may include palpitations or feeling a pause between heartbeats. More seriously there may be lightheadedness, passing out, shortness of breath, or chest pain.[51] While most types of arrhythmia are not serious, some predispose a person to complications such as stroke or heart failure.[50][52] Others may result in cardiac arrest.[52]
There are four main types of arrhythmia: extra beats, supraventricular tachycardias, ventricular arrhythmias, and bradyarrhythmias. Extra beats include premature atrial contractions, premature ventricular contractions, and premature junctional contractions. Supraventricular tachycardias include atrial fibrillation, atrial flutter, and paroxysmal supraventricular tachycardia. Ventricular arrhythmias include ventricular fibrillation and ventricular tachycardia.[52][53] Arrhythmias are due to problems with the electrical conduction system of the heart.[50] Arrhythmias may occur in children; however, the normal range for the heart rate is different and depends on age.[52] A number of tests can help with diagnosis including an electrocardiogram (ECG) and Holter monitor.[54]
Most arrhythmias can be effectively treated.[50] Treatments may include medications, medical procedures such as a pacemaker, and surgery. Medications for a fast heart rate may include beta blockers or agents that attempt to restore a normal heart rhythm such as procainamide. This later group may have more significant side effects especially if taken for a long period of time. Pacemakers are often used for slow heart rates. Those with an irregular heartbeat are often treated with blood thinners to reduce the risk of complications. Those who have severe symptoms from an arrhythmia may receive urgent treatment with a jolt of electricity in the form of cardioversion or defibrillation.[55]
Arrhythmia affects millions of people.[56] In Europe and North America, as of 2014, atrial fibrillation affects about 2% to 3% of the population.[57] Atrial fibrillation and atrial flutter resulted in 112,000 deaths in 2013, up from 29,000 in 1990.[58] Sudden cardiac death is the cause of about half of deaths due to cardiovascular disease or about 15% of all deaths globally.[59] About 80% of sudden cardiac death is the result of ventricular arrhythmias.[59] Arrhythmias may occur at any age but are more common among older people.[56]
Coronary artery disease
Coronary artery disease, also known as "ischemic heart disease",[60] is a group of diseases that includes: stable angina, unstable angina, myocardial infarction, and sudden cardiac death.[61] It is within the group of cardiovascular diseases of which it is the most common type.[62] A common symptom is chest pain or discomfort which may travel into the shoulder, arm, back, neck, or jaw.[63] Occasionally it may feel like heartburn. Usually symptoms occur with exercise or emotional stress, last less than a few minutes, and get better with rest.[63] Shortness of breath may also occur and sometimes no symptoms are present.[63] The first sign is occasionally a heart attack.[64] Other complications include heart failure or an irregular heartbeat.[64]
Risk factors include: high blood pressure, smoking, diabetes, lack of exercise, obesity, high blood cholesterol, poor diet, and excessive alcohol, among others.[65][66] Other risks include depression.[67] The underlying mechanism involves atherosclerosis of the arteries of the heart. A number of tests may help with diagnoses including: electrocardiogram, cardiac stress testing, coronary computed tomographic angiography, and coronary angiogram, among others.[68]
Prevention is by eating a healthy diet, regular exercise, maintaining a healthy weight and not smoking.[69] Sometimes medication for diabetes, high cholesterol, or high blood pressure are also used.[69] There is limited evidence for screening people who are at low risk and do not have symptoms.[70] Treatment involves the same measures as prevention.[71][72] Additional medications such as antiplatelets including aspirin, beta blockers, or nitroglycerin may be recommended.[72] Procedures such as percutaneous coronary intervention (PCI) or coronary artery bypass surgery (CABG) may be used in severe disease.[72][73] In those with stable CAD it is unclear if PCI or CABG in addition to the other treatments improve life expectancy or decreases heart attack risk.[74]
In 2013 CAD was the most common cause of death globally, resulting in 8.14 million deaths (16.8%) up from 5.74 million deaths (12%) in 1990.[62] The risk of death from CAD for a given age has decreased between 1980 and 2010 especially in developed countries.[75] The number of cases of CAD for a given age has also decreased between 1990 and 2010.[76] In the United States in 2010 about 20% of those over 65 had CAD, while it was present in 7% of those 45 to 64, and 1.3% of those 18 to 45.[77] Rates are higher among men than women of a given age.[77]
Cardiac arrest
Cardiac arrest is a sudden stop in effective blood flow due to the failure of the heart to contract effectively.[78] Symptoms include loss of consciousness and abnormal or absent breathing.[79][80] Some people may have chest pain, shortness of breath, or nausea before this occurs.[80] If not treated within minutes, death usually occurs.[78]
The most common cause of cardiac arrest is coronary artery disease. Less common causes include major blood loss, lack of oxygen, very low potassium, heart failure, and intense physical exercise. A number of inherited disorders may also increase the risk including long QT syndrome. The initial heart rhythm is most often ventricular fibrillation.[81] The diagnosis is confirmed by finding no pulse.[79] While a cardiac arrest may be caused by heart attack or heart failure these are not the same.[78]
Prevention includes not smoking, physical activity, and maintaining a healthy weight.[82] Treatment for cardiac arrest is immediate cardiopulmonary resuscitation (CPR) and, if a shockable rhythm is present, defibrillation.[83] Among those who survive targeted temperature management may improve outcomes.[84] An implantable cardiac defibrillator may be placed to reduce the chance of death from recurrence.[82]
In the United States, cardiac arrest outside of hospital occurs in about 13 per 10,000 people per year (326,000 cases). In hospital cardiac arrest occurs in an additional 209,000[85] Cardiac arrest becomes more common with age. It affects males more often than females.[86] The percentage of people who survive with treatment is about 8%. Many who survive have significant disability. Many U.S. television shows, however, have portrayed unrealistically high survival rates of 67%.[87]
Congenital heart defects
A congenital heart defect, also known as a "congenital heart anomaly" or "congenital heart disease", is a problem in the structure of the heart that is present at birth.[88] Signs and symptoms depend on the specific type of problem.[89] Symptoms can vary from none to life-threatening.[88] When present they may include rapid breathing, bluish skin, poor weight gain, and feeling tired.[90] It does not cause chest pain.[90] Most congenital heart problems do not occur with other diseases.[89] Complications that can result from heart defects include heart failure.[90]
The cause of a congenital heart defect is often unknown.[91] Certain cases may be due to infections during pregnancy such as rubella, use of certain medications or drugs such as alcohol or tobacco, parents being closely related, or poor nutritional status or obesity in the mother.[89][92] Having a parent with a congenital heart defect is also a risk factor.[93] A number of genetic conditions are associated with heart defects including Down syndrome, Turner syndrome, and Marfan syndrome.[89] Congenital heart defects are divided into two main groups: cyanotic heart defects and non-cyanotic heart defects, depending on whether the child has the potential to turn bluish in color.[89] The problems may involve the interior walls of the heart, the heart valves, or the large blood vessels that lead to and from the heart.[88]
Congenital heart defects are partly preventable through rubella vaccination, the adding of iodine to salt, and the adding of folic acid to certain food products.[89] Some defects do not need treatment.[88] Other may be effectively treated with catheter based procedures or heart surgery.[94] Occasionally a number of operations may be needed.[94] Occasionally heart transplantation is required.[94] With appropriate treatment outcomes, even with complex problems, are generally good.[88]
Heart defects are the most common birth defect.[89][95] In 2013 they were present in 34.3 million people globally.[95] They affect between 4 and 75 per 1,000 live births depending upon how they are diagnosed.[89][93] About 6 to 19 per 1,000 cause a moderate to severe degree of problems.[93] Congenital heart defects are the leading cause of birth defect-related deaths.[89] In 2013 they resulted in 323,000 deaths down from 366,000 deaths in 1990.[96]
Diagnostic tests in cardiology
Diagnostic tests in cardiology are the methods of identifying heart conditions associated with healthy vs. unhealthy, pathologic heart function. The starting point is obtaining a medical history, followed by Auscultation. Then blood tests, electrophysiological procedures, and cardiac imaging can be ordered for further analysis. Electrophysiological procedures include electrocardiogram, cardiac monitoring, cardiac stress testing, and the electrophysiology study.
Also, HeartScore exists
Cardiology community
Associations
- American College of Cardiology
- American Heart Association
- European Society of Cardiology
- Heart Rhythm Society
- Canadian Cardiovascular Society
- Indian Heart Association
- National Heart Foundation of Australia
- Cardiology Society of India
Journals
- Acta Cardiologica
- American Journal of Cardiology
- Annals of Cardiac Anaesthesia
- Current Research: Cardiology
- Cardiology in Review
- Circulation
- Circulation Research
- Clinical and Experimental Hypertension
- Clinical Cardiology
- EP – Europace
- European Heart Journal
- Heart
- Heart Rhythm
- International Journal of Cardiology
- Journal of the American College of Cardiology
- Pacing and Clinical Electrophysiology
- Indian Heart Journal
Cardiologists
| Occupation | |
|---|---|
| Names | Doctor, Medical Specialist |
Occupation type | Specialty |
Activity sectors | Medicine |
| Specialty | UnlinkedWikibase error: ⧼unlinkedwikibase-error-statements-entity-not-set⧽ |
| Description | |
Education required |
|
Fields of employment | Hospitals, Clinics |
- Robert Atkins (1930–2003), known for the Atkins diet
- Eugene Braunwald (born 1929), editor of Braunwald's Heart Disease and 1000+ publications
- Wallace Brigden (1916–2008), identified cardiomyopathy
- Willem Einthoven (1860–1927), a physiologist who built the first practical ECG and won the 1924 Nobel Prize in Physiology or Medicine ("for the discovery of the mechanism of the electrocardiogram")
- Werner Forssmann (1904–1979), who infamously performed the first human catheterization on himself that led to him being let go from Berliner Charité Hospital, quitting cardiology as a speciality, and then winning the 1956 Nobel Prize in Physiology or Medicine ("for their discoveries concerning heart catheterization and pathological changes in the circulatory system")
- Andreas Gruentzig (1939–1985), first developed balloon angioplasty
- William Harvey (1578–1657), wrote Exercitatio Anatomica de Motu Cordis et Sanguinis in Animalibus that first described the closed circulatory system and whom Forssmann described as founding cardiology in his Nobel lecture
- Murray S. Hoffman (born 1924) As president of the Colorado Heart Association, he initiated one of the first jogging programs promoting cardiac health
- Max Holzmann (1899–1994), co-founder of the Swiss Society of Cardiology, president from 1952–1955
- Samuel A. Levine (1891–1966), recognized the sign known as Levine's sign as well as the current grading of the intensity of heart murmurs, known as the Levine scale
- Henry Joseph Llewellyn "Barney" Marriott (1917–2007), ECG interpretation and Practical Electrocardiography[97]
- Bernard Lown (born 1921), original developer of the defibrillator
- Woldemar Mobitz (1889–1951), described and classified the two types of second-degree atrioventricular block often called "Mobitz Type I" and "Mobitz Type II"
- Jacqueline Noonan (born 1928), discoverer of Noonan syndrome that is the top syndromic cause of congenital heart disease
- John Parkinson (1885–1976), known for Wolff–Parkinson–White syndrome
- Helen B. Taussig (1898–1986), founder of pediatric cardiology and extensively worked on blue baby syndrome
- Paul Dudley White (1886–1973), known for Wolff–Parkinson–White syndrome
- Louis Wolff (1898–1972), known for Wolff–Parkinson–White syndrome
- Karel Frederik Wenckebach (1864–1940), first described what is now called type I second-degree atrioventricular block in 1898
See also
References
- ↑ "Cardiologists in Delhi NCR". Full Details Information. 26 March 2019. Archived from the original on 29 September 2020. Retrieved 13 July 2020.
- ↑ "Specialties & Subspecialties". American Osteopathic Association. Archived from the original on 2015-08-13. Retrieved 23 September 2012.
- 1 2 Hamblin, James (January 27, 2015) What Doctors Make Archived 2017-11-17 at the Wayback Machine. theatlantic.com
- 1 2 Fauci, Anthony, et al. Harrison's Textbook of Medicine. New York: McGraw Hill, 2009.
- ↑ Braunwald, Eugene, ed. Heart Disease, 6th edition. Philadelphia: Saunders, 2011.
- ↑ "Trends in Causes of Death among Older Persons in the United States" (PDF). Archived (PDF) from the original on 2017-11-13.
- ↑ Golomb Beatrice A.; Dang Tram T.; Criqui Michael H. (2006-08-15). "Peripheral Arterial Disease". Circulation. 114 (7): 688–699. doi:10.1161/CIRCULATIONAHA.105.593442. PMID 16908785.
- ↑ Yazdanyar, Ali; Newman, Anne B. (2010-11-01). "The Burden of Cardiovascular Disease in the Elderly: Morbidity, Mortality, and Costs". Clinics in Geriatric Medicine. 25 (4): 563–vii. doi:10.1016/j.cger.2009.07.007. ISSN 0749-0690. PMC 2797320. PMID 19944261.
- ↑ "Cardiovascular diseases (CVDs)". www.who.int. Archived from the original on 2021-09-07. Retrieved 2019-05-14.
- ↑ Murphy, Anne M. (2008-07-16). "The Blalock-Taussig-Thomas Collaboration". JAMA. 300 (3): 328–30. doi:10.1001/jama.300.3.328. ISSN 0098-7484. PMID 18632547.
- ↑ Ramaswamy P, Webber HS. "Ventricular Septal Defects: Background, Anatomy, Pathophysiology". Medscape. WebMD LLC. Archived from the original on August 22, 2017. Retrieved August 22, 2017.
- 1 2 3 "Facts about Pulmonary Atresia: Types of Pulmonary Atresia". CDC. USA.gov. Archived from the original on June 26, 2018. Retrieved August 22, 2017.
- ↑ Bhat, Venkatraman (2016). "Illustrated Imaging Essay on Congenital Heart Diseases: Multimodality Approach Part III: Cyanotic Heart Diseases and Complex Congenital Anomalies". Journal of Clinical and Diagnostic Research. 10 (7): TE01–10. doi:10.7860/jcdr/2016/21443.8210. PMC 5020285. PMID 27630924.
- ↑ Pagidipati, Neha Jadeja; Gaziano, Thomas A. (2013). "Estimating Deaths From Cardiovascular Disease: A Review of Global Methodologies of Mortality Measurement". Circulation. 127 (6): 749–756. doi:10.1161/CIRCULATIONAHA.112.128413. ISSN 0009-7322. PMC 3712514. PMID 23401116.
- ↑ "Cardiologists in Delhi NCR". Full Details Information. 26 March 2019. Archived from the original on 29 September 2020. Retrieved 13 July 2020.
- 1 2 Naish, Jeannette; Court, Denise Syndercombe (2014). Medical sciences (2 ed.). p. 562. ISBN 9780702052491. Archived from the original on 2020-07-27. Retrieved 2020-07-13.
- 1 2 3 "High Blood Pressure Fact Sheet". CDC. February 19, 2015. Archived from the original on 6 March 2016. Retrieved 6 March 2016.
- ↑ Lackland, DT; Weber, MA (May 2015). "Global burden of cardiovascular disease and stroke: hypertension at the core". The Canadian Journal of Cardiology. 31 (5): 569–71. doi:10.1016/j.cjca.2015.01.009. PMID 25795106.
- ↑ Mendis, Shanthi; Puska, Pekka; Norrving, Bo (2011). Global atlas on cardiovascular disease prevention and control (PDF) (1st ed.). Geneva: World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. p. 38. ISBN 9789241564373. Archived (PDF) from the original on 2014-08-17. Retrieved 2020-07-13.
- 1 2 3 4 5 6 Poulter, NR; Prabhakaran, D; Caulfield, M (22 August 2015). "Hypertension". Lancet. 386 (9995): 801–12. doi:10.1016/s0140-6736(14)61468-9. PMID 25832858.
- ↑ Giuseppe, Mancia; Fagard, R; Narkiewicz, K; Redon, J; Zanchetti, A; Bohm, M; Christiaens, T; Cifkova, R; De Backer, G; Dominiczak, A; Galderisi, M; Grobbee, DE; Jaarsma, T; Kirchhof, P; Kjeldsen, SE; Laurent, S; Manolis, AJ; Nilsson, PM; Ruilope, LM; Schmieder, RE; Sirnes, PA; Sleight, P; Viigimaa, M; Waeber, B; Zannad, F; Redon, J; Dominiczak, A; Narkiewicz, K; Nilsson, PM; et al. (July 2013). "2013 ESH/ESC Guidelines for the management of arterial hypertension: The Task Force for the management of arterial hypertension of the European Society of Hypertension (ESH) and of the European Society of Cardiology (ESC)" (PDF). European Heart Journal. 34 (28): 2159–219. doi:10.1093/eurheartj/eht151. hdl:1854/LU-4127523. PMID 23771844. Archived (PDF) from the original on 2021-08-28. Retrieved 2020-07-13.
- ↑ James, PA.; Oparil, S.; Carter, BL.; Cushman, WC.; Dennison-Himmelfarb, C.; Handler, J.; Lackland, DT.; Lefevre, ML.; et al. (Dec 2013). "2014 Evidence-Based Guideline for the Management of High Blood Pressure in Adults: Report From the Panel Members Appointed to the Eighth Joint National Committee (JNC 8)". JAMA. 311 (5): 507–20. doi:10.1001/jama.2013.284427. PMID 24352797.
- 1 2 "How Is High Blood Pressure Treated?". National Heart, Lung, and Blood Institute. September 10, 2015. Archived from the original on 6 April 2016. Retrieved 6 March 2016.
- ↑ Musini, Vijaya M; Tejani, Aaron M; Bassett, Ken; Puil, Lorri; Wright, James M (2019-06-05). Cochrane Hypertension Group (ed.). "Pharmacotherapy for hypertension in adults 60 years or older". Cochrane Database of Systematic Reviews. 6: CD000028. doi:10.1002/14651858.CD000028.pub3. PMC 6550717. PMID 31167038.
- ↑ Sundström, Johan; Arima, Hisatomi; Jackson, Rod; Turnbull, Fiona; Rahimi, Kazem; Chalmers, John; Woodward, Mark; Neal, Bruce (February 2015). "Effects of Blood Pressure Reduction in Mild Hypertension". Annals of Internal Medicine. 162 (3): 184–91. doi:10.7326/M14-0773. PMID 25531552.
- ↑ Xie, X; Atkins, E; Lv, J; Bennett, A; Neal, B; Ninomiya, T; Woodward, M; MacMahon, S; Turnbull, F; Hillis, GS; Chalmers, J; Mant, J; Salam, A; Rahimi, K; Perkovic, V; Rodgers, A (30 January 2016). "Effects of intensive blood pressure lowering on cardiovascular and renal outcomes: updated systematic review and meta-analysis". Lancet. 387 (10017): 435–43. doi:10.1016/S0140-6736(15)00805-3. PMID 26559744. Archived from the original on 16 April 2019. Retrieved 13 July 2020.
- ↑ Diao, D; Wright, JM; Cundiff, DK; Gueyffier, F (Aug 15, 2012). "Pharmacotherapy for mild hypertension". The Cochrane Database of Systematic Reviews. 8 (8): CD006742. doi:10.1002/14651858.CD006742.pub2. PMID 22895954. Archived from the original on July 29, 2020. Retrieved July 13, 2020.
- ↑ Campbell, NR; Lackland, DT; Lisheng, L; Niebylski, ML; Nilsson, PM; Zhang, XH (March 2015). "Using the Global Burden of Disease study to assist development of nation-specific fact sheets to promote prevention and control of hypertension and reduction in dietary salt: a resource from the World Hypertension League". Journal of Clinical Hypertension. 17 (3): 165–67. doi:10.1111/jch.12479. PMID 25644474.
- ↑ Carretero OA, Oparil S (January 2000). "Essential hypertension. Part I: definition and etiology". Circulation. 101 (3): 329–35. doi:10.1161/01.CIR.101.3.329. PMID 10645931. Archived from the original on 2012-07-07. Retrieved 2009-06-05.
- ↑ Oparil S, Zaman MA, Calhoun DA (November 2003). "Pathogenesis of hypertension". Ann. Intern. Med. 139 (9): 761–76. doi:10.7326/0003-4819-139-9-200311040-00011. PMID 14597461.
- ↑ Hall, John E.; Guyton, Arthur C. (2006). Textbook of medical physiology. St. Louis, Mo: Elsevier Saunders. p. 228. ISBN 978-0-7216-0240-0.
- ↑ "Hypertension: eMedicine Nephrology". Archived from the original on 2019-08-01. Retrieved 2009-06-05.
- ↑ "Essential hypertension : The Lancet". Archived from the original on 2013-06-01. Retrieved 2009-06-01.
{{cite journal}}: Cite journal requires|journal=(help) - 1 2 White WB (May 2009). "Defining the problem of treating the patient with hypertension and arthritis pain". The American Journal of Medicine. 122 (5 Suppl): S3–9. doi:10.1016/j.amjmed.2009.03.002. PMID 19393824.
- ↑ Insull W (January 2009). "The pathology of atherosclerosis: plaque development and plaque responses to medical treatment". The American Journal of Medicine. 122 (1 Suppl): S3–S14. doi:10.1016/j.amjmed.2008.10.013. PMID 19110086.
- ↑ Liapis CD, Avgerinos ED, Kadoglou NP, Kakisis JD (May 2009). "What a vascular surgeon should know and do about atherosclerotic risk factors". Journal of Vascular Surgery. 49 (5): 1348–54. doi:10.1016/j.jvs.2008.12.046. PMID 19394559.
- ↑ Riccioni G (2009). "The effect of antihypertensive drugs on carotid intima media thickness: an up-to-date review". Current Medicinal Chemistry. 16 (8): 988–96. doi:10.2174/092986709787581923. PMID 19275607. Archived from the original on 2013-01-12. Retrieved 2009-06-20.
- ↑ Safar ME, Jankowski P (February 2009). "Central blood pressure and hypertension: role in cardiovascular risk assessment". Clinical Science. 116 (4): 273–82. doi:10.1042/CS20080072. PMID 19138169.
- ↑ Werner CM, Böhm M (June 2008). "The therapeutic role of RAS blockade in chronic heart failure". Therapeutic Advances in Cardiovascular Disease. 2 (3): 167–77. doi:10.1177/1753944708091777. PMID 19124420.
- ↑ Gaddam KK, Verma A, Thompson M, Amin R, Ventura H (May 2009). "Hypertension and cardiac failure in its various forms". The Medical Clinics of North America. 93 (3): 665–80. doi:10.1016/j.mcna.2009.02.005. PMID 19427498. Archived from the original on 2020-03-28. Retrieved 2009-06-20.
- ↑ Reisin E, Jack AV (May 2009). "Obesity and hypertension: mechanisms, cardio-renal consequences, and therapeutic approaches". The Medical Clinics of North America. 93 (3): 733–51. doi:10.1016/j.mcna.2009.02.010. PMID 19427502. Archived from the original on 2020-03-28. Retrieved 2009-06-20.
- ↑ Agabiti-Rosei E (September 2008). "From macro- to microcirculation: benefits in hypertension and diabetes". Journal of Hypertension Supplement. 26 (3): S15–9. doi:10.1097/01.hjh.0000334602.71005.52. PMID 19363848.
- ↑ Murphy BP, Stanton T, Dunn FG (May 2009). "Hypertension and myocardial ischemia". The Medical Clinics of North America. 93 (3): 681–95. doi:10.1016/j.mcna.2009.02.003. PMID 19427499. Archived from the original on 2020-03-28. Retrieved 2009-06-20.
- ↑ Tylicki L, Rutkowski B (February 2003). "[Hypertensive nephropathy: pathogenesis, diagnosis and treatment]". Polski Merkuriusz Lekarski : Organ Polskiego Towarzystwa Lekarskiego (in Polish). 14 (80): 168–73. PMID 12728683.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Truong LD, Shen SS, Park MH, Krishnan B (February 2009). "Diagnosing nonneoplastic lesions in nephrectomy specimens". Archives of Pathology & Laboratory Medicine. 133 (2): 189–200. doi:10.1043/1543-2165-133.2.189 (inactive 2020-03-08). PMID 19195963. Archived from the original on 2022-02-08. Retrieved 2009-06-20.
{{cite journal}}: CS1 maint: DOI inactive as of March 2020 (link) - ↑ Tracy RE, White S (February 2002). "A method for quantifying adrenocortical nodular hyperplasia at autopsy: some use of the method in illuminating hypertension and atherosclerosis". Annals of Diagnostic Pathology. 6 (1): 20–9. doi:10.1053/adpa.2002.30606. PMID 11842376.
- ↑ Aronow WS (August 2008). "Hypertension and the older diabetic". Clinics in Geriatric Medicine. 24 (3): 489–501, vi–vii. doi:10.1016/j.cger.2008.03.001. PMID 18672184. Archived from the original on 2020-03-28. Retrieved 2009-06-20.
- ↑ Gardner AW, Afaq A (2008). "Management of Lower Extremity Peripheral Arterial Disease". Journal of Cardiopulmonary Rehabilitation and Prevention. 28 (6): 349–57. doi:10.1097/HCR.0b013e31818c3b96. PMC 2743684. PMID 19008688.
- ↑ Novo S, Lunetta M, Evola S, Novo G (January 2009). "Role of ARBs in the blood hypertension therapy and prevention of cardiovascular events". Current Drug Targets. 10 (1): 20–5. doi:10.2174/138945009787122897. PMID 19149532. Archived from the original on 2013-01-12. Retrieved 2009-06-20.
- 1 2 3 4 "What Is Arrhythmia?". www.nhlbi.nih.gov. July 1, 2011. Archived from the original on 2 March 2015. Retrieved 7 March 2015.
- ↑ "What Are the Signs and Symptoms of an Arrhythmia?". www.nhlbi.nih.gov. July 1, 2011. Archived from the original on 19 February 2015. Retrieved 7 March 2015.
- 1 2 3 4 "Types of Arrhythmia". www.nhlbi.nih.gov. July 1, 2011. Archived from the original on 7 June 2015. Retrieved 7 March 2015.
- ↑ Martin, C; Matthews, G; Huang, CL (2012). "Sudden cardiac death and Inherited channelopathy: the basic electrophysiology of the myocyte and myocardium in ion channel disease". Heart. 98 (7): 536–543. doi:10.1136/heartjnl-2011-300953. PMC 3308472. PMID 22422742.
- ↑ "How Are Arrhythmias Diagnosed?". www.nhlbi.nih.gov/. July 1, 2011. Archived from the original on 18 February 2015. Retrieved 7 March 2015.
- ↑ "How Are Arrhythmias Treated?". www.nhlbi.nih.gov/. July 1, 2011. Archived from the original on 17 February 2015. Retrieved 7 March 2015.
- 1 2 "Who Is at Risk for an Arrhythmia?". www.nhlbi.nih.gov/. July 1, 2011. Archived from the original on 3 March 2015. Retrieved 7 March 2015.
- ↑ Zoni-Berisso, M; Lercari, F; Carazza, T; Domenicucci, S (2014). "Epidemiology of atrial fibrillation: European perspective". Clinical Epidemiology. 6: 213–20. doi:10.2147/CLEP.S47385. PMC 4064952. PMID 24966695.
- ↑ GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–171. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- 1 2 Mehra, R (2007). "Global public health problem of sudden cardiac death". Journal of Electrocardiology. 40 (6 Suppl): S118–22. doi:10.1016/j.jelectrocard.2007.06.023. PMID 17993308.
- ↑ Bhatia, Sujata K. (2010). Biomaterials for clinical applications (Online-Ausg. ed.). New York: Springer. p. 23. ISBN 9781441969200. Archived from the original on 2020-07-27. Retrieved 2020-07-13.
- ↑ Wong, ND (May 2014). "Epidemiological studies of CHD and the evolution of preventive cardiology". Nature Reviews. Cardiology. 11 (5): 276–89. doi:10.1038/nrcardio.2014.26. PMID 24663092.
- 1 2 GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–171. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- 1 2 3 "What Are the Signs and Symptoms of Coronary Heart Disease?". 29 September 2014. Archived from the original on 24 February 2015. Retrieved 23 February 2015.
- 1 2 "Coronary Artery Disease (CAD)". 12 March 2013. Archived from the original on 2 March 2015. Retrieved 23 February 2015.
- ↑ Mehta, PK; Wei, J; Wenger, NK (16 October 2014). "Ischemic heart disease in women: A focus on risk factors". Trends in Cardiovascular Medicine. 25 (2): 140–151. doi:10.1016/j.tcm.2014.10.005. PMC 4336825. PMID 25453985.
- ↑ Mendis, Shanthi; Puska, Pekka; Norrving, Bo (2011). Global atlas on cardiovascular disease prevention and control (PDF) (1st ed.). Geneva: World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. pp. 3–18. ISBN 9789241564373. Archived (PDF) from the original on 2014-08-17. Retrieved 2020-07-13.
- ↑ Charlson, FJ; Moran, AE; Freedman, G; Norman, RE; Stapelberg, NJ; Baxter, AJ; Vos, T; Whiteford, HA (26 November 2013). "The contribution of major depression to the global burden of ischemic heart disease: a comparative risk assessment". BMC Medicine. 11: 250. doi:10.1186/1741-7015-11-250. PMC 4222499. PMID 24274053.
- ↑ "How Is Coronary Heart Disease Diagnosed?". 29 September 2014. Archived from the original on 24 February 2015. Retrieved 25 February 2015.
- 1 2 "How Can Coronary Heart Disease Be Prevented or Delayed?". Archived from the original on 24 February 2015. Retrieved 25 February 2015.
- ↑ Desai, CS; Blumenthal, RS; Greenland, P (April 2014). "Screening low-risk individuals for coronary artery disease". Current Atherosclerosis Reports. 16 (4): 402. doi:10.1007/s11883-014-0402-8. PMID 24522859.
- ↑ Boden, WE; Franklin, B; Berra, K; Haskell, WL; Calfas, KJ; Zimmerman, FH; Wenger, NK (October 2014). "Exercise as a therapeutic intervention in patients with stable ischemic heart disease: an underfilled prescription". The American Journal of Medicine. 127 (10): 905–11. doi:10.1016/j.amjmed.2014.05.007. PMID 24844736.
- 1 2 3 "How Is Coronary Heart Disease Treated?". 29 September 2014. Archived from the original on 24 February 2015. Retrieved 25 February 2015.
- ↑ Deb, S; Wijeysundera, HC; Ko, DT; Tsubota, H; Hill, S; Fremes, SE (20 November 2013). "Coronary artery bypass graft surgery vs percutaneous interventions in coronary revascularization: a systematic review". JAMA. 310 (19): 2086–95. doi:10.1001/jama.2013.281718. PMID 24240936.
- ↑ Rezende, PC; Scudeler, TL; da Costa, LM; Hueb, W (16 February 2015). "Conservative strategy for treatment of stable coronary artery disease". World Journal of Clinical Cases. 3 (2): 163–70. doi:10.12998/wjcc.v3.i2.163. PMC 4317610. PMID 25685763.
- ↑ Moran, AE; Forouzanfar, MH; Roth, GA; Mensah, GA; Ezzati, M; Murray, CJ; Naghavi, M (8 April 2014). "Temporal trends in ischemic heart disease mortality in 21 world regions, 1980 to 2010: the Global Burden of Disease 2010 study". Circulation. 129 (14): 1483–92. doi:10.1161/circulationaha.113.004042. PMC 4181359. PMID 24573352.
- ↑ Moran, AE; Forouzanfar, MH; Roth, GA; Mensah, GA; Ezzati, M; Flaxman, A; Murray, CJ; Naghavi, M (8 April 2014). "The global burden of ischemic heart disease in 1990 and 2010: the Global Burden of Disease 2010 study". Circulation. 129 (14): 1493–501. doi:10.1161/circulationaha.113.004046. PMC 4181601. PMID 24573351.
- 1 2 Centers for Disease Control and Prevention, (CDC) (14 October 2011). "Prevalence of coronary heart disease—United States, 2006–2010". MMWR. Morbidity and Mortality Weekly Report. 60 (40): 1377–81. PMID 21993341.
- 1 2 3 "What Is Sudden Cardiac Arrest?". NHLBI. June 22, 2016. Archived from the original on 28 July 2016. Retrieved 16 August 2016.
- 1 2 Field, John M. (2009). The Textbook of Emergency Cardiovascular Care and CPR. Lippincott Williams & Wilkins. p. 11. ISBN 9780781788991. Archived from the original on 2020-12-22. Retrieved 2020-07-13.
- 1 2 "What Are the Signs and Symptoms of Sudden Cardiac Arrest?". NHLBI. June 22, 2016. Archived from the original on 27 August 2016. Retrieved 16 August 2016.
- ↑ "What Causes Sudden Cardiac Arrest?". NHLBI. June 22, 2016. Archived from the original on 28 July 2016. Retrieved 16 August 2016.
- 1 2 "How Can Death Due to Sudden Cardiac Arrest Be Prevented?". NHLBI. June 22, 2016. Archived from the original on 27 August 2016. Retrieved 16 August 2016.
- ↑ "How Is Sudden Cardiac Arrest Treated?". NHLBI. June 22, 2016. Archived from the original on 27 August 2016. Retrieved 16 August 2016.
- ↑ Schenone, AL; Cohen, A; Patarroyo, G; Harper, L; Wang, X; Shishehbor, MH; Menon, V; Duggal, A (10 August 2016). "Therapeutic hypothermia after cardiac arrest: a systematic review/meta-analysis exploring the impact of expanded criteria and targeted temperature". Resuscitation. 108: 102–110. doi:10.1016/j.resuscitation.2016.07.238. PMID 27521472.
- ↑ Kronick, SL; Kurz, MC; Lin, S; Edelson, DP; Berg, RA; Billi, JE; Cabanas, JG; Cone, DC; Diercks, DB; Foster, JJ; Meeks, RA; Travers, AH; Welsford, M (3 November 2015). "Part 4: Systems of Care and Continuous Quality Improvement: 2015 American Heart Association Guidelines Update for Cardiopulmonary Resuscitation and Emergency Cardiovascular Care". Circulation. 132 (18 Suppl 2): S397–413. doi:10.1161/cir.0000000000000258. PMID 26472992.
- ↑ "Who Is at Risk for Sudden Cardiac Arrest?". NHLBI. June 22, 2016. Archived from the original on 23 August 2016. Retrieved 16 August 2016.
- ↑ Adams, James G. (2012). Emergency Medicine: Clinical Essentials (Expert Consult – Online). Elsevier Health Sciences. p. 1771. ISBN 978-1455733941. Archived from the original on 2020-12-22. Retrieved 2020-07-13.
- 1 2 3 4 5 "What Are Congenital Heart Defects?". National Heart, Lung, and Blood Institute. July 1, 2011. Archived from the original on 13 August 2015. Retrieved 10 August 2015.
- 1 2 3 4 5 6 7 8 9 Shanthi Mendis; Pekka Puska; Bo Norrving; World Health Organization (2011). Global Atlas on Cardiovascular Disease Prevention and Control (PDF). World Health Organization in collaboration with the World Heart Federation and the World Stroke Organization. pp. 3, 60. ISBN 978-92-4-156437-3. Archived (PDF) from the original on 2014-08-17. Retrieved 2020-07-13.
- 1 2 3 "What Are the Signs and Symptoms of Congenital Heart Defects?". National Heart, Lung, and Blood Institute. July 1, 2011. Archived from the original on 27 July 2015. Retrieved 10 August 2015.
- ↑ "What Causes Congenital Heart Defects?". National Heart, Lung, and Blood Institute. July 1, 2011. Archived from the original on 8 July 2015. Retrieved 10 August 2015.
- ↑ Dean, SV; Lassi, ZS; Imam, AM; Bhutta, ZA (26 September 2014). "Preconception care: nutritional risks and interventions". Reproductive Health. 11 Suppl 3: S3. doi:10.1186/1742-4755-11-s3-s3. PMC 4196560. PMID 25415364.
- 1 2 3 Milunsky, Aubrey (2011). "1". Genetic Disorders and the Fetus: Diagnosis, Prevention and Treatment. John Wiley & Sons. ISBN 9781444358216. Archived from the original on 2020-07-27. Retrieved 2020-07-13.
- 1 2 3 "How Are Congenital Heart Defects Treated?". National Heart, Lung, and Blood Institute. July 1, 2011. Archived from the original on 27 July 2015. Retrieved 10 August 2015.
- 1 2 Global Burden of Disease Study 2013, Collaborators (7 June 2015). "Global, regional, and national incidence, prevalence, and years lived with disability for 301 acute and chronic diseases and injuries in 188 countries, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 386 (9995): 743–800. doi:10.1016/S0140-6736(15)60692-4. PMC 4561509. PMID 26063472.
- ↑ GBD 2013 Mortality and Causes of Death, Collaborators (17 December 2014). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/S0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
- ↑ Upshaw, Charles (18 April 2007). "Henry J. L. Marriott: Lucid Teacher of Electrocardiography". Clinical Cardiology. 30 (4): 207–8. doi:10.1002/clc.6. PMC 6652921. PMID 17443652.
External links
| Look up cardiology in Wiktionary, the free dictionary. |
- American Heart Association Archived 2008-08-28 at the Wayback Machine
- About The HEART With Dr Alvin Ng Chee Keong