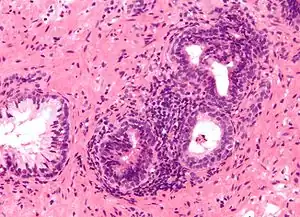
Prostatitis
Prostatitis is inflammation of the prostate gland.[1] There are two main types acute and chronic.[1] Acute prostatitis is sudden in onset, results in significant pain, and is less common.[1] Chronic prostatitis lasts for at least three months, symptoms come and go, and it is more common.[1] Complications of acute disease may include urinary retention or a prostate abscess.[1] Chronic disease may result in recurrent urinary tract infections.[2]
The cause of acute disease is generally a bacterial infection, while the cause of chronic disease is often less clear.[1] Chronic disease may be divided into chronic bacterial prostatitis and chronic prostatitis/chronic pelvic pain syndrome (CP/CPPS).[2] Another category is known as asymptomatic inflammatory prostatitis (AIP).[2] Diagnosis may involve examination, urine analysis, medical imaging, PSA testing, and semen testing.[2]
Treatment depends on the type.[1] Acute prostatitis is generally treated with antibiotics while chronic disease may be treated with alpha blockers and NSAIDs in addition to antibiotics.[1][2] Rarely surgery is required.[2] Asymptomatic prostatitis may not require treatment.[2]
Prostatitis affects about half of males at some point in time.[2] It represents the reason for about a quarter of urology visits related to urinary symptoms.[2] Prostatitis most commonly occurs in a persons 30s or 40s.[1] Prostatitis was first described by Verdies in 1838 and early treatments included leeches and prostatic message.[4]
Classification
The term prostatitis refers to inflammation of the tissue of the prostate gland. It may occur as an appropriate physiological response to an infection, or it may occur in the absence of infection.[5]
In 1999, the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK) devised a new classification system.[6][7] For more specifics about each type of prostatitis, including information on symptoms, treatment, and prognosis, follow the links to the relevant full articles.
| Category | Current name | Old name | Pain | Bacteria | WBCs | Description |
|---|---|---|---|---|---|---|
| I | Acute bacterial prostatitis[2] | Acute bacterial prostatitis | Yes | Yes | Yes | Bacterial infection of the prostate gland that requires urgent medical treatment. |
| II | Chronic bacterial prostatitis[2] | Chronic bacterial prostatitis | ± | Yes | Yes | A relatively rare condition that usually presents as intermittent urinary tract infections. |
| IIIa | Inflammatory CP/CPPS | Nonbacterial prostatitis | Yes | No | Yes | Accounts for 90–95% of prostatitis diagnoses,[8] formerly known as chronic nonbacterial prostatitis. |
| IIIb | Noninflammatory CP/CPPS | Prostatodynia | Yes | No | No | |
| IV | Asymptomatic inflammatory prostatitis[2] | (none) | No | No | Yes | No history of genitourinary pain complaints, but leukocytosis is noted, usually during evaluation for other conditions. Between 6 and 19% of men have pus cells in their semen but no symptoms.[9] |
.jpg.webp)
In 1968, Meares and Stamey determined a classification technique based upon the culturing of bacteria.[10] This classification is no longer used.
The conditions are distinguished by the different presentation of pain, white blood cells (WBCs) in the urine, duration of symptoms and bacteria cultured from the urine. To help express prostatic secretions that may contain WBCs and bacteria, prostate massage is sometimes used.[11]
See also
- Interstitial cystitis — a related disease
- Granulomatous prostatitis
- IgG4-related prostatitis
- Male accessory gland infection (MAGI)
References
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 18 "Prostatitis". nhs.uk. 19 October 2017. Archived from the original on 17 October 2017. Retrieved 7 November 2020.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 17 Khan, FU; Ihsan, AU; Khan, HU; Jana, R; Wazir, J; Khongorzul, P; Waqar, M; Zhou, X (October 2017). "Comprehensive overview of prostatitis". Biomedicine & pharmacotherapy = Biomedecine & pharmacotherapie. 94: 1064–1076. doi:10.1016/j.biopha.2017.08.016. PMID 28813783.
- ↑ Sharp, VJ; Takacs, EB; Powell, CR (15 August 2010). "Prostatitis: diagnosis and treatment". American family physician. 82 (4): 397–406. PMID 20704171.
- ↑ Partin, Alan W.; Wein, Alan J.; Kavoussi, Louis R.; Peters, Craig A.; Dmochowski, Roger R. (2020). Campbell Walsh Wein Urology, E-Book. Elsevier Health Sciences. p. 1202. ISBN 978-0-323-67227-6. Archived from the original on 2021-08-27. Retrieved 2020-11-07.
- ↑ Kirby, Roger; Carson, Culley C. (January–February 2015). "Editor's Comment on Diagnosis and treatment of chronic prostatitis/chronic pelvic pain syndrome". Trends in Urology and Men's Health. 6 (1): 17. doi:10.1002/tre.434.
- ↑ Krieger JN, Nyberg L, Nickel JC (July 1999). "NIH consensus definition and classification of prostatitis". JAMA. 282 (3): 236–7. doi:10.1001/jama.282.3.236. PMID 10422990.
- ↑ J. Curtis Nickel (1999). Textbook of prostatitis. Taylor & Francis. pp. 27–. ISBN 978-1-901865-04-2. Retrieved 18 April 2010.
- ↑ Habermacher GM, Chason JT, Schaeffer AJ (2006). "Prostatitis/chronic pelvic pain syndrome". Annu. Rev. Med. 57: 195–206. doi:10.1146/annurev.med.57.011205.135654. PMID 16409145.
- ↑ Korrovits P, Ausmees K, Mändar R, Punab M (June 2008). "Prevalence of asymptomatic inflammatory (National Institutes of Health Category IV) prostatitis in young men according to semen analysis". Urology. 71 (6): 1010–5. doi:10.1016/j.urology.2007.12.082. PMID 18455767.
- ↑ Meares EM, Stamey TA (March 1968). "Bacteriologic localization patterns in bacterial prostatitis and urethritis". Invest Urol. 5 (5): 492–518. PMID 4870505.
- ↑ "Prostatitis: Benign Prostate Disease: Merck Manual Professional". Archived from the original on 2011-09-25. Retrieved 2011-07-11.
External links
| Classification | |
|---|---|
| External resources |
- Prostatitis Self Assessment Calculator Archived 2016-07-01 at the Wayback Machine