Pneumocystis jirovecii
| Pneumocystis jirovecii | |
|---|---|
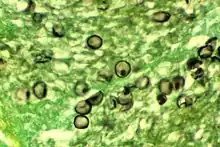 | |
| P. jirovecii cysts in tissue | |
| Scientific classification | |
| Domain: | Eukaryota |
| Kingdom: | Fungi |
| Division: | Ascomycota |
| Class: | Pneumocystidomycetes |
| Order: | Pneumocystidales |
| Family: | Pneumocystidaceae |
| Genus: | Pneumocystis |
| Species: | P. jirovecii |
| Binomial name | |
| Pneumocystis jirovecii J.K.Frenkel | |
| Synonyms | |
| |
Pneumocystis jirovecii (previously P. carinii) is a yeast-like fungus of the genus Pneumocystis. The causative organism of Pneumocystis pneumonia, it is an important human pathogen, particularly among immunocompromised hosts. Prior to its discovery as a human-specific pathogen, P. jirovecii was known as P. carinii.
Genome
Pneumocystis species cannot be grown in culture, so the availability of the human disease-causing agent, P. jirovecii, is limited. Hence, investigation of the whole genome of a Pneumocystis is largely based upon true P. carinii available from experimental rats, which can be maintained with infections. Genetic material of other species, such as P. jirovecii, can be compared to the genome of P. carinii.[1]
The genome of P. jirovecii has been sequenced from a bronchoalveolar lavage sample.[2]
The genome is small, low in G+C content, and lacks most amino-acid biosynthesis enzymes.
Lifecycle
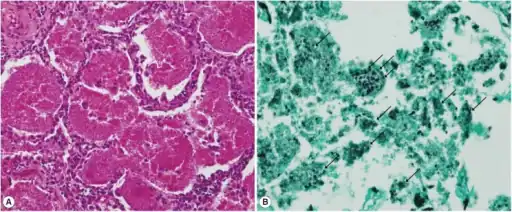
The complete lifecycles of any of the species of Pneumocystis are not known, but presumably all resemble the others in the genus. The terminology follows zoological terms, rather than mycological terms, reflecting the initial misdetermination as a protozoan parasite. It is an extracellular fungus. All stages are found in lungs and because they cannot be cultured ex vivo, direct observation of living Pneumocystis is difficult. The trophozoite stage is thought to be equivalent to the so-called vegetative state of other species (such as Schizosaccharomyces pombe), which like Pneumocystis, belong to the Taphrinomycotina branch of the fungal kingdom.[3] The trophozoite stage is single-celled and appears amoeboid (multilobed) and closely associated with host cells. Globular cysts eventually form that have a thicker wall. Within these ascus-like cysts, eight spores form, which are released through rupture of the cyst wall. The cysts often collapse, forming crescent-shaped bodies visible in stained tissue. Whether meiosis takes place within the cysts, or what the genetic status is of the various cell types, is not known for certain.[4]
Homothallism
The lifecycle of P. jirovecii is thought to include both asexual and sexual phases.[5] Asexual multiplication of haploid cells likely occurs by binary fission. The mode of sexual reproduction appears to be primary homothallism, a form of self-fertilization.[5] The sexual phase takes place in the host's lungs. This phase is presumed to involve formation of a diploid zygote, followed by meiosis, and then production of an ascus containing the products of meiosis, eight haploid ascospores. The ascospores may be disseminated by airborne transmission to new hosts.
Nomenclature
At first, the name Pneumocystis carinii was applied to the organisms found in both rats and humans, as the parasite was not yet known to be host-specific. In 1976, the name "Pneumocystis jiroveci" was proposed for the first time, to distinguish the organism found in humans from variants of Pneumocystis in other animals. The organism was named thus in honor of Czech parasitologist Otto Jirovec, who described Pneumocystis pneumonia in humans in 1952. After DNA analysis showed significant differences in the human variant, the proposal was made again in 1999 and has come into common use.[6]
The name was spelled according to the International Code of Zoological Nomenclature, since the organism was believed to be a protozoan. After it became clear that it was a fungus, the name was changed to Pneumocystis jirovecii,[7] according to the International Code of Nomenclature for algae, fungi, and plants (ICNafp), which requires such names be spelled with double i (ii).[8] Both spellings are commonly used, but according to the ICNafp, P. jirovecii is correct.[9] A change in the ICNafp now recognizes the validity of the 1976 publication, making the 1999 proposal redundant, and cites Pneumocystis and P. jiroveci as examples of the change in ICN Article 45, Ex 7. The name P. jiroveci is typified (both lectotypified and epitypified) by samples from human autopsies dating from the 1960s. [10]
The term PCP, which was widely used by practitioners and patients, has been retained for convenience, with the rationale that it now stands for the more general Pneumocystis pneumonia rather than Pneumocystis carinii pneumonia.
The name P. carinii is incorrect for the human variant, but still describes the species found in rats, and that name is typified by an isolate from rats.[10]
History
The earliest report of this genus appears to have been that of Carlos Chagas in 1909,[11] who discovered it in experimental animals, but confused it with part of the lifecycle of Trypanosoma cruzi (causal agent of Chagas disease) and later called both organisms Schizotrypanum cruzi, a form of trypanosome infecting humans.[12] The rediscovery of Pneumocystis cysts was reported by Antonio Carini in 1910, also in Brazil.[13] The genus was again discovered in 1912 by Delanoë and Delanoë, this time at the Pasteur Institute in Paris, who found it in rats and proposed the genus and species name Pneumocystis carinii after Carini.[14]
Pneumocystis was redescribed as a human pathogen in 1942 by two Dutch investigators, van der Meer and Brug, who found it in three new cases: a 3-month-old infant with congenital heart disease and in two of 104 autopsy cases – a 4-month-old infant and a 21-year-old adult.[15] There being only one described species in the genus, they considered the human parasite to be P. carinii. Nine years later (1951), Dr. Josef Vanek at Charles University in Prague, Czechoslovakia, showed in a study of lung sections from 16 children that the organism labelled "P. carinii" was the causative agent of pneumonia in these children.[16] The following year, Jírovec reported "P. carinii" as the cause of interstitial pneumonia in neonates.[17][18][19] Following the realization that Pneumocystis from humans could not infect experimental animals such as rats, and that the rat form of Pneumocystis differed physiologically and had different antigenic properties, Frenkel[20] was the first to recognize the human pathogen as a distinct species. He named it "Pneumocystis jiroveci" (corrected to P. jirovecii - see nomenclature above). Controversy existed over the relabeling of P. carinii in humans as P. jirovecii,[10][21] which is why both names still appear in publications. However, only the name P. jirovecii is used exclusively for the human pathogen, whereas the name P. carinii has had a broader application to many species.[22] Frenkel and those before him believed that all Pneumocystis were protozoans, but soon afterwards evidence began accumulating that Pneumocystis was a fungal genus. Recent studies show it to be an unusual, in some ways a primitive genus of Ascomycota, related to a group of yeasts.[3] Every tested primate, including humans, appears to have its own type of Pneumocystis that is incapable of cross-infecting other host species and has co-evolved with each species.[23] Currently, only five species have been formally named: P. jirovecii from humans, P. carinii as originally named from rats, P. murina from mice,[24] P. wakefieldiae[25][26] also from rats, and P. oryctolagi from rabbits.[27]
Historical and even recent reports of P. carinii from humans are based upon older classifications (still used by many, or those still debating the recognition of distinct species in the genus Pneumocystis) which does not mean that the true P. carinii from rats actually infects humans. In an intermediate classification system, the various taxa in different mammals have been called formae speciales or forms. For example, the human "form" was called Pneumocystis carinii f. [or f. sp.] hominis, while the original rat infecting form was called Pneumocystis carinii f. [or f. sp.] carinii. This terminology is still used by some researchers. The species of Pneumocystis originally seen by Chagas have not yet been named as distinct species.[10] Many other undescribed species presumably exist and those that have been detected in many mammals are only known from molecular sample detection from lung tissue or fluids, rather than by direct physical observation.[28][29] Currently, they are cryptic taxa.
Medical relevance
Pneumocystis pneumonia is an important disease of immunocompromised humans, particularly patients with HIV, but also patients with an immune system that is severely suppressed for other reasons, for example, following a bone marrow transplant. In humans with a normal immune system, it is an extremely common silent infection.[30]
Identified by methenamine silver stain of lung tissue, type I pneumocytes, and type II pneumocytes over-replicate and damage alveolar epithelium, causing death by asphyxiation. Fluid leaks into alveoli, producing an exudate seen as honeycomb/cotton candy appearance on hematoxylin and eosin-stained slides. Drug of choice is trimethoprim/sulfamethoxazole, pentamidine, or dapsone. In HIV patients, most cases occur when the CD4 count is below 200 cells per microliter.
References
- ↑ "Pneumocystis Genome Project". Pgp.cchmc.org. Archived from the original on 2013-05-15. Retrieved 2013-03-26.
- ↑ Cisse, O. H; Pagni, M; Hauser, P. M (2012). "De Novo Assembly of the Pneumocystis jirovecii Genome from a Single Bronchoalveolar Lavage Fluid Specimen from a Patient". mBio. 4 (1): e00428–12. doi:10.1128/mBio.00428-12. PMC 3531804. PMID 23269827.
- 1 2 James TY, et al. (2006). "Reconstructing the early evolution of Fungi using a six-dp[k geny". Nature. 443 (7113): 818–822. doi:10.1038/nature05110. PMID 17051209. S2CID 4302864.
- ↑ "see DPDx life-cycle diagram". Dpd.cdc.gov. Archived from the original on 2013-03-18. Retrieved 2013-03-26.
- 1 2 Richard S, Almeida JM, Cissé OH, Luraschi A, Nielsen O, Pagni M, Hauser PM (2018). "Functional and Expression Analyses of the Pneumocystis MAT Genes Suggest Obligate Sexuality through Primary Homothallism within Host Lungs". mBio. 9 (1). doi:10.1128/mBio.02201-17. PMC 5821091. PMID 29463658.
- ↑ Stringer JR, Beard CB, Miller RF, Wakefield AE (2002). "A New Name for Pneumocystis from Humans and New Perspectives on the Host-Pathogen Relationship". Emerging Infectious Diseases. 8 (9): 891–6. doi:10.3201/eid0809.020096. PMC 2732539. PMID 12194762.
- ↑ Stringer JR, Beard CB, Miller RF (2009). "Spelling Pneumocystis jiroveci" (PDF). Emerging Infectious Diseases. 15 (3): 506a–506. doi:10.3201/eid1503.081060. PMC 2681121. PMID 19239784. Archived (PDF) from the original on 2011-06-04. Retrieved 2023-06-03.
- ↑ "ICBN Recommendation 60C.1". Archived from the original on 2021-01-26. Retrieved 2023-06-03.
If the personal name ends with a consonant (except -er), substantival epithets are formed by adding -i- (stem augmentation) plus the genitive inflection appropriate to the sex and number of the person(s) honoured (e.g. lecardii for Théodore Lecard).
- ↑ "International Code of Nomenclature for algae, fungi, and plants". www.iapt-taxon.org. Archived from the original on 2019-12-16. Retrieved 2023-06-03.
- 1 2 3 4 Redhead SA, Cushion MT, Frenkel JK, Stringer JR (2006). "Pneumocystis and Trypanosoma cruzi: nomenclature and typifications". J Eukaryot Microbiol. 53 (1): 2–11. doi:10.1111/j.1550-7408.2005.00072.x. PMID 16441572. S2CID 38119833.
- ↑ Chagas C (1909). "Neue Trypanosomen". Vorläufige Mitteilung. Arch. Schiff. Tropenhyg. 13: 120–122.
- ↑ Chagas C (1909). "Nova tripanozomiase humana: Estudos sobre a morfolojia e o ciclo evolutivo do Schizotrypanum cruzi n. gen., n. sp., ajente etiolojico de nova entidade morbida do homem". Mem Inst Oswaldo Cruz. 1 (2): 159–218. doi:10.1590/S0074-02761909000200008.
- ↑ Carini A. (1910). "Formas des eschizogonia do Trypanosoma lewisi". Soc Med Cir São Paulo. 38 (8).
- ↑ Delanoë P, Delanoë M (1912). "Sur les rapports des kystes de Carini du poumon des rats avec le Trypanosoma lewisi". Comptes Rendus de l'Académie des Sciences. 155: 658–61.
- ↑ van der Meer MG, Brug SL (1942). "Infection à Pneumocystis chez l'homme et chez les animaux". Amer Soc Belge Méd Trop. 22: 301–9.
- ↑ Vanek J. (1951). "Atypicka (interstitiálni) pneumonie detí vyvolaná Pneumocystis carinii (Atypical interstitial pneumonia of infants produced by Pneumocystis carinii)". Casop Lék Cesk. 90: 1121–4.
- ↑ Jírovec O. (1952). "Pneumocystis carinii puvodce t. zv intertitialnich plasmocelularnich pneumonii kojencw (Pneumocystis carinii, the cause of interstitial plasmacellular pneumonia in neonates)". CSL. Hyg. Epid. Mikrob. 1: 141.
- ↑ Vanek J, Jírovec O, Lukes J (1953). "Interstitial plasma cell pneumonia in infants". Annales Paediatrici. 180 (1): 1–21. PMID 13051050.
- ↑ Gajdusek DC (1957). "Pneumocystis carinii; etiologic agent of interstitial plasma cell pneumonia of premature and young infants". Pediatrics. 19 (4 Pt 1): 543–65. doi:10.1542/peds.19.4.543. PMID 13419426. S2CID 19507186.
- ↑ Frenkel JK (1976). "Pneumocystis jiroveci n. sp. from man: morphology, physiology, and immunology in relation to pathology". Natl Cancer Inst Monogr. 43: 13–27. PMID 828240.
- ↑ Gigliotti F (2005). "Pneumocystis carinii: has the name really been changed?". Clin Infect Dis. 41 (12): 1752–5. doi:10.1086/498150. PMID 16288399.
- ↑ Hawksworth DL (2007). "Responsibility in naming pathogens: the case of Pneumocystis jiroveci, the causal agent of pneumocystis pneumonia". Lancet Infect. Dis. 7 (1): 3–5. doi:10.1016/S1473-3099(06)70663-6. PMID 17182335.
- ↑ Hugot J, Demanche C, Barriel V, Dei-Cas E, Guillot J (2003). "Phylogenetic systematics and evolution of primate-derived Pneumocystis based on mitochondrial or nuclear DNA sequence comparison". Syst Biol. 52 (6): 735–744. doi:10.1080/10635150390250893. PMID 14668114.
- ↑ Keely S, Fischer J, Cushion M, Stringer J (2004). "Phylogenetic identification of Pneumocystis murina sp. nov., a new species in laboratory mice". Microbiology. 150 (Pt 5): 1153–65. doi:10.1099/mic.0.26921-0. PMID 15133075.
- ↑ Cushion MT, Keely SP, Stringer JR (2004). "Molecular and phenotypic description of Pneumocystis wakefieldiae sp. nov., a new species in rats". Mycologia. 96 (3): 429–438. doi:10.2307/3762163. JSTOR 3762163. PMID 21148866.
- ↑ Cushion MT, Keely SP, Stringer JR (2005). "Validation of the name Pneumocystis wakefieldiae". Mycologia. 97: 268. doi:10.3852/mycologia.97.1.268.
- ↑ Dei-Cas E, et al. (2006). "Pneumocystis oryctolagi sp. nov., an uncultured fungus causing pneumonia in rabbits at weaning: review of current knowledge, and description of a new taxon on genotypic, phylogenetic and phenotypic bases". FEMS Microbiol. Rev. 30 (6): 853–871. doi:10.1111/j.1574-6976.2006.00037.x. PMID 17064284.
- ↑ Aliouat-Denis, C-M.; et al. (2008). "Pneumocystis species, co-evolution and pathogenic power". Infection, Genetics and Evolution. 8 (5): 708–726. doi:10.1016/j.meegid.2008.05.001. PMID 18565802.
- ↑ Demanche C, et al. (2001). "Phylogeny of Pneumocystis carinii from 18 Primate Species Confirms Host Specificity and Suggests Coevolution". J. Clin. Microbiol. 39 (6): 2126–2133. doi:10.1128/JCM.39.6.2126-2133.2001. PMC 88100. PMID 11376046.
- ↑ Ponce CA, Gallo M, Bustamante R, Vargas SL (2010). "Pneumocystis colonization is highly prevalent in the autopsied lungs of the general population". Clin Infect Dis. 50 (3): 347–353. doi:10.1086/649868. PMID 20047487.