Birth control
| Birth control | |
|---|---|
| Other names: Contraception, fertility control | |
 | |
| A package of birth control pills | |
| Specialty | Family medicine |
| Indications | Prevent pregnancy[1] |
Birth control, also known as contraception and fertility control, is a method or device used to prevent pregnancy.[1] Birth control has been used since ancient times, but effective and safe methods of birth control only became available in the 20th century.[2] Planning, making available, and using birth control is called family planning.[3][4] Some cultures limit or discourage access to birth control because they consider it to be morally, religiously, or politically undesirable.[2]
The most effective methods of birth control are sterilization by means of vasectomy in males and tubal ligation in females, intrauterine devices (IUDs), and implantable birth control.[5] This is followed by a number of hormone-based methods including oral pills, patches, vaginal rings, and injections.[5] Less effective methods include physical barriers such as condoms, diaphragms and birth control sponges and fertility awareness methods.[5] The least effective methods are spermicides and withdrawal by the male before ejaculation.[5] Sterilization, while highly effective, is not usually reversible; all other methods are reversible, most immediately upon stopping them.[5] Safe sex practices, such as with the use of male or female condoms, can also help prevent sexually transmitted infections.[6] Other methods of birth control do not protect against sexually transmitted diseases.[7] Emergency birth control can prevent pregnancy if taken within 72 to 120 hours after unprotected sex.[8][9] Some argue not having sex is also a form of birth control, but abstinence-only sex education may increase teenage pregnancies if offered without birth control education, due to non-compliance.[10][11]
In teenagers, pregnancies are at greater risk of poor outcomes.[12] Comprehensive sex education and access to birth control decreases the rate of unwanted pregnancies in this age group.[12][13] While all forms of birth control can generally be used by young people,[14] long-acting reversible birth control such as implants, IUDs, or vaginal rings are more successful in reducing rates of teenage pregnancy.[13] After the delivery of a child, a woman who is not exclusively breastfeeding may become pregnant again after as few as four to six weeks.[14] Some methods of birth control can be started immediately following the birth, while others require a delay of up to six months.[14] In women who are breastfeeding, progestin-only methods are preferred over combined oral birth control pills.[14] In women who have reached menopause, it is recommended that birth control be continued for one year after the last period.[14]
About 222 million women who want to avoid pregnancy in developing countries are not using a modern birth control method.[15][16] Birth control use in developing countries has decreased the number of deaths during or around the time of pregnancy by 40% (about 270,000 deaths prevented in 2008) and could prevent 70% if the full demand for birth control were met.[17][18] By lengthening the time between pregnancies, birth control can improve adult women's delivery outcomes and the survival of their children.[17] In the developing world, women's earnings, assets, and weight, as well as their children's schooling and health, all improve with greater access to birth control.[19] Birth control increases economic growth because of fewer dependent children, more women participating in the workforce, and less use of scarce resources.[19][20]
Methods
| Method | Typical use | Perfect use |
|---|---|---|
| No birth control | 85% | 85% |
| Combination pill | 9% | 0.3% |
| Progestin-only pill | 13% | 1.1% |
| Sterilization (female) | 0.5% | 0.5% |
| Sterilization (male) | 0.15% | 0.1% |
| Condom (female) | 21% | 5% |
| Condom (male) | 18% | 2% |
| Copper IUD | 0.8% | 0.6% |
| Hormonal IUD | 0.2% | 0.2% |
| Patch | 9% | 0.3% |
| Vaginal ring | 9% | 0.3% |
| MPA shot | 6% | 0.2% |
| Implant | 0.05% | 0.05% |
| Diaphragm and spermicide | 12% | 6% |
| Fertility awareness | 24% | 0.4–5% |
| Withdrawal | 22% | 4% |
| Lactational amenorrhea method (6 months failure rate) | 0–7.5%[23] | <2%[24] |
Birth control methods include barrier methods, hormonal birth control, intrauterine devices (IUDs), sterilization, and behavioral methods. They are used before or during sex while emergency contraceptives are effective for up to five days after sex. Effectiveness is generally expressed as the percentage of women who become pregnant using a given method during the first year,[25] and sometimes as a lifetime failure rate among methods with high effectiveness, such as tubal ligation.[26]
The most effective methods are those that are long acting and do not require ongoing health care visits.[27] Surgical sterilization, implantable hormones, and intrauterine devices all have first-year failure rates of less than 1%.[21] Hormonal contraceptive pills, patches or vaginal rings, and the lactational amenorrhea method (LAM), if adhered to strictly, can also have first-year (or for LAM, first-6-month) failure rates of less than 1%.[27] With typical use, first-year failure rates are considerably high, at 9%, due to inconsistent use.[21] Other methods such as condoms, diaphragms, and spermicides have higher first-year failure rates even with perfect usage.[27] The American Academy of Pediatrics recommends long acting reversible birth control as first line for young individuals.[28]
While all methods of birth control have some potential adverse effects, the risk is less than that of pregnancy.[27] After stopping or removing many methods of birth control, including oral contraceptives, IUDs, implants and injections, the rate of pregnancy during the subsequent year is the same as for those who used no birth control.[29]
For individuals with specific health problems, certain forms of birth control may require further investigations.[30] For women who are otherwise healthy, many methods of birth control should not require a medical exam—including birth control pills, injectable or implantable birth control, and condoms.[31] For example, a pelvic exam, breast exam, or blood test before starting birth control pills does not appear to affect outcomes.[32][33][34] In 2009, the World Health Organization (WHO) published a detailed list of medical eligibility criteria for each type of birth control.[30]
Hormonal
Hormonal contraception is available in a number of different forms, including oral pills, implants under the skin, injections, patches, IUDs and a vaginal ring. They are currently available only for women, although hormonal contraceptives for men have been and are being clinically tested.[35] There are two types of oral birth control pills, the combined oral contraceptive pills (which contain both estrogen and a progestin) and the progestogen-only pills (sometimes called minipills).[36] If either is taken during pregnancy, they do not increase the risk of miscarriage nor cause birth defects.[33] Both types of birth control pills prevent fertilization mainly by inhibiting ovulation and thickening cervical mucus.[37][38] They may also change the lining of the uterus and thus decrease implantation.[38] Their effectiveness depends on the user's adherence to taking the pills.[33]
Combined hormonal contraceptives are associated with a slightly increased risk of venous and arterial blood clots.[39] Venous clots, on average, increase from 2.8 to 9.8 per 10,000 women years[40] which is still less than that associated with pregnancy.[39] Due to this risk, they are not recommended in women over 35 years of age who continue to smoke.[41] Due to the increased risk, they are included in decision tools such as the DASH score and PERC rule used to predict the risk of blood clots.[42]
The effect on sexual desire is varied, with increase or decrease in some but with no effect in most.[43] Combined oral contraceptives reduce the risk of ovarian cancer and endometrial cancer and do not change the risk of breast cancer.[44][45] They often reduce menstrual bleeding and painful menstruation cramps.[33] The lower doses of estrogen released from the vaginal ring may reduce the risk of breast tenderness, nausea, and headache associated with higher dose estrogen products.[44]
Progestin-only pills, injections and intrauterine devices are not associated with an increased risk of blood clots and may be used by women with a history of blood clots in their veins.[39][46] In those with a history of arterial blood clots, non-hormonal birth control or a progestin-only method other than the injectable version should be used.[39] Progestin-only pills may improve menstrual symptoms and can be used by breastfeeding women as they do not affect milk production. Irregular bleeding may occur with progestin-only methods, with some users reporting no periods.[47] The progestins drospirenone and desogestrel minimize the androgenic side effects but increase the risks of blood clots and are thus not first line.[48] The perfect use first-year failure rate of injectable progestin is 0.2%; the typical use first failure rate is 6%.[21]
 Three varieties of birth control pills in calendar oriented packaging
Three varieties of birth control pills in calendar oriented packaging Birth control pills
Birth control pills A transdermal contraceptive patch
A transdermal contraceptive patch A NuvaRing vaginal ring
A NuvaRing vaginal ring
Barrier
Barrier contraceptives are devices that attempt to prevent pregnancy by physically preventing sperm from entering the uterus.[49] They include male condoms, female condoms, cervical caps, diaphragms, and contraceptive sponges with spermicide.[49]
Globally, condoms are the most common method of birth control.[50] Male condoms are put on a man's erect penis and physically block ejaculated sperm from entering the body of a sexual partner.[51] Modern condoms are most often made from latex, but some are made from other materials such as polyurethane, or lamb's intestine.[51] Female condoms are also available, most often made of nitrile, latex or polyurethane.[52] Male condoms have the advantage of being inexpensive, easy to use, and have few adverse effects.[53] Making condoms available to teenagers does not appear to affect the age of onset of sexual activity or its frequency.[54] In Japan, about 80% of couples who are using birth control use condoms, while in Germany this number is about 25%,[55] and in the United States it is 18%.[56]
Male condoms and the diaphragm with spermicide have typical use first-year failure rates of 18% and 12%, respectively.[21] With perfect use condoms are more effective with a 2% first-year failure rate versus a 6% first-year rate with the diaphragm.[21] Condoms have the additional benefit of helping to prevent the spread of some sexually transmitted infections such as HIV/AIDS, however, condoms made from animal intestine do not.[5][57]
Contraceptive sponges combine a barrier with a spermicide.[27] Like diaphragms, they are inserted vaginally before intercourse and must be placed over the cervix to be effective.[27] Typical failure rates during the first year depend on whether or not a woman has previously given birth, being 24% in those who have and 12% in those who have not.[21] The sponge can be inserted up to 24 hours before intercourse and must be left in place for at least six hours afterward.[27] Allergic reactions[58] and more severe adverse effects such as toxic shock syndrome have been reported.[59]
 A rolled up male condom.
A rolled up male condom. An unrolled male latex condom
An unrolled male latex condom A polyurethane female condom
A polyurethane female condom
 A contraceptive sponge set inside its open package.
A contraceptive sponge set inside its open package.
Intrauterine devices

The current intrauterine devices (IUD) are small devices, often 'T'-shaped, containing either copper or levonorgestrel, which are inserted into the uterus. They are one form of long-acting reversible contraception which are the most effective types of reversible birth control.[60] Failure rates with the copper IUD is about 0.8% while the levonorgestrel IUD has a failure rates of 0.2% in the first year of use.[61] Among types of birth control, they, along with birth control implants, result in the greatest satisfaction among users.[62] As of 2007, IUDs are the most widely used form of reversible contraception, with more than 180 million users worldwide.[63]
Evidence supports effectiveness and safety in adolescents[62] and those who have and have not previously had children.[64] IUDs do not affect breastfeeding and can be inserted immediately after delivery.[65] They may also be used immediately after an abortion.[66][67] Once removed, even after long term use, fertility returns to normal immediately.[68]
While copper IUDs may increase menstrual bleeding and result in more painful cramps,[69] hormonal IUDs may reduce menstrual bleeding or stop menstruation altogether.[65] Cramping can be treated with painkillers like non-steroidal anti-inflammatory drugs.[70] Other potential complications include expulsion (2–5%) and rarely perforation of the uterus (less than 0.7%).[65][70] A previous model of the intrauterine device (the Dalkon shield) was associated with an increased risk of pelvic inflammatory disease, however the risk is not affected with current models in those without sexually transmitted infections around the time of insertion.[71] IUDs appear to decrease the risk of ovarian cancer.[72]
Sterilization
Surgical sterilization is available in the form of tubal ligation for women and vasectomy for men.[2] There are no significant long term side effects, and tubal ligation decreases the risk of ovarian cancer.[2] Short term complications are twenty times less likely from a vasectomy than a tubal ligation.[2][73] After a vasectomy, there may be swelling and pain of the scrotum which usually resolves in one or two weeks.[74] With tubal ligation, complications occur in 1 to 2 percent of procedures with serious complications usually due to the anesthesia.[75] Neither method offers protection from sexually transmitted infections.[2]
This decision may cause regret in some men and women. Of women aged over 30 who have undergone tubal ligation, about 5% regret their decision, as compared with 20% of women aged under 30.[2] By contrast, less than 5% of men are likely to regret sterilization. Men who are more likely to regret sterilization are younger, have young or no children, or have an unstable marriage.[76] In a survey of biological parents, 9% stated they would not have had children if they were able to do it over again.[77]
Although sterilization is considered a permanent procedure,[78] it is possible to attempt a tubal reversal to reconnect the fallopian tubes or a vasectomy reversal to reconnect the vasa deferentia. In women, the desire for a reversal is often associated with a change in spouse.[78] Pregnancy success rates after tubal reversal are between 31 and 88 percent, with complications including an increased risk of ectopic pregnancy.[78] The number of males who request reversal is between 2 and 6 percent.[79] Rates of success in fathering another child after reversal are between 38 and 84 percent; with success being lower the longer the time period between the vasectomy and the reversal.[79] Sperm extraction followed by in vitro fertilization may also be an option in men.[80]
Behavioral
Behavioral methods involve regulating the timing or method of intercourse to prevent introduction of sperm into the female reproductive tract, either altogether or when an egg may be present.[81] If used perfectly the first-year failure rate may be around 3.4%, however if used poorly first-year failure rates may approach 85%.[82]
Fertility awareness
.jpg.webp)
Fertility awareness methods involve determining the most fertile days of the menstrual cycle and avoiding unprotected intercourse.[81] Techniques for determining fertility include monitoring basal body temperature, cervical secretions, or the day of the cycle.[81] They have typical first-year failure rates of 24%; perfect use first-year failure rates depend on which method is used and range from 0.4% to 5%.[21] The evidence on which these estimates are based, however, is poor as the majority of people in trials stop their use early.[81] Globally, they are used by about 3.6% of couples.[83] If based on both basal body temperature and another primary sign, the method is referred to as symptothermal. First-year failure rates of 20% overall and 0.4% for perfect use have been reported in clinical studies of the symptothermal method.[84][21] A number of fertility tracking apps are available, as of 2016, but they are more commonly designed to assist those trying to get pregnant rather than prevent pregnancy.[85]
Withdrawal
The withdrawal method (also known as coitus interruptus) is the practice of ending intercourse ("pulling out") before ejaculation.[86] The main risk of the withdrawal method is that the man may not perform the maneuver correctly or in a timely manner.[86] First-year failure rates vary from 4% with perfect usage to 22% with typical usage.[21] It is not considered birth control by some medical professionals.[27]
There is little data regarding the sperm content of pre-ejaculatory fluid.[87] While some tentative research did not find sperm,[87] one trial found sperm present in 10 out of 27 volunteers.[88] The withdrawal method is used as birth control by about 3% of couples.[83]
Abstinence
Sexual abstinence may be used as a form of birth control, meaning either not engaging in any type of sexual activity, or specifically not engaging in vaginal intercourse, while engaging in other forms of non-vaginal sex.[89][90] Complete sexual abstinence is 100% effective in preventing pregnancy.[91][92] However, among those who take a pledge to abstain from premarital sex, as many as 88% who engage in sex, do so prior to marriage.[93] The choice to abstain from sex cannot protect against pregnancy as a result of rape, and public health efforts emphasizing abstinence to reduce unwanted pregnancy may have limited effectiveness, especially in developing countries and among disadvantaged groups.[94][95]
Deliberate non-penetrative sex without vaginal sex or deliberate oral sex without vaginal sex are also sometimes considered birth control.[89] While this generally avoids pregnancy, pregnancy can still occur with intercrural sex and other forms of penis-near-vagina sex (genital rubbing, and the penis exiting from anal intercourse) where sperm can be deposited near the entrance to the vagina and can travel along the vagina's lubricating fluids.[96][97]
Abstinence-only sex education does not reduce teenage pregnancy.[7][98] Teen pregnancy rates and STI rates are generally the same or higher in states where students are given abstinence-only education, as compared with comprehensive sex education.[98] Some authorities recommend that those using abstinence as a primary method have backup methods available (such as condoms or emergency contraceptive pills).[99]
Lactation
The lactational amenorrhea method involves the use of a woman's natural postpartum infertility which occurs after delivery and may be extended by breastfeeding.[100] This usually requires the presence of no periods, exclusively breastfeeding the infant, and a child younger than six months.[24] The World Health Organization states that if breastfeeding is the infant's only source of nutrition, the failure rate is 2% in the six months following delivery.[101] Six uncontrolled studies of lactational amenorrhea method users found failure rates at 6 months postpartum between 0% and 7.5%.[102] Failure rates increase to 4–7% at one year and 13% at two years.[103] Feeding formula, pumping instead of nursing, the use of a pacifier, and feeding solids all increase its failure rate.[104] In those who are exclusively breastfeeding, about 10% begin having periods before three months and 20% before six months.[103] In those who are not breastfeeding, fertility may return four weeks after delivery.[103]
Emergency
.jpg.webp)
Emergency contraceptive methods are medications (sometimes misleadingly referred to as "morning-after pills")[105] or devices used after unprotected sexual intercourse with the hope of preventing pregnancy.[8] They work primarily by preventing ovulation or fertilization.[2][106] They are unlikely to affect implantation, but this has not been completely excluded.[106] A number of options exist, including high dose birth control pills, levonorgestrel, mifepristone, ulipristal and IUDs.[107] Providing emergency contraceptive pills to women in advance does not affect rates of sexually transmitted infections, condom use, pregnancy rates, or sexual risk-taking behavior.[108][109] All methods have minimal side effects.[107]
Levonorgestrel pills, when used within 3 days, decrease the chance of pregnancy after a single episode of unprotected sex or condom failure by 70% (resulting in a pregnancy rate of 2.2%).[8] Ulipristal, when used within 5 days, decreases the chance of pregnancy by about 85% (pregnancy rate 1.4%) and is more effective than levonorgestrel.[8][107][110] Mifepristone is also more effective than levonorgestrel, while copper IUDs are the most effective method.[107] IUDs can be inserted up to five days after intercourse and prevent about 99% of pregnancies after an episode of unprotected sex (pregnancy rate of 0.1 to 0.2%).[2][111] This makes them the most effective form of emergency contraceptive.[112] In those who are overweight or obese, levonorgestrel is less effective and an IUD or ulipristal is recommended.[113]
Dual protection
Dual protection is the use of methods that prevent both sexually transmitted infections and pregnancy.[114] This can be with condoms either alone or along with another birth control method or by the avoidance of penetrative sex.[115][116]
If pregnancy is a high concern, using two methods at the same time is reasonable.[115] For example, two forms of birth control are recommended in those taking the anti-acne drug isotretinoin or anti-epileptic drugs like carbamazepine, due to the high risk of birth defects if taken during pregnancy.[117][118]
Effects
Health


Contraceptive use in developing countries is estimated to have decreased the number of maternal deaths by 40% (about 270,000 deaths prevented in 2008) and could prevent 70% of deaths if the full demand for birth control were met.[17][18] These benefits are achieved by reducing the number of unplanned pregnancies that subsequently result in unsafe abortions and by preventing pregnancies in those at high risk.[17]
Birth control also improves child survival in the developing world by lengthening the time between pregnancies.[17] In this population, outcomes are worse when a mother gets pregnant within eighteen months of a previous delivery.[17][120] Delaying another pregnancy after a miscarriage however does not appear to alter risk and women are advised to attempt pregnancy in this situation whenever they are ready.[120]
Teenage pregnancies, especially among younger teens, are at greater risk of adverse outcomes including early birth, low birth weight, and death of the infant.[12] In the United States 82% of pregnancies in those between 15 and 19 are unplanned.[70] Comprehensive sex education and access to birth control are effective in decreasing pregnancy rates in this age group.[121]
Finances

In the developing world, birth control increases economic growth due to there being fewer dependent children and thus more women participating in or increased contribution to the workforce.[19] Women's earnings, assets, body mass index, and their children's schooling and body mass index all improve with greater access to birth control.[19] Family planning, via the use of modern birth control, is one of the most cost-effective health interventions.[122] For every dollar spent, the United Nations estimates that two to six dollars are saved.[16] These cost savings are related to preventing unplanned pregnancies and decreasing the spread of sexually transmitted illnesses.[122] While all methods are beneficial financially, the use of copper IUDs resulted in the greatest savings.[122]
The total medical cost for a pregnancy, delivery and care of a newborn in the United States is on average $21,000 for a vaginal delivery and $31,000 for a caesarean delivery as of 2012.[123] In most other countries, the cost is less than half.[123] For a child born in 2011, an average US family will spend $235,000 over 17 years to raise them.[124]
Prevalence
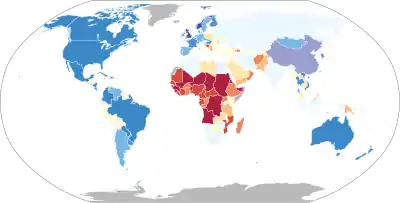
|
6%
12%
18%
24%
|
30%
36%
48%
60%
|
66%
78%
86%
No data
|

Globally, as of 2009, approximately 60% of those who are married and able to have children use birth control.[126] How frequently different methods are used varies widely between countries.[126] The most common method in the developed world is condoms and oral contraceptives, while in Africa it is oral contraceptives and in Latin America and Asia it is sterilization.[126] In the developing world overall, 35% of birth control is via female sterilization, 30% is via IUDs, 12% is via oral contraceptives, 11% is via condoms, and 4% is via male sterilization.[126]
While less used in the developed countries than the developing world, the number of women using IUDs as of 2007 was more than 180 million.[63] Avoiding sex when fertile is used by about 3.6% of women of childbearing age, with usage as high as 20% in areas of South America.[127] As of 2005, 12% of couples are using a male form of birth control (either condoms or a vasectomy) with higher rates in the developed world.[128] Usage of male forms of birth control has decreased between 1985 and 2009.[126] Contraceptive use among women in Sub-Saharan Africa has risen from about 5% in 1991 to about 30% in 2006.[129]
As of 2012, 57% of women of childbearing age want to avoid pregnancy (867 of 1,520 million).[130] About 222 million women however were not able to access birth control, 53 million of whom were in sub-Saharan Africa and 97 million of whom were in Asia.[130] This results in 54 million unplanned pregnancies and nearly 80,000 maternal deaths a year.[126] Part of the reason that many women are without birth control is that many countries limit access due to religious or political reasons,[2] while another contributor is poverty.[131] Due to restrictive abortion laws in Sub-Saharan Africa, many women turn to unlicensed abortion providers for unintended pregnancy, resulting in about 2–4% obtaining unsafe abortions each year.[131]
History
Early history

The Egyptian Ebers Papyrus from 1550 BC and the Kahun Papyrus from 1850 BC have within them some of the earliest documented descriptions of birth control: the use of honey, acacia leaves and lint to be placed in the vagina to block sperm.[132][133] Silphium, a species of giant fennel native to north Africa, may have been used as birth control in ancient Greece and the ancient Near East.[134][135] Due to its supposed desirability, by the first century AD, it had become so rare that it was worth more than its weight in silver and, by late antiquity, it was fully extinct.[134] Most methods of birth control used in antiquity were probably ineffective.[136]
The ancient Greek philosopher Aristotle (c. 384–322 BC) recommended applying cedar oil to the womb before intercourse, a method which was probably only effective on occasion.[136] A Hippocratic text On the Nature of Women recommended that a woman drink a copper salt dissolved in water, which it claimed would prevent pregnancy for a year.[136] This method was not only ineffective, but also dangerous, as the later medical writer Soranus of Ephesus (c. 98–138 AD) pointed out.[136] Soranus attempted to list reliable methods of birth control based on rational principles.[136] He rejected the use of superstition and amulets and instead prescribed mechanical methods such as vaginal plugs and pessaries using wool as a base covered in oils or other gummy substances.[136] Many of Soranus's methods were probably also ineffective.[136]
In medieval Europe, any effort to halt pregnancy was deemed immoral by the Catholic Church,[132] although it is believed that women of the time still used a number of birth control measures, such as coitus interruptus and inserting lily root and rue into the vagina.[137] Women in the Middle Ages were also encouraged to tie weasel testicles around their thighs during sex to prevent pregnancy.[138] The oldest condoms discovered to date were recovered in the ruins of Dudley Castle in England, and are dated back to 1640.[138] They were made of animal gut, and were most likely used to prevent the spread of sexually transmitted diseases during the English Civil War.[138] Casanova, living in 18th century Italy, described the use of a lambskin covering to prevent pregnancy; however, condoms only became widely available in the 20th century.[132]
Birth control movement
The birth control movement developed during the 19th and early 20th centuries.[139] The Malthusian League, based on the ideas of Thomas Malthus, was established in 1877 in the United Kingdom to educate the public about the importance of family planning and to advocate for getting rid of penalties for promoting birth control.[140] It was founded during the "Knowlton trial" of Annie Besant and Charles Bradlaugh, who were prosecuted for publishing on various methods of birth control.[141]
In the United States, Margaret Sanger and Otto Bobsein popularized the phrase "birth control" in 1914.[142][143] Sanger primarily advocated for birth control on the idea that it would prevent women from seeking unsafe abortions, but during her lifetime, she began to campaign for it on the grounds that it would reduce mental and physical defects.[144][145] She was mainly active in the United States but had gained an international reputation by the 1930s. At the time, under the Comstock Law, distribution of birth control information was illegal. She jumped bail in 1914 after her arrest for distributing birth control information and left the United States for the United Kingdom.[146] In the U.K., Sanger, influenced by Havelock Ellis, further developed her arguments for birth control. She believed women needed to enjoy sex without fearing a pregnancy. During her time abroad, Sanger also saw a more flexible diaphragm in a Dutch clinic, which she thought was a better form of contraceptive.[145] Once Sanger returned to the United States, she established a short-lived birth-control clinic with the help of her sister, Ethel Bryne, based in the Brownville section of Brooklyn, New York[147] in 1916. It was shut down after eleven days and resulted in her arrest.[148] The publicity surrounding the arrest, trial, and appeal sparked birth control activism across the United States.[149] Besides her sister, Sanger was helped in the movement by her first husband, William Sanger, who distributed copies of “Family Limitation.” Sanger's second husband, James Noah H. Slee, would also later become involved in the movement, acting as its main funder.[145]
The increased use of birth control was seen by some as a form of social decay.[150] A decrease of fertility was seen as a negative. Throughout the Progressive Era (1890-1920), there was an increase of voluntary associations aiding the contraceptive movement.[150] These organizations failed to enlist more than 100,000 women because the use of birth control was often compared to eugenics;[150] however, there were women seeking a community with like-minded women. The ideology that surrounded birth control started to gain traction during the Progressive Era due to voluntary associations establishing community. Birth control was unlike the Victorian Era because women wanted to manage their sexuality. The use of birth control was another form of self-interest women clung to. This was seen as women began to gravitate towards strong figures, like the Gibson girl.[151]
The first permanent birth-control clinic was established in Britain in 1921 by Marie Stopes working with the Malthusian League.[152] The clinic, run by midwives and supported by visiting doctors,[153] offered women's birth-control advice and taught them the use of a cervical cap. Her clinic made contraception acceptable during the 1920s by presenting it in scientific terms. In 1921, Sanger founded the American Birth Control League, which later became the Planned Parenthood Federation of America.[154] In 1924 the Society for the Provision of Birth Control Clinics was founded to campaign for municipal clinics; this led to the opening of a second clinic in Greengate, Salford in 1926.[155] Throughout the 1920s, Stopes and other feminist pioneers, including Dora Russell and Stella Browne, played a major role in breaking down taboos about sex. In April 1930 the Birth Control Conference assembled 700 delegates and was successful in bringing birth control and abortion into the political sphere – three months later, the Ministry of Health, in the United Kingdom, allowed local authorities to give birth-control advice in welfare centres.[156]
The National Birth Control Association was founded in Britain in 1931, and became the Family Planning Association eight years later. The Association amalgamated several British birth control-focused groups into 'a central organisation' for administering and overseeing birth control in Britain. The group incorporated the Birth Control Investigation Committee, a collective of physicians and scientists that was founded to investigate scientific and medical aspects of contraception with 'neutrality and impartiality'.[157] Subsequently, the Association effected a series of 'pure' and 'applied' product and safety standards that manufacturers must meet to ensure their contraceptives could be prescribed as part of the Association's standard two-part-technique combining ‘a rubber appliance to protect the mouth of the womb’ with a ‘chemical preparation capable of destroying... sperm’.[158] Between 1931 and 1959, the Association founded and funded a series of tests to assess chemical efficacy and safety and rubber quality.[159] These tests became the basis for the Association's Approved List of contraceptives, which was launched in 1937, and went on to become an annual publication that the expanding network of FPA clinics relied upon as a means to 'establish facts [about contraceptives] and to publish these facts as a basis on which a sound public and scientific opinion can be built'.[160]
In 1936 the U.S. court ruled in U.S. v. One Package that medically prescribing contraception to save a person's life or well-being was not illegal under the Comstock Law; following this decision, the American Medical Association Committee on Contraception revoked its 1936 statement condemning birth control. A national survey in 1937 showed 71 percent of the adult population supported the use of contraception. By 1938 347 birth control clinics were running in the United States despite their advertisement still being illegal. First Lady Eleanor Roosevelt publicly supported birth control and family planning.[161] In 1966, President Lyndon B. Johnson started endorsing public funding for family planning services, and the Federal Government began subsidizing birth control services for low-income families.[162] The Affordable Care Act, passed into law on March 23, 2010 under President Barack Obama, requires all plans in the Health Insurance Marketplace to cover contraceptive methods. These include barrier methods, hormonal methods, implanted devices, emergency contraceptives, and sterilization procedures.[163]
Modern methods
In 1909, Richard Richter developed the first intrauterine device made from silkworm gut, which was further developed and marketed in Germany by Ernst Gräfenberg in the late 1920s.[164] In 1951, a chemist, named Carl Djerassi from Mexico City made the hormones in progesterone pills using Mexican yams.[165] Djerassi had chemically created the pill but was not equipped to distribute it to patients. Meanwhile, Gregory Pincus and John Rock with help from the Planned Parenthood Federation of America developed the first birth control pills in the 1950s, such as mestranol/noretynodrel, which became publicly available in the 1960s through the Food and Drug Administration under the name Enovid.[154][166] Medical abortion became an alternative to surgical abortion with the availability of prostaglandin analogs in the 1970s and mifepristone in the 1980s.[167]
Society and culture
Legal positions
Human rights agreements require most governments to provide family planning and contraceptive information and services. These include the requirement to create a national plan for family planning services, remove laws that limit access to family planning, ensure that a wide variety of safe and effective birth control methods are available including emergency contraceptives, make sure there are appropriately trained healthcare providers and facilities at an affordable price, and create a process to review the programs implemented. If governments fail to do the above it may put them in breach of binding international treaty obligations.[168]
In the United States, the 1965 Supreme Court decision Griswold v. Connecticut overturned a state law prohibiting dissemination of contraception information based on a constitutional right to privacy for marital relationships. In 1971, Eisenstadt v. Baird extended this right to privacy to single people.[169]
In 2010, the United Nations launched the Every Woman Every Child movement to assess the progress toward meeting women's contraceptive needs. The initiative has set a goal of increasing the number of users of modern birth control by 120 million women in the world's 69 poorest countries by the year 2020. Additionally, they aim to eradicate discrimination against girls and young women who seek contraceptives.[170] The American Congress of Obstetricians and Gynecologists (ACOG) recommended in 2014 that oral birth control pills should be over the counter medications.[171]
Since at least the 1870s, American religious, medical, legislative, and legal commentators have debated contraception laws. Ana Garner and Angela Michel have found that in these discussions men often attach reproductive rights to moral and political matters, as part of an ongoing attempt to regulate human bodies. In press coverage between 1873–2013 they found a divide between institutional ideology and real-life experiences of women.[172]
Religious views
.jpg.webp)
Religions vary widely in their views of the ethics of birth control.[173] The Roman Catholic Church officially only accepts natural family planning,[174] although large numbers of Catholics in developed countries accept and use modern methods of birth control.[175][176][177] Among Protestants, there is a wide range of views from supporting none, such as in the Quiverfull movement, to allowing all methods of birth control.[178] Views in Judaism range from the stricter Orthodox sect, which prohibits all methods of birth control, to the more relaxed Reform sect, which allows most.[179] Hindus may use both natural and modern contraceptives.[180] A common Buddhist view is that preventing conception is acceptable, while intervening after conception has occurred is not.[181] In Islam, contraceptives are allowed if they do not threaten health, although their use is discouraged by some.[182]
World Contraception Day
September 26 is World Contraception Day, devoted to raising awareness and improving education about sexual and reproductive health, with a vision of a world where every pregnancy is wanted.[183] It is supported by a group of governments and international NGOs, including the Office of Population Affairs, the Asian Pacific Council on Contraception, Centro Latinamericano Salud y Mujer, the European Society of Contraception and Reproductive Health, the German Foundation for World Population, the International Federation of Pediatric and Adolescent Gynecology, International Planned Parenthood Federation, the Marie Stopes International, Population Services International, the Population Council, the United States Agency for International Development (USAID), and Women Deliver.[183]
Misconceptions
There are a number of common misconceptions regarding sex and pregnancy.[184] Douching after sexual intercourse is not an effective form of birth control.[185] Additionally, it is associated with a number of health problems and thus is not recommended.[186] Women can become pregnant the first time they have sexual intercourse[187] and in any sexual position.[188] It is possible, although not very likely, to become pregnant during menstruation.[189]
Accessibility
Access to birth control may be affected by finances and the laws within a region or country.[190] In the United States African American, Hispanic, and young women are disproportionately affected by limited access to birth control, as a result of financial disparity.[191][192] For example Hispanic and African American women often lack insurance coverage and are more often poor.[193] New immigrants in the United States are not offered preventive care such as birth control.[194]
Research directions
Females
Improvements of existing birth control methods are needed, as around half of those who get pregnant unintentionally are using birth control at the time.[27] A number of alterations of existing contraceptive methods are being studied, including a better female condom, an improved diaphragm, a patch containing only progestin, and a vaginal ring containing long-acting progesterone.[195] This vaginal ring appears to be effective for three or four months and is currently available in some areas of the world.[195] For women who rarely have sex, the taking of the hormonal birth control levonorgestrel around the time of sex looks promising.[196]
A number of methods to perform sterilization via the cervix are being studied. One involves putting quinacrine in the uterus which causes scarring and infertility. While the procedure is inexpensive and does not require surgical skills, there are concerns regarding long-term side effects.[197] Another substance, polidocanol, which functions in the same manner is being looked at.[195] A device called Essure, which expands when placed in the fallopian tubes and blocks them, was approved in the United States in 2002.[197] In 2016, a black boxed warning regarding potentially serious side effects was added,[198][199] and in 2018, the device was discontinued.[200]
Males
Methods of male birth control include condoms, vasectomies and withdrawal.[201][202] Between 25 and 75% of males who are sexually active would use hormonal birth control if it was available for them.[128][201] A number of hormonal and non-hormonal methods are in trials,[128] and there is some research looking at the possibility of contraceptive vaccines.[203]
A reversible surgical method under investigation is reversible inhibition of sperm under guidance (RISUG) which consists of injecting a polymer gel, styrene maleic anhydride in dimethyl sulfoxide, into the vas deferens. An injection with sodium bicarbonate washes out the substance and restores fertility. Another is an intravas device which involves putting a urethane plug into the vas deferens to block it. A combination of an androgen and a progestin seems promising, as do selective androgen receptor modulators.[128] Ultrasound and methods to heat the testicles have undergone preliminary studies.[204]
Other animals
Neutering or spaying, which involves removing some of the reproductive organs, is often carried out as a method of birth control in household pets. Many animal shelters require these procedures as part of adoption agreements.[205] In large animals the surgery is known as castration.[206]
Birth control is also being considered as an alternative to hunting as a means of controlling overpopulation in wild animals.[207] Contraceptive vaccines have been found to be effective in a number of different animal populations.[208][209] Kenyan goat herders fix a skirt, called an olor, to male goats to prevent them from impregnating female goats.[210]
References
- 1 2 "Definition of Birth control". MedicineNet. Archived from the original on August 6, 2012. Retrieved August 9, 2012.
- 1 2 3 4 5 6 7 8 9 10 Hanson, S.J.; Burke, Anne E. (2010). "Fertility control: contraception, sterilization, and abortion". In Hurt, K. Joseph; Guile, Matthew W.; Bienstock, Jessica L.; Fox, Harold E.; Wallach, Edward E. (eds.). The Johns Hopkins manual of gynecology and obstetrics (4th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. pp. 382–395. ISBN 978-1-60547-433-5. Archived from the original on 2016-05-12. Retrieved 2020-08-08.
- ↑ Oxford English Dictionary. Oxford University Press. 2012.
- ↑ World Health Organization (WHO). "Family planning". Health topics. World Health Organization (WHO). Archived from the original on March 18, 2016. Retrieved March 28, 2016.
- 1 2 3 4 5 6 World Health Organization Department of Reproductive Health and Research (2011). Family planning: A global handbook for providers: Evidence-based guidance developed through worldwide collaboration (PDF) (Rev. and Updated ed.). Geneva: WHO and Center for Communication Programs. ISBN 978-0-9788563-7-3. Archived (PDF) from the original on September 21, 2013.
- ↑ Taliaferro, L.A.; Sieving, R.; Brady, S.S.; Bearinger, L.H. (2011). "We have the evidence to enhance adolescent sexual and reproductive health—do we have the will?". Adolescent Medicine: State of the Art Reviews. 22 (3): xii, 521–43. PMID 22423463.
- 1 2 Chin, H.B.; Sipe, T.A.; Elder, R.; Mercer, S.L.; Chattopadhyay, S.K.; Jacob, V.; Wethington, H.R.; Kirby, D.; Elliston, D.B. (2012). "The Effectiveness of Group-Based Comprehensive Risk-Reduction and Abstinence Education Interventions to Prevent or Reduce the Risk of Adolescent Pregnancy, Human Immunodeficiency Virus, and Sexually Transmitted Infections". American Journal of Preventive Medicine. 42 (3): 272–94. doi:10.1016/j.amepre.2011.11.006. PMID 22341164. Archived from the original on 2020-01-02. Retrieved 2020-08-08.
- 1 2 3 4 Gizzo, S; Fanelli, T; Di Gangi, S; Saccardi, C; Patrelli, TS; Zambon, A; Omar, A; D'Antona, D; Nardelli, GB (October 2012). "Nowadays which emergency contraception? Comparison between past and present: latest news in terms of clinical efficacy, side effects and contraindications". Gynecological Endocrinology. 28 (10): 758–63. doi:10.3109/09513590.2012.662546. PMID 22390259.
- ↑ Selected practice recommendations for contraceptive use (2nd ed.). Geneva: World Health Organization. 2004. p. 13. ISBN 978-92-4-156284-3. Archived from the original on September 8, 2017.
- ↑ DiCenso A, Guyatt G, Willan A, Griffith L (June 2002). "Interventions to reduce unintended pregnancies among adolescents: systematic review of randomised controlled trials". BMJ. 324 (7351): 1426. doi:10.1136/bmj.324.7351.1426. PMC 115855. PMID 12065267.
- ↑ Duffy, K.; Lynch, D.A.; Santinelli, J. (2008). "Government Support for Abstinence-Only-Until-Marriage Education". Clinical Pharmacology & Therapeutics. 84 (6): 746–48. doi:10.1038/clpt.2008.188. PMID 18923389. Archived from the original on December 11, 2008.
- 1 2 3 Black, A.Y.; Fleming, N.A.; Rome, E.S. (2012). "Pregnancy in adolescents". Adolescent Medicine: State of the Art Reviews. 23 (1): xi, 123–38. PMID 22764559.
- 1 2 Rowan, S.P.; Someshwar, J.; Murray, P. (2012). "Contraception for primary care providers". Adolescent Medicine: State of the Art Reviews. 23 (1): x–xi, 95–110. PMID 22764557.
- 1 2 3 4 5 World Health Organization Department of Reproductive Health and Research (2011). Family planning: A global handbook for providers: Evidence-based guidance developed through worldwide collaboration (PDF) (Rev. and Updated ed.). Geneva: WHO and Center for Communication Programs. pp. 260–300. ISBN 978-0-9788563-7-3. Archived (PDF) from the original on September 21, 2013.
- ↑ "Costs and Benefits of Contraceptive Services: Estimates for 2012" (PDF). United Nations Population Fund. June 2012. p. 1. Archived (PDF) from the original on August 5, 2012.
- 1 2 Carr, B.; Gates, M.F.; Mitchell, A.; Shah, R. (2012). "Giving women the power to plan their families". The Lancet. 380 (9837): 80–82. doi:10.1016/S0140-6736(12)60905-2. PMID 22784540. Archived from the original on May 10, 2013.
- 1 2 3 4 5 6 Cleland, J; Conde-Agudelo, A; Peterson, H; Ross, J; Tsui, A (July 14, 2012). "Contraception and health". Lancet. 380 (9837): 149–56. doi:10.1016/S0140-6736(12)60609-6. PMID 22784533.
- 1 2 Ahmed, S.; Li, Q.; Liu, L.; Tsui, A.O. (2012). "Maternal deaths averted by contraceptive use: An analysis of 172 countries". The Lancet. 380 (9837): 111–25. doi:10.1016/S0140-6736(12)60478-4. PMID 22784531. Archived from the original on May 10, 2013.
- 1 2 3 4 Canning, D.; Schultz, T.P. (2012). "The economic consequences of reproductive health and family planning". The Lancet. 380 (9837): 165–71. doi:10.1016/S0140-6736(12)60827-7. PMID 22784535. Archived from the original on June 2, 2013.
- ↑ Van Braeckel, D.; Temmerman, M.; Roelens, K.; Degomme, O. (2012). "Slowing population growth for wellbeing and development". The Lancet. 380 (9837): 84–85. doi:10.1016/S0140-6736(12)60902-7. PMID 22784542. Archived from the original on May 10, 2013.
- 1 2 3 4 5 6 7 8 9 10 Trussell, James (May 2011). "Contraceptive failure in the United States". Contraception. 83 (5): 397–404. doi:10.1016/j.contraception.2011.01.021. PMC 3638209. PMID 21477680.
Trussell, James (2011). "Contraceptive efficacy". In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 779–863. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734. - ↑ Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, Centers for Disease Control and Prevention (CDC) (June 21, 2013). "U.S. Selected practice recommendations for contraceptive use, 2013: adapted from the World Health Organization Selected practice recommendations for contraceptive use, 2nd edition". MMWR Recommendations and Reports. 62 (5): 1–60. PMID 23784109. Archived from the original on July 10, 2013.
{{cite journal}}: CS1 maint: uses authors parameter (link) - ↑ Van der Wijden, C; Manion, C (12 October 2015). "Lactational amenorrhoea method for family planning". The Cochrane Database of Systematic Reviews (10): CD001329. doi:10.1002/14651858.CD001329.pub2. PMC 6823189. PMID 26457821.
- 1 2 Blenning, CE; Paladine, H (Dec 15, 2005). "An approach to the postpartum office visit". American Family Physician. 72 (12): 2491–96. PMID 16370405.
- ↑ Gordon Edlin; Eric Golanty; Kelli McCormack Brown (2000). Essentials for health and wellness (2nd ed.). Sudbury, MA: Jones and Bartlett. p. 161. ISBN 978-0-7637-0909-9. Archived from the original on June 10, 2016.
- ↑ Edmonds, D. Keith, ed. (2012). Dewhurst's textbook of obstetrics & gynaecology (8th ed.). Chichester, West Sussex: Wiley-Blackwell. p. 508. ISBN 978-0-470-65457-6. Archived from the original on May 3, 2016.
- 1 2 3 4 5 6 7 8 9 Cunningham, F. Gary; Stuart, Gretchen S. (2012). "Contraception and sterilization". In Hoffman, Barbara; Schorge, John O.; Schaffer, Joseph I.; Halvorson, Lisa M.; Bradshaw, Karen D.; Cunningham, F. Gary (eds.). Williams gynecology (2nd ed.). New York: McGraw-Hill Medical. pp. 132–69. ISBN 978-0-07-171672-7.
- ↑ Committee on Adolescence (September 29, 2014). "Contraception for Adolescents". Pediatrics. 134 (4): e1244–56. doi:10.1542/peds.2014-2299. PMC 1070796. PMID 25266430.
- ↑ Mansour, D; Gemzell-Danielsson, K; Inki, P; Jensen, JT (November 2011). "Fertility after discontinuation of contraception: a comprehensive review of the literature". Contraception. 84 (5): 465–77. doi:10.1016/j.contraception.2011.04.002. PMID 22018120.
- 1 2 Organization, World Health (2009). Medical eligibility criteria for contraceptive use (PDF) (4th ed.). Geneva: Reproductive Health and Research, World Health Organization. pp. 1–10. ISBN 978-92-4-156388-8. Archived (PDF) from the original on July 9, 2012.
- ↑ Department of Reproductive Health and Research, Family and Community (2004). Selected practice recommendations for contraceptive use (PDF) (2nd ed.). Geneva: World Health Organization. p. Chapter 31. ISBN 978-92-4-156284-3. Archived (PDF) from the original on July 18, 2013.
- ↑ Tepper, NK; Curtis, KM; Steenland, MW; Marchbanks, PA (May 2013). "Physical examination prior to initiating hormonal contraception: a systematic review". Contraception. 87 (5): 650–54. doi:10.1016/j.contraception.2012.08.010. PMID 23121820. Archived from the original on 2020-08-09. Retrieved 2020-08-08.
- 1 2 3 4 World Health Organization Department of Reproductive Health and Research (2011). Family planning: A global handbook for providers: Evidence-based guidance developed through worldwide collaboration (PDF) (Rev. and Updated ed.). Geneva: WHO and Center for Communication Programs. pp. 1–10. ISBN 978-0-9788563-7-3. Archived (PDF) from the original on September 21, 2013.
- ↑ "American Academy of Family Physicians | Choosing Wisely". www.choosingwisely.org. Archived from the original on 29 July 2020. Retrieved 14 August 2018.
- ↑ Mackenzie, James (December 6, 2013). "The male pill? Bring it on". The Guardian. Archived from the original on May 21, 2014. Retrieved May 20, 2014.
- ↑ Ammer, Christine (2009). "oral contraceptive". The encyclopedia of women's health (6th ed.). New York: Facts On File. pp. 312–15. ISBN 978-0-8160-7407-5. Archived from the original on 2021-03-13. Retrieved 2020-08-08.
- ↑ Nelson, Anita L.; Cwiak, Carrie (2011). "Combined oral contraceptives (COCs)". In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 249–341 [257–58]. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734.
- 1 2 Barbara L. Hoffman (2011). "5 Second-Tier Contraceptive Methods—Very Effective". Williams gynecology (2nd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-171672-7.
- 1 2 3 4 Brito, MB; Nobre, F; Vieira, CS (April 2011). "Hormonal contraception and cardiovascular system". Arquivos Brasileiros de Cardiologia. 96 (4): e81–89. doi:10.1590/S0066-782X2011005000022. PMID 21359483.
- ↑ Stegeman, BH; de Bastos, M; Rosendaal, FR; van Hylckama Vlieg, A; Helmerhorst, FM; Stijnen, T; Dekkers, OM (Sep 12, 2013). "Different combined oral contraceptives and the risk of venous thrombosis: systematic review and network meta-analysis". BMJ (Clinical Research Ed.). 347: f5298. doi:10.1136/bmj.f5298. PMC 3771677. PMID 24030561.
- ↑ Kurver, Miranda J.; van der Wijden, Carla L.; Burgers, Jako (October 4, 2012). "Samenvatting van de NHG-standaard 'Anticonceptie' [Summary of the Dutch College of General Practitioners' practice guideline 'Contraception']". Nederlands Tijdschrift voor Geneeskunde (in Dutch). 156 (41): A5083. PMID 23062257. Archived from the original on April 5, 2020. Retrieved March 15, 2022.
{{cite journal}}: CS1 maint: unrecognized language (link) - ↑ Tosetto, A; et al. (2012). "Predicting disease recurrence in patients with previous unprovoked venous thromboembolism: a proposed prediction score (DASH)". J Thromb Haemost. 10 (6): 1019–25. doi:10.1111/j.1538-7836.2012.04735.x. PMID 22489957.
- ↑ Burrows, LJ; Basha, M; Goldstein, AT (September 2012). "The effects of hormonal contraceptives on female sexuality: a review". The Journal of Sexual Medicine. 9 (9): 2213–23. doi:10.1111/j.1743-6109.2012.02848.x. PMID 22788250.
- 1 2 Shulman, LP (October 2011). "The state of hormonal contraception today: benefits and risks of hormonal contraceptives: combined estrogen and progestin contraceptives". American Journal of Obstetrics and Gynecology. 205 (4 Suppl): S9–13. doi:10.1016/j.ajog.2011.06.057. PMID 21961825.
- ↑ Havrilesky, LJ; Moorman, PG; Lowery, WJ; Gierisch, JM; Coeytaux, RR; Urrutia, RP; Dinan, M; McBroom, AJ; Hasselblad, V; Sanders, GD; Myers, ER (July 2013). "Oral Contraceptive Pills as Primary Prevention for Ovarian Cancer: A Systematic Review and Meta-analysis". Obstetrics and Gynecology. 122 (1): 139–47. doi:10.1097/AOG.0b013e318291c235. PMID 23743450.
- ↑ Mantha, S.; Karp, R.; Raghavan, V.; Terrin, N.; Bauer, K.A.; Zwicker, J.I. (August 7, 2012). "Assessing the risk of venous thromboembolic events in women taking progestin-only contraception: a meta-analysis". BMJ. 345 (aug07 2): e4944. doi:10.1136/bmj.e4944. PMC 3413580. PMID 22872710.
- ↑ Burke, AE (October 2011). "The state of hormonal contraception today: benefits and risks of hormonal contraceptives: progestin-only contraceptives". American Journal of Obstetrics and Gynecology. 205 (4 Suppl): S14–7. doi:10.1016/j.ajog.2011.04.033. PMID 21961819.
- ↑ Rott, H (August 2012). "Thrombotic risks of oral contraceptives". Current Opinion in Obstetrics and Gynecology. 24 (4): 235–40. doi:10.1097/GCO.0b013e328355871d. PMID 22729096.
- 1 2 Neinstein, Lawrence (2008). Adolescent health care : a practical guide (5th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 624. ISBN 978-0-7817-9256-1. Archived from the original on June 17, 2016.
- ↑ Chaudhuri (2007). Practice Of Fertility Control: A Comprehensive Manual (7th ed.). Elsevier India. p. 88. ISBN 978-81-312-1150-2. Archived from the original on April 30, 2016.
- 1 2 Hamilton, Richard (2012). Pharmacology for nursing care (8th ed.). St. Louis, MO: Elsevier/Saunders. p. 799. ISBN 978-1-4377-3582-6. Archived from the original on June 3, 2016.
- ↑ Facts for life (4th ed.). New York: United Nations Children's Fund. 2010. p. 141. ISBN 978-92-806-4466-1. Archived from the original on May 13, 2016.
- ↑ Pray, Walter Steven (2005). Nonprescription product therapeutics (2nd ed.). Philadelphia: Lippincott Williams & Wilkins. p. 414. ISBN 978-0-7817-3498-1. Archived from the original on April 30, 2016.
- ↑ COMMITTEE ON ADOLESCENCE (October 28, 2013). "Condom Use by Adolescents". Pediatrics. 132 (5): 973–81. doi:10.1542/peds.2013-2821. PMID 28448257.
- ↑ Eberhard, Nieschlag (2010). Andrology Male Reproductive Health and Dysfunction (3rd ed.). [S.l.]: Springer-Verlag Berlin Heidelberg. p. 563. ISBN 978-3-540-78355-8. Archived from the original on May 10, 2016.
- ↑ Barbieri, Jerome F. (2009). Yen and Jaffe's reproductive endocrinology : physiology, pathophysiology, and clinical management (6th ed.). Philadelphia: Saunders/Elsevier. p. 873. ISBN 978-1-4160-4907-4. Archived from the original on May 18, 2016.
- ↑ "Preventing Sexually Transmitted Infections (STIs)". British Columbia Health Link. February 2017. Archived from the original on 27 July 2020. Retrieved 31 March 2018.
- ↑ Kuyoh, MA; Toroitich-Ruto, C; Grimes, DA; Schulz, KF; Gallo, MF (January 2003). "Sponge versus diaphragm for contraception: a Cochrane review". Contraception. 67 (1): 15–18. doi:10.1016/s0010-7824(02)00434-1. PMID 12521652.
- ↑ Organization, World Health (2009). Medical eligibility criteria for contraceptive use (4th ed.). Geneva: Reproductive Health and Research, World Health Organization. p. 88. ISBN 978-92-4-156388-8. Archived from the original on May 15, 2016.
- ↑ Winner, B; Peipert, JF; Zhao, Q; Buckel, C; Madden, T; Allsworth, JE; Secura, GM. (2012). "Effectiveness of Long-Acting Reversible Contraception". New England Journal of Medicine. 366 (21): 1998–2007. doi:10.1056/NEJMoa1110855. PMID 22621627. Archived from the original on August 17, 2020. Retrieved August 8, 2020.
- ↑ Hurt, K. Joseph; et al., eds. (March 28, 2012). The Johns Hopkins manual of gynecology and obstetrics. Department of Gynecology and Obstetrics, The Johns Hopkins University School of Medicine, Baltimore Maryland (4th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 232. ISBN 978-1-60547-433-5. Archived from the original on May 12, 2016.
- 1 2 Committee on Adolescent Health Care Long-Acting Reversible Contraception Working Group, The American College of Obstetricians and Gynecologists (October 2012). "Committee opinion no. 539: adolescents and long-acting reversible contraception: implants and intrauterine devices". Obstetrics and Gynecology. 120 (4): 983–88. doi:10.1097/AOG.0b013e3182723b7d. PMID 22996129.
- 1 2 Darney, Leon Speroff, Philip D. (2010). A clinical guide for contraception (5th ed.). Philadelphia: Lippincott Williams & Wilkins. pp. 242–43. ISBN 978-1-60831-610-6. Archived from the original on May 6, 2016.
- ↑ Black, K; Lotke, P; Buhling, KJ; Zite, NB; Intrauterine contraception for Nulliparous women: Translating Research into Action (INTRA), group (October 2012). "A review of barriers and myths preventing the more widespread use of intrauterine contraception in nulliparous women". The European Journal of Contraception & Reproductive Health Care. 17 (5): 340–50. doi:10.3109/13625187.2012.700744. PMC 4950459. PMID 22834648.
- 1 2 3 Gabbe, Steven (2012). Obstetrics: Normal and Problem Pregnancies. Elsevier Health Sciences. p. 527. ISBN 978-1-4557-3395-8. Archived from the original on May 15, 2016.
- ↑ Steenland, MW; Tepper, NK; Curtis, KM; Kapp, N (November 2011). "Intrauterine contraceptive insertion postabortion: a systematic review". Contraception. 84 (5): 447–64. doi:10.1016/j.contraception.2011.03.007. PMID 22018119. Archived from the original on 2020-08-09. Retrieved 2020-08-08.
- ↑ Roe, Andrea Hsu; Bartz, Deborah (2019-01-01). "Society of Family Planning clinical recommendations: contraception after surgical abortion". Contraception. 99 (1): 2–9. doi:10.1016/j.contraception.2018.08.016. ISSN 0010-7824. PMID 30195718. Archived from the original on 2021-08-28. Retrieved 2020-08-08.
- ↑ Tommaso Falcone; William W. Hurd, eds. (2007). Clinical reproductive medicine and surgery. Philadelphia: Mosby. p. 409. ISBN 978-0-323-03309-1. Archived from the original on June 17, 2016.
- ↑ Grimes, D.A. (2007). ""Intrauterine Devices (IUDs)" In:Hatcher, RA; Nelson, TJ; Guest, F; Kowal, D". Contraceptive Technology (19th ed.).
- 1 2 3 Marnach, ML; Long, ME; Casey, PM (March 2013). "Current issues in contraception". Mayo Clinic Proceedings. 88 (3): 295–99. doi:10.1016/j.mayocp.2013.01.007. PMID 23489454.
- ↑ "Popularity Disparity: Attitudes About the IUD in Europe and the United States". Guttmacher Policy Review. 2007. Archived from the original on March 7, 2010. Retrieved April 27, 2010.
- ↑ Cramer, DW (February 2012). "The epidemiology of endometrial and ovarian cancer". Hematology/Oncology Clinics of North America. 26 (1): 1–12. doi:10.1016/j.hoc.2011.10.009. PMC 3259524. PMID 22244658.
- ↑ Adams CE, Wald M (August 2009). "Risks and complications of vasectomy". Urol. Clin. North Am. 36 (3): 331–36. doi:10.1016/j.ucl.2009.05.009. PMID 19643235.
- ↑ Hillard, Paula Adams (2008). The 5-minute obstetrics and gynecology consult. Hagerstwon, MD: Lippincott Williams & Wilkins. p. 265. ISBN 978-0-7817-6942-6. Archived from the original on June 11, 2016.
- ↑ Hillard, Paula Adams (2008). The 5-minute obstetrics and gynecology consult. Hagerstwon, MD: Lippincott Williams & Wilkins. p. 549. ISBN 978-0-7817-6942-6. Archived from the original on May 5, 2016.
- ↑ Hatcher, Robert (2008). Contraceptive technology (19th ed.). New York: Ardent Media. p. 390. ISBN 978-1-59708-001-9. Archived from the original on May 6, 2016.
- ↑ Moore, David S. (2010). The basic practice of statistics (5th ed.). New York: Freeman. p. 25. ISBN 978-1-4292-2426-0. Archived from the original on April 27, 2016.
- 1 2 3 Deffieux, X; Morin Surroca, M; Faivre, E; Pages, F; Fernandez, H; Gervaise, A (May 2011). "Tubal anastomosis after tubal sterilization: a review". Archives of Gynecology and Obstetrics. 283 (5): 1149–58. doi:10.1007/s00404-011-1858-1. PMID 21331539.
- 1 2 Shridharani, A; Sandlow, JI (November 2010). "Vasectomy reversal versus IVF with sperm retrieval: which is better?". Current Opinion in Urology. 20 (6): 503–09. doi:10.1097/MOU.0b013e32833f1b35. PMID 20852426.
- ↑ Nagler, HM; Jung, H (August 2009). "Factors predicting successful microsurgical vasectomy reversal". The Urologic Clinics of North America. 36 (3): 383–90. doi:10.1016/j.ucl.2009.05.010. PMID 19643240.
- 1 2 3 4 Grimes, DA; Gallo, MF; Grigorieva, V; Nanda, K; Schulz, KF (Oct 18, 2004). "Fertility awareness-based methods for contraception". Cochrane Database of Systematic Reviews (4): CD004860. doi:10.1002/14651858.CD004860.pub2. PMID 15495128.
- ↑ Lawrence, Ruth (2010). Breastfeeding : a guide for the medical professional (7th ed.). Philadelphia: Saunders. p. 673. ISBN 978-1-4377-0788-5. Archived from the original on November 16, 2016. Retrieved August 8, 2020.
- 1 2 Freundl, G; Sivin, I; Batár, I (April 2010). "State-of-the-art of non-hormonal methods of contraception: IV. Natural family planning". The European Journal of Contraception & Reproductive Health Care. 15 (2): 113–23. doi:10.3109/13625180903545302. PMID 20141492.
- ↑ Jennings, Victoria H.; Burke, Anne E. (November 1, 2011). "Fertility awareness-based methods". In Hatcher, Robert A.; Trussell, James; Nelson, Anita L.; Cates, Willard Jr.; Kowal, Deborah; Policar, Michael S. (eds.). Contraceptive technology (20th revised ed.). New York: Ardent Media. pp. 417–34. ISBN 978-1-59708-004-0. ISSN 0091-9721. OCLC 781956734.
- ↑ Mangone, Emily Rose; Lebrun, Victoria; Muessig, Kathryn E (19 January 2016). "Mobile Phone Apps for the Prevention of Unintended Pregnancy: A Systematic Review and Content Analysis". JMIR mHealth and uHealth. 4 (1): e6. doi:10.2196/mhealth.4846. PMC 4738182. PMID 26787311.
- 1 2 Organization, World Health (2009). Medical eligibility criteria for contraceptive use (PDF) (4th ed.). Geneva: Reproductive Health and Research, World Health Organization. pp. 91–100. ISBN 978-92-4-156388-8. Archived (PDF) from the original on July 9, 2012.
- 1 2 Jones, RK; Fennell, J; Higgins, JA; Blanchard, K (June 2009). "Better than nothing or savvy risk-reduction practice? The importance of withdrawal". Contraception. 79 (6): 407–10. doi:10.1016/j.contraception.2008.12.008. PMID 19442773.
- ↑ Killick, SR; Leary, C; Trussell, J; Guthrie, KA (March 2011). "Sperm content of pre-ejaculatory fluid". Human Fertility (Cambridge, England). 14 (1): 48–52. doi:10.3109/14647273.2010.520798. PMC 3564677. PMID 21155689.
- 1 2 "Abstinence". Planned Parenthood. 2009. Archived from the original on September 10, 2009. Retrieved September 9, 2009.
- ↑ Murthy, Amitasrigowri S; Harwood, Bryna (2007). Contraception Update (2nd ed.). New York: Springer. pp. Abstract. doi:10.1007/978-0-387-32328-2_12. ISBN 978-0-387-32327-5.
- ↑ Alters, Sandra; Schiff, Wendy (Oct 5, 2009). Essential Concepts for Healthy Living. Jones & Bartlett Publishers. p. 116. ISBN 978-0-7637-5641-3. Archived from the original on 4 August 2020. Retrieved 30 December 2017.
- ↑ Greenberg, Jerrold S.; Bruess, Clint E.; Oswalt, Sara B. (2016). Exploring the Dimensions of Human Sexuality. Jones & Bartlett Publishers. p. 191. ISBN 978-1-4496-9801-0. Archived from the original on 12 August 2020. Retrieved 30 December 2017.
- ↑ Fortenberry, J. Dennis (2005). "The limits of abstinence-only in preventing sexually transmitted infections". Journal of Adolescent Health. 36 (4): 269–70. doi:10.1016/j.jadohealth.2005.02.001. PMID 15780781.
- ↑ Kim Best (2005). "Nonconsensual Sex Undermines Sexual Health". Network. 23 (4). Archived from the original on February 18, 2009.
{{cite journal}}: Cite has empty unknown parameter:|1=(help) - ↑ Francis, Leslie (2017). The Oxford Handbook of Reproductive Ethics. Oxford University Press. p. 329. ISBN 978-0-19-998187-8. Archived from the original on 27 July 2020. Retrieved 30 December 2017.
- ↑ Thomas, R. Murray (2009). Sex and the American teenager seeing through the myths and confronting the issues. Lanham, MD: Rowman & Littlefield Education. p. 81. ISBN 978-1-60709-018-2. Archived from the original on 2016-11-16. Retrieved 2020-08-08.
- ↑ Edlin, Gordon (2012). Health & Wellness. Jones & Bartlett Learning. p. 213. ISBN 978-1-4496-3647-0. Archived from the original on 2016-11-16. Retrieved 2020-08-08.
- 1 2 Santelli, JS; Kantor, LM; Grilo, SA; Speizer, IS; Lindberg, LD; Heitel, J; Schalet, AT; Lyon, ME; Mason-Jones, AJ; McGovern, T; Heck, CJ; Rogers, J; Ott, MA (September 2017). "Abstinence-Only-Until-Marriage: An Updated Review of U.S. Policies and Programs and Their Impact". The Journal of Adolescent Health. 61 (3): 273–80. doi:10.1016/j.jadohealth.2017.05.031. PMID 28842065.
- ↑ Kowal D (2007). "Abstinence and the Range of Sexual Expression". In Hatcher, Robert A.; et al. (eds.). Contraceptive Technology (19th rev. ed.). New York: Ardent Media. pp. 81–86. ISBN 978-0-9664902-0-6.
- ↑ Blackburn, Susan Tucker (2007). Maternal, fetal, & neonatal physiology : a clinical perspective (3rd ed.). St. Louis, MO: Saunders Elsevier. p. 157. ISBN 978-1-4160-2944-1. Archived from the original on May 12, 2016.
- ↑ "WHO 10 facts on breastfeeding". World Health Organization. April 2005. Archived from the original on June 23, 2013.
- ↑ Van der Wijden, Carla; Brown, Julie; Kleijnen, Jos (October 8, 2008). Van Der Wijden, Carla (ed.). "Lactational amenorrhea for family planning". Cochrane Database of Systematic Reviews (4): CD001329. doi:10.1002/14651858.CD001329. PMID 14583931.
- 1 2 3 Fritz, Marc (2012). Clinical Gynecologic Endocrinology and Infertility. pp. 1007–08. ISBN 978-1-4511-4847-3. Archived from the original on June 3, 2016.
- ↑ Swisher, Judith Lauwers, Anna (October 25, 2010). Counseling the nursing mother a lactation consultant's guide (5th ed.). Sudbury, MA: Jones & Bartlett Learning. pp. 465–66. ISBN 978-1-4496-1948-0. Archived from the original on June 16, 2016.
- ↑ Office of Population Research; Association of Reproductive Health Professionals (July 31, 2013). "What is the difference between emergency contraception, the 'morning after pill', and the 'day after pill'?". Princeton: Princeton University. Archived from the original on September 23, 2013. Retrieved September 7, 2013.
- 1 2 Leung, Vivian W Y; Levine, Marc; Soon, Judith A (February 2010). "Mechanisms of Action of Hormonal Emergency Contraceptives". Pharmacotherapy. 30 (2): 158–68. doi:10.1592/phco.30.2.158. PMID 20099990.
The evidence strongly supports disruption of ovulation as a mechanism of action. The data suggest that emergency contraceptives are unlikely to act by interfering with implantation
- 1 2 3 4 Shen, Jie; Che, Yan; Showell, Emily; Chen, Ke; Cheng, Linan (2019-01-20). Cochrane Fertility Regulation Group (ed.). "Interventions for emergency contraception". Cochrane Database of Systematic Reviews. 1: CD001324. doi:10.1002/14651858.CD001324.pub6. PMC 7055045. PMID 30661244.
- ↑ Kripke C (September 2007). "Advance provision for emergency oral contraception". Am Fam Physician. 76 (5): 654. PMID 17894132.
- ↑ Shrader SP, Hall LN, Ragucci KR, Rafie S (September 2011). "Updates in hormonal emergency contraception". Pharmacotherapy. 31 (9): 887–95. doi:10.1592/phco.31.9.887. PMID 21923590.
- ↑ Richardson, AR; Maltz, FN (January 2012). "Ulipristal acetate: review of the efficacy and safety of a newly approved agent for emergency contraception". Clinical Therapeutics. 34 (1): 24–36. doi:10.1016/j.clinthera.2011.11.012. PMID 22154199.
- ↑ "Update on Emergency Contraception". Association of Reproductive Health Professionals. March 2011. Archived from the original on May 11, 2013. Retrieved May 20, 2013.
- ↑ Cleland K, Zhu H, Goldstruck N, Cheng L, Trussel T (2012). "The efficacy of intrauterine devices for emergency contraception: a systematic review of 35 years of experience". Human Reproduction. 27 (7): 1994–2000. doi:10.1093/humrep/des140. PMC 3619968. PMID 22570193.
- ↑ Glasier, A; Cameron, ST; Blithe, D; Scherrer, B; Mathe, H; Levy, D; Gainer, E; Ulmann, A (Oct 2011). "Can we identify women at risk of pregnancy despite using emergency contraception? Data from randomized trials of ulipristal acetate and levonorgestrel". Contraception. 84 (4): 363–67. doi:10.1016/j.contraception.2011.02.009. PMID 21920190.
- ↑ "Dual protection against unwanted pregnancy and HIV / STDs". Sex Health Exch (3): 8. 1998. PMID 12294688.
- 1 2 Cates, W.; Steiner, M.J. (2002). "Dual Protection Against Unintended Pregnancy and Sexually Transmitted Infections: What Is the Best Contraceptive Approach?". Sexually Transmitted Diseases. 29 (3): 168–74. doi:10.1097/00007435-200203000-00007. PMID 11875378.
- ↑ "Statement on Dual Protection against Unwanted Pregnancy and Sexually Transmitted Infections, including HIV". International Planned Parenthood Federation. May 2000. Archived from the original on April 10, 2016.
- ↑ Gupta, Ramesh C. (2011). Reproductive and Developmental Toxicology. Academic Press. p. 105. ISBN 978-0-12-382032-7. Archived from the original on May 16, 2016.
- ↑ Bhakta, J; Bainbridge, J; Borgelt, L (Nov 2015). "Teratogenic medications and concurrent contraceptive use in women of childbearing ability with epilepsy". Epilepsy Behav. 52 (Pt A): 212–17. doi:10.1016/j.yebeh.2015.08.004. PMID 26460786.
- ↑ Country Comparison: Maternal Mortality Rate Archived November 8, 2012, at the Wayback Machine in The CIA World Factbook
- 1 2 Sholapurkar, SL (February 2010). "Is there an ideal interpregnancy interval after a live birth, miscarriage or other adverse pregnancy outcomes?". Journal of Obstetrics and Gynaecology. 30 (2): 107–10. doi:10.3109/01443610903470288. PMID 20143964.
- ↑ Lavin, C; Cox, JE (August 2012). "Teen pregnancy prevention: current perspectives". Current Opinion in Pediatrics. 24 (4): 462–69. doi:10.1097/MOP.0b013e3283555bee. PMID 22790099.
- 1 2 3 Tsui AO, McDonald-Mosley R, Burke AE (April 2010). "Family planning and the burden of unintended pregnancies". Epidemiol Rev. 32 (1): 152–74. doi:10.1093/epirev/mxq012. PMC 3115338. PMID 20570955.
- 1 2 Rosenthal, Elisabeth (June 30, 2013). "American Way of Birth, Costliest in the World". New York Times. Archived from the original on March 14, 2017.
- ↑ "Expenditures on Children by Families, 2011". United States Department of Agriculture, Center for Nutrition Policy and Promotion. Archived from the original on March 8, 2008. Retrieved August 29, 2012.
- ↑ "Demand for family planning satisfied by modern methods". Our World in Data. Archived from the original on 20 August 2020. Retrieved 5 March 2020.
- 1 2 3 4 5 6 Darroch, JE (March 2013). "Trends in contraceptive use". Contraception. 87 (3): 259–63. doi:10.1016/j.contraception.2012.08.029. PMID 23040137.
- ↑ Darney, Leon Speroff, Philip D. (2010). A clinical guide for contraception (5th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 315. ISBN 978-1-60831-610-6.
- 1 2 3 4 Naz, RK; Rowan, S (June 2009). "Update on male contraception". Current Opinion in Obstetrics and Gynecology. 21 (3): 265–69. doi:10.1097/gco.0b013e328329247d. PMID 19469045.
- ↑ Cleland, JG; Ndugwa, RP; Zulu, EM (Feb 1, 2011). "Family planning in sub-Saharan Africa: progress or stagnation?". Bulletin of the World Health Organization. 89 (2): 137–43. doi:10.2471/BLT.10.077925. PMC 3040375. PMID 21346925.
- 1 2 Darroch, JE; Singh, S (May 18, 2013). "Trends in contraceptive need and use in developing countries in 2003, 2008, and 2012: an analysis of national surveys". Lancet. 381 (9879): 1756–62. doi:10.1016/S0140-6736(13)60597-8. PMID 23683642.
- 1 2 Rasch, V (July 2011). "Unsafe abortion and postabortion care – an overview". Acta Obstetricia et Gynecologica Scandinavica. 90 (7): 692–700. doi:10.1111/j.1600-0412.2011.01165.x. PMID 21542813.
- 1 2 3 Cuomo, Amy (2010). "Birth control". In O'Reilly, Andrea (ed.). Encyclopedia of motherhood. Thousand Oaks, CA: Sage Publications. pp. 121–26. ISBN 978-1-4129-6846-1. Archived from the original on 2020-07-27. Retrieved 2020-08-08.
- ↑ Lipsey, Richard G.; Carlaw, Kenneth; Bekar, Clifford (2005). "Historical Record on the Control of Family Size". Economic Transformations: General Purpose Technologies and Long-Term Economic Growth. Oxford University Press. pp. 335–40. ISBN 978-0-19-928564-8. Archived from the original on 2020-07-27. Retrieved 2020-08-08.
- 1 2 unspecified (2001). "Herbal contraceptives and abortifacients". In Bullough, Vern L. (ed.). Encyclopedia of birth control. Santa Barbara, CA: ABC-CLIO. pp. 125–28. ISBN 978-1-57607-181-6. Archived from the original on 2020-07-27. Retrieved 2020-08-08.
- ↑ Totelin, Laurence M.V. (2009). Hippocratic Recipes: Oral and Written Transmission of Pharmacological Knowledge in Fifth- and Fourth-Century Greece. Leiden, Netherlands; Boston: Brill. pp. 158–61. ISBN 978-90-04-17154-1. Archived from the original on 2020-07-27. Retrieved 2020-08-08.
- 1 2 3 4 5 6 7 Carrick, Paul J. (2001). Medical Ethics in Ancient World. Washington, DC: Georgetown University Press. pp. 119–22. ISBN 978-1-58901-861-7. Archived from the original on 2020-07-27. Retrieved 2020-08-08.
- ↑ McTavish, Lianne (2007). "Contraception and birth control". In Robin, Diana (ed.). Encyclopedia of women in the Renaissance : Italy, France, and England. Santa Barbara, CA: ABC-CLIO. pp. 91–92. ISBN 978-1-85109-772-2.
- 1 2 3 "A History of Birth Control Methods" (PDF). Planned Parenthood Report. January 2012. Archived (PDF) from the original on November 6, 2015.
- ↑ Hartmann, B (1997). "Population control I: Birth of an ideology". International Journal of Health Services. 27 (3): 523–40. doi:10.2190/bl3n-xajx-0yqb-vqbx. PMID 9285280.
- ↑ Simms, Madeleine (January 27, 1977). "Review: A History of the Malthusian League 1877–1927". New Scientist. Archived from the original on May 5, 2016.
- ↑ d'Arcy, F (Nov 1977). "The Malthusian League and the resistance to birth control propaganda in late Victorian Britain". Population Studies. 31 (3): 429–48. doi:10.2307/2173367. JSTOR 2173367. PMID 11630505.
- ↑ Wilkinson Meyer, Jimmy Elaine (2004). Any friend of the movement: networking for birth control, 1920–1940. Ohio State University Press. p. 184. ISBN 978-0-8142-0954-7. Archived from the original on January 3, 2014.
- ↑ Galvin, Rachel (1998). "Margaret Sanger's "Deeds of Terrible Virtue"". National Endowment for the Humanities. Archived from the original on October 1, 2013. Retrieved January 27, 2014.
- ↑ Rossi, Alice (1988). The Feminist Papers. Boston: Northeastern University Press. p. 523. ISBN 978-1-55553-028-0.
- 1 2 3 "Biographical Sketch". About Sanger. New York University. Archived from the original on June 28, 2017. Retrieved February 24, 2017.
- ↑ Karen Pastorello (2013). The Progressives: Activism and Reform in American Society, 1893–1917. John Wiley & Sons. p. 65. ISBN 978-1-118-65112-4. Archived from the original on June 4, 2016.
- ↑ Zorea, Aharon (2012). Birth Control. Santa Barbara, CA: Greenwood. p. 43. ISBN 978-0-313-36254-5.
- ↑ Baker, Jean H. (2012). Margaret Sanger : a life of passion (First pbk. ed.). pp. 115–17. ISBN 978-1-4299-6897-3. Archived from the original on May 4, 2016.
- ↑ McCann, Carole Ruth (2010). "Women as Leaders in the Contraceptive Movement". In Karen O'Connor (ed.). Gender and Women's Leadership: A Reference Handbook. Sage. p. 751. ISBN 978-1-84885-583-0. OCLC 568741234. Archived from the original on June 10, 2016.
- 1 2 3 Buenker, John D.; Kantowicz, Edward R., eds. (1988). Historical dictionary of the Progressive Era, 1890-1920. New York: Greenwood Press. ISBN 978-0313243097. OCLC 17807492.
- ↑ McGerr, Michael (2014). A fierce discontent : the rise and fall of the progressive movement in a. Free Press. ISBN 9781439136034. OCLC 893124592.
- ↑ Hall, Ruth (1977). Passionate Crusader. Harcourt, Brace, Jovanovich. p. 186.
- ↑ Marie Carmichael Stopes (1925). The First Five Thousand. London: John Bale, Sons & Danielsson. p. 9. OCLC 12690936.
- 1 2 "Family Planning Timeline". Congressional Digest. 2015.
- ↑ Herbert, Michael (September 5, 2012). "Salford's birth control pioneers". The Guardian. Archived from the original on May 28, 2015. Retrieved May 28, 2015.
- ↑ Hall, Lesley (2011). The life and times of Stella Browne : feminist and free spirit. London: I.B. Tauris. p. 173. ISBN 978-1-84885-583-0.
- ↑ BCIC Memorandum on Proposed Re-organisation [c. 1931]. Wellcome Library, Archives of the Eugenics Society (WL/SA/EUG/D/12/12.)
- ↑ Wright, Helena (1935). Birth Control: Advice on Family Spacing and Healthy Sex Life. London: Cassell's Health Handbooks.
- ↑ Szuhan, Natasha (28 June 2018). "Sex in the laboratory: the Family Planning Association and contraceptive science in Britain, 1929–1959". The British Journal for the History of Science. 51 (3): 487–510. doi:10.1017/S0007087418000481. PMID 29952279.
- ↑ Birth Control Investigation Committee Statement of Intent [c.1927], Wellcome Library, Archives of the Family Planning Association (WL/SA/FPA), WL/SA/FPA/A13/5.
- ↑ Alesha Doan (2007). Opposition and Intimidation: The Abortion Wars and Strategies of Political Harassment. University of Michigan Press. pp. 53–54. ISBN 978-0-472-06975-0.
- ↑ "History of Birth Control in the United States". Congressional Digest. 2012.
- ↑ "Birth control benefits and reproductive health care options in the Health Insurance Marketplace". HealthCare.gov. Archived from the original on February 12, 2016. Retrieved February 17, 2016.
- ↑ Fritz, Marc A.; Speroff, Leon (2011). "Intrauterine contraception". Clinical gynecologic endocrinology and infertility (8th ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. pp. 1095–98. ISBN 978-0-7817-7968-5. Archived from the original on November 16, 2016.
- ↑ "American Experience | The Pill | Timeline". www.pbs.org. Archived from the original on October 1, 2016. Retrieved October 20, 2016.
- ↑ Poston, Dudley (2010). Population and Society: An Introduction to Demography. Cambridge University Press. p. 98. ISBN 978-1-139-48938-6. Archived from the original on November 16, 2016.
- ↑ Kulier, Regina; Kapp, Nathalie; Gülmezoglu, A. Metin; Hofmeyr, G. Justus; Cheng, Linan; Campana, Aldo (November 9, 2011). "Medical methods for first trimester abortion". Cochrane Database of Systematic Reviews (11): CD002855. doi:10.1002/14651858.CD002855.pub4. PMC 7144729. PMID 22071804.
- ↑ Cottingham J.; Germain A.; Hunt P. (2012). "Use of human rights to meet the unmet need for family planning". The Lancet. 380 (9837): 172–80. doi:10.1016/S0140-6736(12)60732-6. PMID 22784536.
{{cite journal}}: Cite has empty unknown parameter:|1=(help) - ↑ Alesha Doan (2007). Opposition and Intimidation: The Abortion Wars and Strategies of Political Harassment. University of Michigan Press. pp. 62–63. ISBN 978-0-472-06975-0.
- ↑ Susheela Singh; Jacqueline E. Darroch (June 2012). "Adding It Up: Costs and Benefits of Contraceptive Services Estimates for 2012" (PDF). Guttmacher Institute and United Nations Population Fund (UNFPA), 201. Archived (PDF) from the original on August 5, 2012.
- ↑ ACOG (September 9, 2014). "ACOG Statement on OTC Access to Contraception". Archived from the original on September 10, 2014. Retrieved September 11, 2014.
- ↑ Garner, A.C.; Michel, A.R. (4 November 2016). ""The Birth Control Divide": U.S. Press Coverage of Contraception, 1873–2013". Journalism & Communication Monographs. 18 (4): 180–234. doi:10.1177/1522637916672457.
- ↑ Srikanthan, A; Reid, RL (February 2008). "Religious and cultural influences on contraception". Journal of Obstetrics and Gynaecology Canada. 30 (2): 129–37. doi:10.1016/s1701-2163(16)32736-0. PMID 18254994.
- ↑ Pope Paul VI (July 25, 1968). "Humanae Vitae: Encyclical of Pope Paul VI on the Regulation of Birth". Vatican. Archived from the original on August 24, 2000. Retrieved October 1, 2006.
- ↑ Rosemary Radford Ruether (2006). "Women in North American Catholicism". In Rosemary Skinner Keller (ed.). Encyclopedia of women and religion in North America. Bloomington, IN [u.a.]: Indiana Univ. Press. p. 132. ISBN 978-0-253-34686-5. Archived from the original on May 29, 2016.
- ↑ Bob Digby; et al. (2001). Bob Digby (ed.). Heinemann 16–19 Geography: Global Challenges Student Book (2nd ed.). Heinemann. p. 158. ISBN 978-0-435-35249-3. Archived from the original on May 12, 2016.
- ↑ Rengel, Marian (2000). Encyclopedia of birth control. Phoenix, AZ: Oryx Press. p. 202. ISBN 978-1-57356-255-3. Archived from the original on June 3, 2016.
- ↑ Bennett, Jana Marguerite (2008). Water is thicker than blood : an Augustinian theology of marriage and singleness. Oxford: Oxford University Press. p. 178. ISBN 978-0-19-531543-1. Archived from the original on May 28, 2016.
- ↑ Feldman, David M. (1998). Birth Control in Jewish Law. Lanham, MD: Jason Aronson. ISBN 978-0-7657-6058-6.
- ↑ "Hindu Beliefs and Practices Affecting Health Care". University of Virginia Health System. Archived from the original on March 23, 2004. Retrieved October 6, 2006.
- ↑ "More Questions & Answers on Buddhism: Birth Control and Abortion". Alan Khoo. Archived from the original on June 29, 2008. Retrieved June 14, 2008.
- ↑ Khalid Farooq Akbar. "Family Planning and Islam: A Review". Hamdard Islamicus. XVII (3). Archived from the original on September 26, 2006.
- 1 2 "World Contraception Day". Archived from the original on August 18, 2014.
- ↑ Hutcherson, Hilda (2002). What your mother never told you about s.e.x (1st Perigee ed.). New York: Perigee Book. p. 201. ISBN 978-0-399-52853-8. Archived from the original on June 29, 2016.
- ↑ Rengel, Marian (2000). Encyclopedia of birth control. Phoenix, AZ: Oryx Press. p. 65. ISBN 978-1-57356-255-3. Archived from the original on May 6, 2016.
- ↑ Cottrell, BH (Mar–Apr 2010). "An updated review of evidence to discourage douching". MCN: The American Journal of Maternal/Child Nursing. 35 (2): 102–07, quiz 108–09. doi:10.1097/NMC.0b013e3181cae9da. PMID 20215951.
- ↑ Alexander, William (2013). New Dimensions In Women's Health – Book Alone (6th ed.). Jones & Bartlett Publishers. p. 105. ISBN 978-1-4496-8375-7. Archived from the original on May 6, 2016.
- ↑ Sharkey, Harriet (2013). Need to Know Fertility and Conception and Pregnancy. HarperCollins. p. 17. ISBN 978-0-00-751686-5. Archived from the original on June 3, 2016.
- ↑ Strange, Mary (2011). Encyclopedia of women in today's world. Thousand Oaks, CA: Sage Reference. p. 928. ISBN 978-1-4129-7685-5. Archived from the original on May 15, 2016.
- ↑ "Access to Contraception - ACOG". www.acog.org. Archived from the original on 2020-07-27. Retrieved 2020-08-08.
- ↑ "Who's Impacted by Attacks on Birth Control". www.plannedparenthoodaction.org. Archived from the original on 27 July 2020. Retrieved 15 October 2019.
- ↑ Pregnancy, Institute of Medicine (US) Committee on Unintended; Brown, Sarah S.; Eisenberg, Leon (1995). Socioeconomic and Cultural Influences on Contraceptive Use. National Academies Press (US). Archived from the original on 2021-08-28. Retrieved 2020-08-08.
- ↑ "Just the Facts: Latinas & Contraception" (PDF). Archived (PDF) from the original on 26 September 2020. Retrieved 25 March 2020.
- ↑ Dehlendorf, Christine; Rodriguez, Maria Isabel; Levy, Kira; Borrero, Sonya; Steinauer, Jody (March 2010). "Disparities in family planning". American Journal of Obstetrics and Gynecology. 202 (3): 214–220. doi:10.1016/j.ajog.2009.08.022. PMC 2835625. PMID 20207237.
- 1 2 3 Jensen, JT (October 2011). "The future of contraception: innovations in contraceptive agents: tomorrow's hormonal contraceptive agents and their clinical implications". American Journal of Obstetrics and Gynecology. 205 (4 Suppl): S21–5. doi:10.1016/j.ajog.2011.06.055. PMID 21961821.
- ↑ Halpern, V; Raymond, EG; Lopez, LM (Sep 26, 2014). "Repeated use of pre- and postcoital hormonal contraception for prevention of pregnancy". The Cochrane Database of Systematic Reviews. 9 (9): CD007595. doi:10.1002/14651858.CD007595.pub3. PMC 7196890. PMID 25259677.
- 1 2 Castaño, PM; Adekunle, L (March 2010). "Transcervical sterilization". Seminars in Reproductive Medicine. 28 (2): 103–09. doi:10.1055/s-0030-1248134. PMID 20352559.
- ↑ Rabin, Roni Caryn (2016-11-21). "Bayer's Essure Contraceptive Implant, Now With a Warning". The New York Times. ISSN 0362-4331. Archived from the original on 2020-08-12. Retrieved 2020-05-01.
- ↑ Commissioner, Office of the (2020-03-24). "FDA takes additional action to better understand safety of Essure, inform patients of potential risks". FDA. Archived from the original on 2020-08-04. Retrieved 2020-05-01.
- ↑ Kaplan, Sheila (2018-07-20). "Bayer Will Stop Selling the Troubled Essure Birth Control Implants". The New York Times. ISSN 0362-4331. Archived from the original on 2020-10-16. Retrieved 2020-05-01.
- 1 2 Glasier, A (November 2010). "Acceptability of contraception for men: a review". Contraception. 82 (5): 453–56. doi:10.1016/j.contraception.2010.03.016. PMID 20933119.
- ↑ Kogan, P; Wald, M (Feb 2014). "Male contraception: history and development". The Urologic Clinics of North America. 41 (1): 145–61. doi:10.1016/j.ucl.2013.08.012. PMID 24286773.
- ↑ Naz, RK (July 2011). "Antisperm contraceptive vaccines: where we are and where we are going?". American Journal of Reproductive Immunology (New York: 1989). 66 (1): 5–12. doi:10.1111/j.1600-0897.2011.01000.x. PMC 3110624. PMID 21481057.
- ↑ William J. Kovacs; Sergio R. Ojeda, eds. (2011). Textbook of endocrine physiology (6th ed.). Oxford: Oxford University Press. p. 262. ISBN 978-0-19-974412-1. Archived from the original on June 9, 2016.
- ↑ Millar, Lila (2011). Infectious Disease Management in Animal Shelters. John Wiley & Sons. ISBN 978-1-119-94945-9. Archived from the original on May 3, 2016.
- ↑ Ackerman, Lowell, ed. (2007). Blackwell's five-minute veterinary practice management consult (1st ed.). Ames, IO: Blackwell Pub. p. 80. ISBN 978-0-7817-5984-7. Archived from the original on June 10, 2016.
- ↑ Boyle, Rebecca (March 3, 2009). "Birth control for animals: a scientific approach to limiting the wildlife population explosion". Popular Science. New York: PopSci.com. Archived from the original on May 25, 2012.
- ↑ Kirkpatrick, JF; Lyda, RO; Frank, KM (July 2011). "Contraceptive vaccines for wildlife: a review". American Journal of Reproductive Immunology (New York: 1989). 66 (1): 40–50. doi:10.1111/j.1600-0897.2011.01003.x. PMID 21501279.
- ↑ Levy, JK (July 2011). "Contraceptive vaccines for the humane control of community cat populations". American Journal of Reproductive Immunology (New York: 1989). 66 (1): 63–70. doi:10.1111/j.1600-0897.2011.01005.x. PMC 5567843. PMID 21501281.
- ↑ "Goat 'condoms' save Kenyan herds". BBC News. October 6, 2008. Archived from the original on October 6, 2008. Retrieved October 6, 2008.
Further reading
- Speroff, Leon; Darney, Philip D. (2010). A clinical guide for contraception Archived 2020-07-27 at the Wayback Machine (5th ed.). Philadelphia: Lippincott Williams & Wilkins. ISBN 978-1-60831-610-6.
- Stubblefield, Phillip G.; Roncari, Danielle M. (2011). "Family Planning" Archived 2020-08-03 at the Wayback Machine, pp. 211–69, in Berek, Jonathan S. (ed.) Berek & Novak's Gynecology, 15th ed. Philadelphia: Lippincott Williams & Wilkins, ISBN 978-1-4511-1433-1.
- Jensen, Jeffrey T.; Mishell, Daniel R. Jr. (March 19, 2012). "Family Planning: Contraception, Sterilization, and Pregnancy Termination" Archived 2020-07-27 at the Wayback Machine, pp. 215–72, in Lentz, Gretchen M.; Lobo, Rogerio A.; Gershenson, David M.; Katz, Vern L. (eds.) Comprehensive Gynecology, 6th ed. Philadelphia: Mosby Elsevier, ISBN 978-0-323-06986-1.
- Gavin, L; Moskosky, S; Carter, M; Curtis, K; Glass, E (Apr 25, 2014). Godfrey, E; Marcell, A; Mautone-Smith, N; Pazol, K; Tepper, N; Zapata, L; Division of Reproductive Health, National Center for Chronic Disease Prevention and Health Promotion, CDC. "Providing Quality Family Planning Services: Recommendations of CDC and the U.S. Office of Population Affairs". MMWR Recommendations and Reports. 63 (RR-04): 1–54. PMID 24759690.
External links
| Library resources about Birth control |
- Birth control at Curlie
- "WHO Fact Sheet". July 2017. Archived from the original on 19 April 2018. Retrieved 23 July 2017.
- World Health Organization Department of Reproductive Health and Research and Johns Hopkins Bloomberg School of Public Health (2011). Family planning: A global handbook for providers: Evidence-based guidance developed through worldwide collaboration (PDF) (Rev. and Updated ed.). Geneva: WHO and Center for Communication Programs. ISBN 978-0-9788563-7-3. Archived (PDF) from the original on 2013-09-21. Retrieved 2020-08-08.
- Curtis, Kathryn M.; Jatlaoui, Tara C.; Tepper, Naomi K.; Zapata, Lauren B.; Horton, Leah G.; Jamieson, Denise J.; Whiteman, Maura K. (29 July 2016). "U.S. Selected Practice Recommendations for Contraceptive Use". MMWR Recommendations and Reports. 65 (4): 1–66. doi:10.15585/mmwr.rr6504a1. PMID 27467319.
- "Birth Control Comparison Chart". Cedar River Clinics. Archived from the original on 2014-03-29. Retrieved 2020-08-08.
- Bulk procurement of birth control Archived 2014-03-03 at the Wayback Machine by the World Health Organization