Variants of SARS-CoV-2
| Part of a series on the |
| COVID-19 pandemic |
|---|
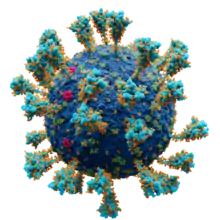 Scientifically accurate atomic model of the external structure of SARS-CoV-2. Each "ball" is an atom. |
|
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2), the virus that causes coronavirus disease 2019 (COVID-19), has many variants; some are believed, or have been believed, to be of particular importance due to their potential for increased transmissibility,[1] increased virulence, or reduced effectiveness of vaccines against them.[2][3] This article discusses such notable variants of SARS-CoV-2 and notable missense mutations found in these variants.
Overview
Although the emergence of SARS-CoV-2 may have resulted from recombination events between a bat SARS-like coronavirus and a pangolin coronavirus (through cross-species transmission),[4] mutations have been shown to play an important role in the ongoing evolution and emergence of novel SARS-CoV-2 variants.[1]
The variant first sampled and identified in China is considered by researchers to differ from the progenitor genome "by three variants".[5][6] Subsequently, many distinct lineages of SARS-CoV-2 have evolved.[7]
Modern DNA sequencing, where available, may permit rapid detection (sometimes known as 'real-time detection') of genetic variants that appear in pathogens during disease outbreaks.[8] Through use of phylogenetic tree visualization software, records of genome sequences can be clustered into groups of identical genomes all containing the same set of mutations. Each group represents a 'variant', 'clade', or 'lineage', and comparison of the sequences allows the evolutionary path of a virus to be deduced. For SARS-CoV-2, over 330,000 viral genomic sequences have been generated by molecular epidemiology studies across the world.[9]
SARS-CoV-2 is evolving to become more transmissible. Notably the Alpha variant and the Delta variant are both more transmissible than the original virus identified round Wuhan in China.[10]
The following table presents information and level of risk for variants with elevated or possibly elevated risk at present.[11][12][13][14][15][16][17] The intervals assume a 95% confidence or credibility level, unless otherwise stated. Currently, all estimates are approximations due to the limited availability of data for studies.
Table/Variants of SARS-CoV-2 | |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
|
Relative risk level: Very high High Medium Low Unknown
| |||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||
Nomenclature
| PANGO lineages[54] | Notes to PANGO lineages[55] | Nextstrain clades,[56] 2021[57] | GISAID clades | Notable variants |
|---|---|---|---|---|
| A.1–A.6 | 19B | S | Contains "reference sequence" WIV04/2019[58] | |
| B.3–B.7, B.9, B.10, B.13–B.16 | 19A | L | ||
| O[lower-alpha 1] | ||||
| B.2 | V | |||
| B.1 | B.1.5–B.1.72 | 20A | G | Lineage B.1 in the PANGO Lineages nomenclature system; includes Delta/ |
| B.1.9, B.1.13, B.1.22, B.1.26, B.1.37 | GH | |||
| B.1.3–B.1.66 | 20C | Includes Epsilon/ | ||
| 20G | Predominant in US generally, Jan '21[60] | |||
| 20H | Includes Beta/ | |||
| B.1.1 | 20B | GR | Includes B.1.1.207 | |
| 20D | ||||
| 20J | Includes Gamma/ | |||
| 20F | ||||
| 20I | Includes Alpha/ | |||
| B.1.177 | 20E (EU1)[57] | GV[lower-alpha 1] | Derived from 20A[57] | |

No consistent nomenclature has been established for SARS-CoV-2.[64] Colloquially, including by governments and news organizations, concerning variants are often referred to by the country in which they were first identified.[65][66][67] After months of discussions, the World Health Organization announced Greek-letter names for important strains on 31 May 2021, so they could be easily referred to in a geographically and politically neutral fashion.[68][69]

While there are many thousands of variants of SARS-CoV-2,[70] subtypes of the virus can be put into larger groupings such as lineages or clades.[lower-alpha 2] Three main, generally used nomenclatures[64] have been proposed:
- As of January 2021, GISAID – referring to SARS-CoV-2 as hCoV-19[55] – had identified eight global clades (S, O, L, V, G, GH, GR, and GV).[71]
- In 2017, Hadfield et al. announced Nextstrain, intended "for real-time tracking of pathogen evolution".[72] Nextstrain has later been used for tracking SARS-CoV-2, identifying 13 major clades[lower-alpha 3] (19A–B, 20A–20J and 21A) as of June 2021.[73]
- In 2020, Rambaut et al. of the Phylogenetic Assignment of Named Global Outbreak Lineages (PANGOLIN)[74] software team proposed in an article[54] "a dynamic nomenclature for SARS-CoV-2 lineages that focuses on actively circulating virus lineages and those that spread to new locations";[64] as of February 2021, six major lineages (A, B, B.1, B.1.1, B.1.177, B.1.1.7) had been identified.[7][75]
Each national public health institute may also institute its own nomenclature system for the purposes of tracking specific variants. For example, Public Health England designated each tracked variant by year, month and number in the format [YYYY] [MM]/[NN], prefixing 'VUI' or 'VOC' for a variant under investigation or a variant of concern respectively.[13] This system has now been modified and now uses the format [YY] [MMM]-[NN], where the month is written out using a three-letter code.[13]
Reference sequence
As it is currently not known when the index case or 'patient zero' occurred, the choice of reference sequence for a given study is relatively arbitrary, with different notable research studies' choices varying as follows:
- The earliest sequence, Wuhan-1, was collected on 24 December 2019.[5]
- One group (Sudhir Kumar et al.)[5] refers extensively to an NCBI reference genome (GenBankID:NC_045512; GISAID ID: EPI_ISL_402125),[76] this sample was collected on 26 December 2019,[77] although they also used the WIV04 GISAID reference genome (ID: EPI_ISL_402124),[78] in their analyses.[79]
- According to another source (Zhukova et al.), the sequence WIV04/2019, belonging to the GISAID S clade / PANGO A lineage / Nextstrain 19B clade, is thought to most closely reflect the sequence of the original virus infecting humans—known as "sequence zero".[58] WIV04/2019 was sampled from a symptomatic patient on 30 December 2019 and is widely used (especially by those collaborating with GISAID)[80] as a reference sequence.[58]
Criteria for notability
Viruses generally acquire mutations over time, giving rise to new variants. When a new variant appears to be growing in a population, it can be labeled as an "emerging variant".
Some of the potential consequences of emerging variants are the following:[22][81]
- Increased transmissibility
- Increased morbidity
- Increased mortality
- Ability to evade detection by diagnostic tests
- Decreased susceptibility to antiviral drugs (if and when such drugs are available)
- Decreased susceptibility to neutralizing antibodies, either therapeutic (e.g., convalescent plasma or monoclonal antibodies) or in laboratory experiments
- Ability to evade natural immunity (e.g., causing reinfections)
- Ability to infect vaccinated individuals
- Increased risk of particular conditions such as multisystem inflammatory syndrome or long-haul COVID.
- Increased affinity for particular demographic or clinical groups, such as children or immunocompromised individuals.
Variants that appear to meet one or more of these criteria may be labeled "variants under investigation" or "variants of interest" pending verification and validation of these properties. The primary characteristic of a variant of interest is that it shows evidence that demonstrates it is the cause of an increased proportion of cases or unique outbreak clusters; however, it must also have limited prevalence or expansion at national levels, or the classification would be elevated to a "variant of concern".[13][82] If there is clear evidence that the effectiveness of prevention or intervention measures for a particular variant is substantially reduced, that variant is termed a "variant of high consequence".[12]
Variants of Concern (WHO)
Listed below are the Variants of Concern (VOC) currently recognised by the World Health Organization[11]. Note that other organizations such as the CDC in the United States may use a slightly different list.[12]
Alpha (lineage B.1.1.7)
_(cropped).jpg.webp)
First detected in October 2020 during the COVID-19 pandemic in the United Kingdom from a sample taken the previous month in Kent,[83] lineage B.1.1.7,[84] labelled Alpha variant by the WHO, was previously known as the first Variant Under Investigation in December 2020 (VUI – 202012/01)[85] and later notated as VOC-202012/01.[13] It is also known as 20I (V1),[18] 20I/501Y.V1[86] (formerly 20B/501Y.V1),[87][88][22] or 501Y.V1.[40] Since then, its prevalence odds have doubled every 6.5 days, the presumed generational interval.[89][90] It is correlated with a significant increase in the rate of COVID-19 infection in United Kingdom, associated partly with the N501Y mutation.[91] There is some evidence that this variant has 40–80% increased transmissibility (with most estimates lying around the middle to higher end of this range),[92] and early analyses suggest an increase in lethality.[93][94] More recent work has found no evidence of increased virulence.[95] As of May 2021, the Alpha variant has been detected in some 120 countries.[96]
B.1.1.7 with E484K
Variant of Concern 21FEB-02 (previously written as VOC-202102/02), described by Public Health England (PHE) as "B.1.1.7 with E484K"[13] is of the same lineage in the Pango nomenclature system, but has an additional E484K mutation. As of 17 March 2021, there are 39 confirmed cases of VOC-21FEB-02 in the UK.[13] On 4 March 2021, scientists reported B.1.1.7 with E484K mutations in the state of Oregon. In 13 test samples analysed, one had this combination, which appeared to have arisen spontaneously and locally, rather than being imported.[97][98][99] Other names for this variant include B.1.1.7+E484K[100] and B.1.1.7 Lineage with S:E484K.[101]
Beta (lineage B.1.351)
On 18 December 2020, the 501.V2 variant, also known as 501.V2, 20H (V2),[18] 20H/501Y.V2[86] (formerly 20C/501Y.V2), 501Y.V2,[27] VOC-20DEC-02 (formerly VOC-202012/02), or lineage B.1.351,[22] was first detected in South Africa and reported by the country's health department.[102] It has been labelled as Beta variant by WHO. Researchers and officials reported that the prevalence of the variant was higher among young people with no underlying health conditions, and by comparison with other variants it is more frequently resulting in serious illness in those cases.[103][104] The South African health department also indicated that the variant may be driving the second wave of the COVID-19 epidemic in the country due to the variant spreading at a more rapid pace than other earlier variants of the virus.[102][103]
Scientists noted that the variant contains several mutations that allow it to attach more easily to human cells because of the following three mutations in the receptor-binding domain (RBD) in the spike glycoprotein of the virus: N501Y,[102][105] K417N, and E484K.[106][107] The N501Y mutation has also been detected in the United Kingdom.[102][108]
Gamma (lineage P.1)
The Gamma variant or lineage P.1, termed Variant of Concern 21JAN-02[13] (formerly VOC-202101/02) by Public Health England,[13] 20J (V3)[18] or 20J/501Y.V3[86] by Nextstrain, or just 501Y.V3,[40] was detected in Tokyo on 6 January 2021 by the National Institute of Infectious Diseases (NIID). It has been labelled as Gamma variant by WHO. The new variant was first identified in four people who arrived in Tokyo having travelled from the Brazilian Amazonas state on 2 January 2021.[109] On 12 January 2021, the Brazil-UK CADDE Centre Archived 24 June 2021 at the Wayback Machine confirmed 13 local cases of the new Gamma variant in the Amazon rain forest.[110] This variant of SARS-CoV-2 has been named lineage P.1 (although it is a descendant of B.1.1.28, the name B.1.1.28.1[111][14] is not permitted and thus the resultant name is P.1), and has 17 unique amino acid changes, 10 of which in its spike protein, including the three concerning mutations: N501Y, E484K and K417T.[110][112][113][114]: Figure 5
The N501Y and E484K mutations favour the formation of a stable RBD-hACE2 complex, thus, enhancing the binding affinity of RBD to hACE2. However, the K417T mutation disfavours complex formation between RBD and hACE2, which has been demonstrated to reduce the binding affinity.[1]
The new variant was absent in samples collected from March to November 2020 in Manaus, Amazonas state, but it was detected for the same city in 42% of the samples from 15–23 December 2020, followed by 52.2% during 15–31 December and 85.4% during 1–9 January 2021.[110] A study found that infections by Gamma can produce nearly ten times more viral load compared to persons infected by one of the other lineages identified in Brazil (B.1.1.28 or B.1.195). Gamma also showed 2.2 times higher transmissibility with the same ability to infect both adults and older persons, suggesting P.1 and P.1-like lineages are more successful at infecting younger humans irrespective of sex.[115]
A study of samples collected in Manaus between November 2020 and January 2021, indicated that the Gamma variant is 1.4–2.2 times more transmissible and was shown to be capable of evading 25–61% of inherited immunity from previous coronavirus diseases, leading to the possibility of reinfection after recovery from an earlier COVID-19 infection. As for the fatality ratio, infections by Gamma were also found to be 10–80% more lethal.[116][117][35]
A study found that people fully vaccinated with Pfizer or Moderna have significantly decreased neutralization effect against Gamma, although the actual impact on the course of the disease is uncertain.[118] A pre-print study by the Oswaldo Cruz Foundation published in early April found that the real-world performance of people with the initial dose of the Sinovac's Coronavac Vaccine had approximately 50% efficacy rate. They expected the efficacy to be higher after the 2nd dose. The study is ongoing.[119]
Preliminary data from two studies indicate that the Oxford–AstraZeneca vaccine is effective against the Gamma variant, although the exact level of efficacy has not yet been released.[120][121] Preliminary data from a study conducted by Instituto Butantan suggest that CoronaVac is effective against the Gamma variant as well, and the study will be expanded to obtain definitive data.[122]
Delta (lineage B.1.617.2)
The Delta variant, also known as B.1.617.2, G/452R.V3, 21A[18] or 21A/S:478K,[86] was first discovered in India. Descendant of lineage B.1.617, which also includes the Kappa variant under investigation, it was first discovered in October 2020 and has since spread internationally.[123][124][125][126][127] On 6 May 2021, British scientists declared B.1.617.2 (which notably lacks mutation at E484Q) as a "variant of concern", labelling it VOC-21APR-02, after they flagged evidence that it spreads more quickly than the original version of the virus and could spread as quickly as Alpha.[128][129][130] It carries L452R, T478K and P681R mutations,[45] but unlike Kappa it does not carry E484Q.
On 3 June 2021, Public Health England reported that twelve of the 42 deaths from the Delta variant in England were among the fully vaccinated, and that it was spreading almost twice as fast as the Alpha variant.[131] Also on 11 June, Foothills Medical Centre in Calgary, Canada reported that half of their 22 cases of the Delta variant occurred among the fully vaccinated.[132]
On 14 June 2021, India detected a mutated variant of B.1.617.2 or Delta variant which is known as AY.1 or 'Delta Plus' variant.[133]
Variants of Interest (WHO)
Listed below are the Variants of Interest (VOI) currently recognised by the World Health Organization<[11]. Note that other organizations such as the CDC in the United States may use a slightly different list. For example, they designate Epsilon as a VOC rather than a VOI.[12]
Epsilon (lineages B.1.429, B.1.427, CAL.20C)
The Epsilon variant or lineage B.1.429, also known as CAL.20C[134] or CA VUI1,[135] 21C[18] or 20C/S:452R,[86] is defined by five distinct mutations (I4205V and D1183Y in the ORF1ab-gene, and S13I, W152C, L452R in the spike protein's S-gene), of which the L452R (previously also detected in other unrelated lineages) was of particular concern.[60][136] B.1.429 is possibly more transmissible, but further study is necessary to confirm this.[136] CDC has listed B.1.429 and the related B.1.427 as "variants of concern," and cites a preprint for saying that they exhibit a ~20% increase in viral transmissibility, have a "Significant impact on neutralization by some, but not all," therapeutics that have been given Emergency Use Authorization (EUA) by FDA for treatment or prevention of COVID-19, and moderately reduce neutralization by plasma collected by people who have previously infected by the virus or who have received a vaccine against the virus.[137][138] According to WHO, it has been labelled as Epsilon variant.
Epsilon (CAL.20C) was first observed in July 2020 by researchers at the Cedars-Sinai Medical Center, California, in one of 1,230 virus samples collected in Los Angeles County since the start of the COVID-19 epidemic.[139] It was not detected again until September when it reappeared among samples in California, but numbers remained very low until November.[140][141] In November 2020, the Epsilon variant accounted for 36 percent of samples collected at Cedars-Sinai Medical Center, and by January 2021, the Epsilon variant accounted for 50 percent of samples.[136] In a joint press release by University of California, San Francisco, California Department of Public Health, and Santa Clara County Public Health Department,[142] the variant was also detected in multiple counties in Northern California. From November to December 2020, the frequency of the variant in sequenced cases from Northern California rose from 3% to 25%.[143] In a preprint, CAL.20C is described as belonging to clade 20C and contributing approximately 36% of samples, while an emerging variant from the 20G clade accounts for some 24% of the samples in a study focused on Southern California. Note however that in the US as a whole, the 20G clade predominates, as of January 2021.[60] Following the increasing numbers of Epsilon in California, the variant has been detected at varying frequencies in most US states. Small numbers have been detected in other countries in North America, and in Europe, Asia and Australia.[140][141] After an initial increase, its frequency rapidly dropped from February 2021 as it was being outcompeted by the more transmissible Alpha. In April, Epsilon remained relatively frequent in parts of northern California, but it had virtually disappeared from the south of the state and had never been able to establish a foothold elsewhere; only 3.2% of all cases in the United States were Epsilon, whereas more than two-thirds were Alpha.[144]
Zeta (lineage P.2)
Zeta variant or lineage P.2, a sub-lineage of B.1.1.28 like P.1, was first detected in circulation in the state of Rio de Janeiro; it harbours the E484K mutation, but not the N501Y and K417T mutations.[114] It evolved independently in Rio de Janeiro without being directly related to the Gamma variant from Manaus.[110][145]
Under the simplified naming scheme proposed by the World Health Organization, P.2 has been labeled Zeta variant', and is considered a variant of interest (VOI), but not yet a variant of concern.[11]
Eta (lineage B.1.525)
The Eta variant or lineage B.1.525, also called VUI-21FEB-03[13] (previously VUI-202102/03) by Public Health England (PHE) and formerly known as UK1188,[13] 21D[18] or 20A/S:484K,[86] does not carry the same N501Y mutation found in Alpha, Beta and Gamma, but carries the same E484K-mutation as found in the Gamma, Zeta, and Beta variants, and also carries the same ΔH69/ΔV70 deletion (a deletion of the amino acids histidine and valine in positions 69 and 70) as found in Alpha, N439K variant (B.1.141 and B.1.258) and Y453F variant (Cluster 5).[146] Eta differs from all other variants by having both the E484K-mutation and a new F888L mutation (a substitution of phenylalanine (F) with leucine (L) in the S2 domain of the spike protein). As of March 5, it had been detected in 23 countries, including the UK, Denmark, Finland, Norway, Netherlands, Belgium, France, Spain, Nigeria, Ghana, Jordan, Japan, Singapore, Australia, Canada, Germany, Italy, Slovenia, Austria, Malaysia, Switzerland, the Republic of Ireland and the US.[147][148][149][51][150][151][152] It has also been reported in Mayotte, the overseas department/region of France.[147] The first cases were detected in December 2020 in the UK and Nigeria, and as of 15 February, it had occurred in the highest frequency among samples in the latter country.[51] As of 24 February, 56 cases were found in the UK.[13] Denmark, which sequences all its COVID-19 cases, found 113 cases of this variant from January 14 to February 21, of which seven were directly related to foreign travels to Nigeria.[148]
UK experts are studying it to understand how much of a risk it could be. It is currently regarded as a "variant under investigation", but pending further study, it may become a "variant of concern". Prof Ravi Gupta, from the University of Cambridge spoke to the BBC and said lineage B.1.525 appeared to have "significant mutations" already seen in some of the other newer variants, which is partly reassuring as their likely effect is to some extent more predictable.[153]
Under the simplified naming scheme proposed by the World Health Organization, lineage B.1.525 has been labelled variant Eta.[11]
Theta (lineage P.3)
On 18 February 2021, the Department of Health of the Philippines confirmed the detection of two mutations of COVID-19 in Central Visayas after samples from patients were sent to undergo genome sequencing. The mutations were later named as E484K and N501Y, which were detected in 37 out of 50 samples, with both mutations co-occurrent in 29 out of these. There were no official names for the variants and the full sequence was yet to be identified.[154] It is also labelled as Theta variant by WHO.
On 13 March, the Department of Health confirmed the mutations constitutes a variant which was designated as lineage P.3.[155] On the same day, it also confirmed the first COVID-19 case caused by the Gamma variant in the country. Although the Gamma and Theta variants stem from lineage B.1.1.28, the department said that the impact of the Theta variant on vaccine efficacy and transmissibility is yet to be ascertained. The Philippines had 98 cases of the Theta variant on 13 March.[156] On 12 March it was announced that Theta had also been detected in Japan.[157][158] On 17 March, the United Kingdom confirmed its first two cases,[159] where PHE termed it VUI-21MAR-02.[13] On 30 April 2021, Malaysia detected 8 cases of the Theta variant in Sarawak.[160]
Iota (lineage B.1.526)
In November 2020, a mutant variant was discovered in New York City, which was named lineage B.1.526.[161] As of April 11, 2021, the variant has been detected in at least 48 U.S. states and 18 countries. In a pattern mirroring Epsilon, Iota was initially able to reach relatively high levels in some states, but in the spring of 2021 it was outcompeted by the more transmissible Alpha.[144] It is labelled as Iota variant by the WHO.
Kappa (lineage B.1.617.1)
Kappa variant[162] is one of the three sublineages of lineage B.1.617. It is also known as lineage B.1.617.1, 21B[18] or 21A/S:154K,[86] and was first detected in India in December 2020.[163] By the end of March 2021, the Kappa variant accounted for more than half of the sequences being submitted from India.[164] On 1 April 2021, it was designated a variant under investigation (VUI-21APR-01) by Public Health England.[165]
Lambda (lineage C.37)
The Lambda variant, also known as lineage C.37, was first detected in Peru in August 2020 and was designated as a variant of interest on 14 June 2021.[166]
Other notable variants
Lineage B.1.1.207
First sequenced in August 2020 in Nigeria,[167] the implications for transmission and virulence are unclear but it has been listed as an emerging variant by the US Centers for Disease Control.[22] Sequenced by the African Centre of Excellence for Genomics of Infectious Diseases in Nigeria, this variant has a P681H mutation, shared in common with the Alpha variant. It shares no other mutations with the Alpha variant and as of late December 2020 this variant accounts for around 1% of viral genomes sequenced in Nigeria, though this may rise.[167] As of May 2021, lineage B.1.1.207 has been detected in 10 countries.[168]
Lineage B.1.620
In March 2021, this variant was discovered in Lithuania. It was named lineage B.1.620, also known as the 'Lithuanian strain'. It is found in Central Africa as well as North America.[169] Apart from Lithuania, other European countries including Spain and Belgium have also found presence of this variant. This lineage has 23 mutations and deletions compared to the reference strain, some of which are unique mutations. The lineage contains an E484K mutation.[169][170] D614G, a mutation present in most circulating strain, is also found in this variant.[171] Other notable mutations include P681H and S477N.[169]
Additional variants
- Lineage B.1.618 was first isolated in October 2020. It has the E484K mutation in common with several other variants, and showed significant spread in April 2021 in West Bengal, India.[172][173] As of 23 April 2021, the PANGOLIN database showed 135 sequences detected in India, with single-figure numbers in each of eight other countries worldwide.[174]
- Lineage B.1.1.318 was designated by PHE as a VUI (VUI-21FEB-04,[13] previously VUI-202102/04) on 24 February 2021. 16 cases of it have been detected in the UK.[13][175]
- Lineage B.1.1.317, while not considered a variant of concern, is noteworthy in that Queensland Health forced 2 people undertaking hotel quarantine in Brisbane, Australia to undergo an additional 5 days quarantine on top of the mandatory 14 days after it was confirmed they were infected with this variant.[176]
- On 29 May 2021, medical scientists in Vietnam reported a new, more contagious, form of the COVID-19 virus, that may be a mixture of the variants first detected in India and Britain.[177] On 3 June, the WHO described this as a mutated form of the Delta variant.[178]
Cross-species transmission
Cluster 5
In early November 2020, Cluster 5, also referred to as ΔFVI-spike by the Danish State Serum Institute (SSI),[179] was discovered in Northern Jutland, Denmark, and is believed to have been spread from minks to humans via mink farms. On 4 November 2020, it was announced that the mink population in Denmark would be culled to prevent the possible spread of this mutation and reduce the risk of new mutations happening. A lockdown and travel restrictions were introduced in seven municipalities of Northern Jutland to prevent the mutation from spreading, which could compromise national or international responses to the COVID-19 pandemic. By 5 November 2020, some 214 mink-related human cases had been detected.[180]
The World Health Organization (WHO) has stated that cluster 5 has a "moderately decreased sensitivity to neutralizing antibodies".[181] SSI warned that the mutation could reduce the effect of COVID-19 vaccines under development, although it was unlikely to render them useless. Following the lockdown and mass-testing, SSI announced on 19 November 2020 that cluster 5 in all probability had become extinct.[182] As of 1 February 2021, authors to a peer-reviewed paper, all of whom were from the SSI, assessed that cluster 5 was not in circulation in the human population.[183]
There is a risk that COVID-19 could transfer from humans to other animal populations and could combine with other animal viruses to creat yet more variants that are dangerous to humans.[184]
Notable missense mutations
N440K
The name of the mutation, N440K, refers to an exchange whereby the asparagine (N) is replaced by lysine (K) at position 440.[185]
This mutation has been observed in cell cultures to be 10 times more infective compared to the previously widespread A2a strain and 1000 times more in the lesser widespread A3i strain.[186] It is involved in current rapid surges of Covid cases in India.[187] India has the largest proportion of N440K mutated variants followed by the US and Germany.[188]
L452R
The name of the mutation, L452R, refers to an exchange whereby the leucine (L) is replaced by arginine (R) at position 452.[185]
There has been a significant surge of COVID-19 starting 2021 all across India caused in part by lineage B.1.617, frequently, but misleadingly, referred to as a "double mutant". L452R is a relevant mutation in this strain that enhances ACE2 receptor binding ability and can reduce vaccine-stimulated antibodies from attaching to this altered spike protein.
L452R, some studies show, could even make the coronavirus resistant to T cells, that are class of cells necessary to target and destroy virus-infected cells. They are different from antibodies that are useful in blocking coronavirus particles and preventing it from proliferating.[124]
S477G/N
A highly flexible region in the receptor binding domain (RBD) of SARS-CoV-2, starting from residue 475 and continuing up to residue 485, was identified using bioinformatics and statistical methods in several studies. The University of Graz[189] and the Biotech Company Innophore[190] have shown in a recent publication that structurally, the position S477 shows the highest flexibility among them.[191]
At the same time, S477 is hitherto the most frequently exchanged amino acid residue in the RBDs of SARS-CoV-2 mutants. By using molecular dynamics simulations of RBD during the binding process to hACE2, it has been shown that both S477G and S477N strengthen the binding of the SARS-COV-2 spike with the hACE2 receptor. The vaccine developer BioNTech[192] referenced this amino acid exchange as relevant regarding future vaccine design in a preprint published in February 2021.[193]
E484K
The name of the mutation, E484K, refers to an exchange whereby the glutamic acid (E) is replaced by lysine (K) at position 484.[185] It is nicknamed "Eeek".[194]
E484K has been reported to be an escape mutation (i.e., a mutation that improves a virus's ability to evade the host's immune system[195][196]) from at least one form of monoclonal antibody against SARS-CoV-2, indicating there may be a "possible change in antigenicity".[197] The Alpha variant (lineage P.1),[110] the Zeta variant (lineage P.2, also known as lineage B.1.1.28.2)[114] and the Beta variant (501.V2) exhibit this mutation.[197] A limited number of lineage B.1.1.7 genomes with E484K mutation have also been detected.[198] Monoclonal and serum-derived antibodies are reported to be from 10 to 60 times less effective in neutralizing virus bearing the E484K mutation.[199][200] On 2 February 2021, medical scientists in the United Kingdom reported the detection of E484K in 11 samples (out of 214,000 samples), a mutation that may compromise current vaccine effectiveness.[201][202]
E484Q
The name of the mutation, E484Q, refers to an exchange whereby the glutamic acid (E) is replaced by glutamine (Q) at position 484.[185]
India is seeing a significant surge of COVID-19 starting 2021 caused in part by lineage B.1.617. This has frequently (but misleadingly, as most variants contain multiple mutations) been referred to as a "double mutant".[203] E484Q may enhance ACE2 receptor binding ability and may reduce vaccine-stimulated antibodies from attaching to this altered spike protein.[124]
N501Y
N501Y denotes a change from asparagine (N) to tyrosine (Y) in amino-acid position 501.[204] N501Y has been nicknamed "Nelly".[194]
This change is believed by PHE to increase binding affinity because of its position inside the spike glycoprotein's receptor-binding domain, which binds ACE2 in human cells; data also support the hypothesis of increased binding affinity from this change.[23] Molecular interaction modeling and the free energy of binding calculations has demonstrated that the mutation N501Y has the highest binding affinity in variants of concern RBD to hACE2.[1] Variants with N501Y include Gamma,[197][110] Alpha (VOC 20DEC-01), Beta, and COH.20G/501Y (identified in Columbus, Ohio).[1] This last became the dominant form of the virus in Columbus in late December 2020 and January and appears to have evolved independently of other variants.[205][206]
D614G

D614G is a missense mutation that affects the spike protein of SARS-CoV-2. The frequency of this mutation in the viral population has increased during the pandemic. G (glycine) has replaced D (aspartic acid) at position 614 in many countries, especially in Europe though more slowly in China and the rest of East Asia, supporting the hypothesis that G increases the transmission rate, which is consistent with higher viral titers and infectivity in vitro.[58] Researchers with the PANGOLIN tool nicknamed this mutation "Doug".[194]
In July 2020, it was reported that the more infectious D614G SARS-CoV-2 variant had become the dominant form in the pandemic.[208][209][210][211] PHE confirmed that the D614G mutation had a "moderate effect on transmissibility" and was being tracked internationally.[204]
The global prevalence of D614G correlates with the prevalence of loss of smell (anosmia) as a symptom of COVID-19, possibly mediated by higher binding of the RBD to the ACE2 receptor or higher protein stability and hence higher infectivity of the olfactory epithelium.[212]
Variants containing the D614G mutation are found in the G clade by GISAID[58] and the B.1 clade by the PANGOLIN tool.[58]
P681H

In January 2021, scientists reported in a preprint that the mutation 'P681H', a characteristic feature of the Alpha variant and lineage B.1.1.207 (identified in Nigeria), is showing a significant exponential increase in worldwide frequency, similar to the now globally prevalent 'D614G'.[213][207]
P681R
The name of the mutation, P681R, refers to an exchange whereby the proline (P) is replaced by arginine (R) at position 681.[185]
Indian SARS-CoV-2 Genomics Consortium (INSACOG) found that other than the two mutations E484Q and L452R, there is also a third significant mutation, P681R in lineage B.1.617. All three concerning mutations are on the spike protein, the operative part of the coronavirus that binds to receptor cells of the body.[124]
A701V
According to initial media reports, the Malaysian Ministry of Health announced on 23 December 2020 that it had discovered a mutation in the SARS-CoV-2 genome which they designated as A701B(sic), among 60 samples collected from the Benteng Lahad Datu cluster in Sabah. The mutation was characterized as being similar to the one found recently at that time in South Africa, Australia, and the Netherlands, although it was uncertain if this mutation was more infectious or aggressive than before.[214] The provincial government of Sulu in neighboring Philippines temporarily suspended travel to Sabah in response to the discovery of 'A701B' due to uncertainty over the nature of the mutation.[215]
On 25 December 2020, the government health organisation 'Kementerian Kesihatan Malaysia/ covid-19 Malaysia' described a mutation A701V as circulating and present in 85% of cases (D614G was present in 100% of cases) in Malaysia.[216][217][218] These reports also referred to samples collected from the Benteng Lahad Datu cluster.[218][217] The text of the announcement was mirrored verbatim on the Facebook page of Noor Hisham Abdullah, Malay Director-General of Health, who was quoted in some of the news articles.[217]
The A701V mutation has the amino acid alanine substituted by valine at position 701 in the spike protein. Globally, South Africa, Australia, Netherlands and England also reported A701V at about the same time as Malaysia.[216] In GISAID, the prevalence of this mutation is found to be about 0.18%. of cases.[216]
On 14 April 2021, 'Kementerian Kesihatan Malaysia' reported that the third wave, which had started in Sabah, has involved the introduction of variants with D614G and A701V mutations.[219]
New variant detection and assessment
On 26 January 2021, the British government said it would share its genomic sequencing capabilities with other countries in order to increase the genomic sequencing rate and trace new variants, and announced a "New Variant Assessment Platform".[220] As of January 2021, more than half of all genomic sequencing of COVID-19 was carried out in the UK.[221]
Origin of variants
Researchers have suggested that multiple mutations can arise in the course of the persistent infection of an immunocompromised patient, particularly when the virus develops escape mutations under the selection pressure of antibody or convalescent plasma treatment,[222][223] with the same deletions in surface antigens repeatedly recurring in different patients.[224]
Differential vaccine effectiveness
See also
- RaTG13, the closest known relative to SARS-CoV-2
- Pandemic prevention § Surveillance and mapping
Notes
- 1 2 In another source, GISAID name a set of 7 clades without the O clade but including a GV clade.[63]
- ↑ According to the WHO, "Lineages or clades can be defined based on viruses that share a phylogenetically determined common ancestor".[64]
- ↑ As of January 2021, at least one of the following criteria must be met in order to count as a clade in the Nextstrain system (quote from source):[lower-alpha 4]
- A clade reaches >20% global frequency for 2 or more months
- A clade reaches >30% regional frequency for 2 or more months
- A VOC (‘variant of concern’) is recognized (applies currently [6 January 2021] to 501Y.V1 and 501Y.V2)
References
- 1 2 3 4 5 Shahhosseini, Nariman; Babuadze, George; Wong, Gary; Kobinger, Gary (2021). "Mutation Signatures and In Silico Docking of Novel SARS-CoV-2 Variants of Concern". Microorganisms. 9 (5): 926. doi:10.3390/microorganisms9050926. PMID 33925854. S2CID 233460887. Archived from the original on 4 May 2021. Retrieved 4 May 2021.
- ↑ "Coronavirus variants and mutations: The science explained". BBC News. 6 January 2021. Archived from the original on 22 February 2021. Retrieved 2 February 2021.
- ↑ Kupferschmidt K (15 January 2021). "New coronavirus variants could cause more reinfections, require updated vaccines". Science. American Association for the Advancement of Science. doi:10.1126/science.abg6028. Archived from the original on 22 February 2021. Retrieved 2 February 2021.
- ↑ Shahhosseini, Nariman; Wong, Gary; Kobinger, Gary; Chinikar, Sadegh (2021). "SARS-CoV-2 spillover transmission due to recombination event". Gene Reports. 23: 101045. doi:10.1016/j.genrep.2021.101045. PMC 7884226. PMID 33615041.
- 1 2 3 Kumar, Sudhir; Tao, Qiqing; Weaver, Steven; Sanderford, Maxwell; Caraballo-Ortiz, Marcos A; Sharma, Sudip; Pond, Sergei L K; Miura, Sayaka. "An evolutionary portrait of the progenitor SARS-CoV-2 and its dominant offshoots in COVID-19 pandemic". Oxford Academic. Archived from the original on 23 June 2021. Retrieved 10 May 2020.
- ↑ "The ancestor of SARS-CoV-2's Wuhan strain was circulating in late October 2019". News Medical. Archived from the original on 24 July 2021. Retrieved 10 May 2020.
Journal reference: Kumar, S. et al. (2021). An evolutionary portrait...
- 1 2 "Lineage descriptions". cov-lineages.org. Pango team. Archived from the original on 4 June 2021. Retrieved 18 June 2021.
- ↑ Yurkovetskiy, Leonid; Wang, Xue; Pascal, Kristen E.; Tomkins-Tinch, Christopher; Nyalile, Thomas P.; Wang, Yetao; et al. (October 2020). "Structural and Functional Analysis of the D614G SARS-CoV-2 Spike Protein Variant". Cell. 183 (3): 739–751.e8. doi:10.1016/j.cell.2020.09.032. PMC 7492024.
- ↑ Thomson, Emma C.; Rosen, Laura E.; Shepherd, James G.; Spreafico, Roberto; da Silva Filipe, Ana; Wojcechowskyj, Jason A.; et al. (March 2021). "Circulating SARS-CoV-2 spike N439K variants maintain fitness while evading antibody-mediated immunity". Cell. 184 (5): 1171–1187.e20. doi:10.1016/j.cell.2021.01.037.
- ↑ Covid: Is there a limit to how much worse variants can get? Archived 15 June 2021 at the Wayback Machine BBC
- 1 2 3 4 5 "Tracking SARS-CoV-2 variants". who.int. World Health Organization. Archived from the original on 9 June 2021. Retrieved 1 June 2021.
- 1 2 3 4 5 6 7 "SARS-CoV-2 Variant Classifications and Definitions". CDC.gov. Centers for Disease Control and Prevention. Archived from the original on 16 June 2021. Retrieved 18 June 2021.
- 1 2 3 4 5 6 7 8 9 10 11 12 13 14 15 16 "Variants: distribution of cases data". GOV.UK. Government Digital Service. Public Health England. Archived from the original on 7 June 2021. Retrieved 18 June 2021.
- 1 2 "Living Evidence – SARS-CoV-2 variants". Agency for Clinical Innovation. nsw.gov.au. Ministry of Health (New South Wales). Archived from the original on 16 April 2021. Retrieved 22 March 2021.
- ↑ "SARS-CoV-2 variants of concern". ECDC.eu. European Centre for Disease Prevention and Control. Archived from the original on 16 June 2021. Retrieved 7 June 2021.
- ↑ "Coronavirus Disease (COVID-19) Situation Reports". who.int. World Health Organization. Archived from the original on 26 January 2020. Retrieved 18 June 2021.
- ↑ "Investigation of SARS-CoV-2 variants of concern: technical briefings". GOV.UK. Government Digital Service. Public Health England. Archived from the original on 18 June 2021. Retrieved 18 June 2021.
- 1 2 3 4 5 6 7 8 9 Weekly epidemiological update on COVID-19 - 15 June 2021 (Situation report). World Health Organization. 15 June 2021. Retrieved 16 June 2021.
- ↑ "Lineage B.1.1.7". cov-lineages.org. Pango team. Archived from the original on 16 June 2021. Retrieved 6 June 2021.
- ↑ Latif AA, Mullen JL, Alkuzweny M, Tsueng G, Cano M, Haag E, et al. "B.1.1.7 Lineage Report". outbreak.info. Archived from the original on 6 June 2021. Retrieved 6 June 2021.
- ↑ Investigation of novel SARS-COV-2 variant, technical briefing 1 (PDF) (Briefing). Public Health England. 21 December 2020. Retrieved 6 June 2021.
- 1 2 3 4 5 6 7 8 9 "Emerging SARS-CoV-2 Variants". CDC.gov (Science brief). Centers for Disease Control and Prevention. 28 January 2021. Archived from the original on 15 May 2021. Retrieved 4 January 2021.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - 1 2 3 Chand et al. (2020), p. 6, Potential impact of spike variant N501Y.
- ↑ Davies NG, Abbott S, Barnard RC, Jarvis CI, Kucharski AJ, Munday JD; et al. (2021). "Estimated transmissibility and impact of SARS-CoV-2 lineage B.1.1.7 in England". Science. 372 (6538). doi:10.1126/science.abg3055. PMC 8128288. PMID 33658326. Archived from the original on 27 August 2021. Retrieved 14 March 2022.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - ↑ Davies G, Jarvis C, Edmunds WJ, Jewell N, Diaz-Ordaz K, Keogh R (15 March 2021). "Increased mortality in community-tested cases of SARS-CoV-2 lineage B.1.1.7". Nature (Published). 593 (7858): 270–274. doi:10.1038/s41586-021-03426-1. PMID 33723411. Archived from the original on 18 June 2021. Retrieved 29 April 2021.
- ↑ DChallen R, Brooks-Pollock E, Read J, Dyson L, Tsaneva-Atanasova K, Danon L (10 March 2021). "Risk of mortality in patients infected with SARS-CoV-2 variant of concern 202012/1: matched cohort study". The BMJ (Published). 372: n579. doi:10.1136/bmj.n579. PMC 7941603. PMID 33687922.
- 1 2 3 4 Risk related to the spread of new SARS-CoV-2 variants of concern in the EU/EEA – first update (Risk assessment). European Centre for Disease Prevention and Control. 2 February 2021.
- ↑ Horby, Peter; Barclay, Wendy; Huntley, Catherine (13 January 2021). NERVTAG paper: brief note on SARS-CoV-2 variants (Note). Public Health England. Retrieved 6 June 2021.
- ↑ Sruthi S (10 February 2021). "Notable Variants And Mutation Of SARS-CoV-2". BioTecNika. Archived from the original on 17 April 2021. Retrieved 22 March 2021.
- ↑ Planas D, Bruel T, Grzelak L, et al. (14 April 2021). "Sensitivity of infectious SARS-CoV-2 B.1.1.7 and B.1.351 variants to neutralizing antibodies". Nature Medicine. 27 (5): 917–924. doi:10.1038/s41591-021-01318-5. PMID 33772244.
- ↑ "Coronavirus: Sinovac vaccine gives 70 per cent less protection against South African variant, but Hongkongers urged to still get jab". South China Morning Post. 20 April 2021. Archived from the original on 6 June 2021. Retrieved 20 April 2021.
- ↑ "Confirmed cases of COVID-19 variants identified in UK". Friday 15 January: GOV.UK. Public Health England. 15 January 2021. Archived from the original on 7 May 2021. Retrieved 18 June 2021.
{{cite news}}: CS1 maint: location (link) - ↑ Horby, Peter; Barclay, Wendy; Gupta, Ravi; Huntley, Catherine (27 January 2021). NERVTAG paper: note on variant P.1 (Note). Public Health England. Retrieved 6 June 2021.
- ↑ Coutinho RM, Marquitti FM, Ferreira LS, Borges ME, da Silva RL, Canton O, et al. (23 March 2021). "Model-based estimation of transmissibility and reinfection of SARS-CoV-2 P.1 variant". medRxiv (Preprint): 9. doi:10.1101/2021.03.03.21252706. S2CID 232119656. Archived from the original on 3 May 2021. Retrieved 29 April 2021.
The new variant was found to be about 2.6 times more transmissible (95% Confidence Interval (CI): 2.4–2.8) than previous circulating variant(s). ... Table 1: Summary of the fitted parameters and respective confidence intervals considering the entire period, November 1, 2020-January 31, 2021 maintaining the same pathogenicity of the previous variant. Parameter: Relative transmission rate for the new variant. Estimate: 2.61. 2.5%: 2.45. 97.5%: 2.76.
- 1 2 3 Faria NR, Mellan TA, Whittaker C, Claro IM, Candido DS, Mishra S, et al. (21 May 2021). "Genomics and epidemiology of the P.1 SARS-CoV-2 lineage in Manaus, Brazil". Science. 372 (6544): 815–821. doi:10.1126/science.abh2644. ISSN 0036-8075. PMC 8139423. PMID 33853970.
Within this plausible region of parameter space, P.1 can be between 1.7 and 2.4 times more transmissible (50% BCI, 2.0 median, with a 99% posterior probability of being >1) than local non-P1 lineages and can evade 21 to 46% (50% BCI, 32% median, with a 95% posterior probability of being able to evade at least 10%) of protective immunity elicited by previous infection with non-P.1 lineages, corresponding to 54 to 79% (50% BCI, 68% median) cross-immunity ... We estimate that infections are 1.2 to 1.9 times more likely (50% BCI, median 1.5, 90% posterior probability of being >1) to result in mortality in the period after the emergence of P.1, compared with before, although posterior estimates of this relative risk are also correlated with inferred cross-immunity. More broadly, the recent epidemic in Manaus has strained the city’s health care system, leading to inadequate access to medical care. We therefore cannot determine whether the estimated increase in relative mortality risk is due to P.1 infection, stresses on the Manaus health care system, or both. Detailed clinical investigations of P.1 infections are needed.
- ↑ Freitas AR, Lemos DR, Beckedorff OA, Cavalcanti LP, Siqueira AM, Mello RC, et al. (19 April 2021). "The increase in the risk of severity and fatality rate of covid-19 in southern Brazil after the emergence of the Variant of Concern (VOC) SARS-CoV-2 P.1 was greater among young adults without pre-existing risk conditions" (Preprint). doi:10.1101/2021.04.13.21255281. Archived from the original on 4 June 2021. Retrieved 18 June 2021 – via medRxiv.
Female 20 to 39 years old, with no pre-existing risk conditions, were at risk of death 5.65 times higher in February (95% CI, 2.9-11.03; p <0.0001) and in the age group of 40 and 59 years old, this risk was 7.7 times higher (95% CI, 5.01-11.83; p <0.0001) comparing with November–December. ... The heterogeneity observed between the age groups was greater when we analyzed the subgroup of the population without preexisting risk conditions where we found that the CFR in the female sex in the second wave was 1.95 times (95% CI, 1.38-2.76) the CFR of the first wave in the population over 85 years old and was 7.7 times (95% CI, 5.01-11.83; p < 0.0001) in the population between 40 and 59 years old. In the male population without previous diseases, the CFR in the second wave was 2.18 (95% CI, 1.62-2.93) times the CFR of the first wave in the population over 85 years old and 5.9 (95% CI, 3.2-10.85; p < 0, 0001) higher in the range between 20 and 39 years old.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Public Health England (16 February 2021). "Variants: distribution of cases data". GOV.UK. Archived from the original on 7 June 2021. Retrieved 17 February 2021.
- ↑ Investigation of novel SARS-CoV-2 variant 202012/01, technical briefing 5 (PDF) (Briefing). Public Health England. 2 February 2021. GW-1905. Retrieved 14 June 2021.
- ↑ Investigation of SARS-CoV-2 variants of concern in England, technical briefing 6 (PDF) (Briefing). Public Health England. 13 February 2021. GW-1934. Retrieved 6 June 2021.
- 1 2 3 Collier DA, De Marco A, Gupta RK, et al. (6 May 2021). "Sensitivity of SARS-CoV-2 B.1.1.7 to mRNA vaccine-elicited antibodies". Nature (Published). 593: 136–141. doi:10.1038/s41586-021-03412-7. Archived from the original on 10 May 2021. Retrieved 1 June 2021.
We therefore generated pseudoviruses that carried the B.1.1.7 spike mutations with or without the additional E484K substitution and tested these against sera obtained after the first and second dose of the BNT162b2 mRNA vaccine as well as against convalescent sera. After the second vaccine dose, we observed a considerable loss of neutralizing activity for the pseudovirus with the B.1.1.7 spike mutations and E484K (Fig. 3d, e). The mean fold change for the E484K-containing B.1.1.7 spike variant was 6.7 compared with 1.9 for the B.1.1.7 variant, relative to the wild-type spike protein (Fig. 3a–c and Extended Data Fig. 5). Similarly, when we tested a panel of convalescent sera with a range of neutralization titres (Fig. 1f, g and Extended Data Fig. 5), we observed additional loss of activity against the mutant B.1.1.7 spike with E484K, with fold change of 11.4 relative to the wild-type spike protein (Fig. 3f, g and Extended Data Fig. 5).
- ↑ Azad, Arman (17 March 2021). "Coronavirus strains first detected in California are officially 'variants of concern,' CDC says". CNN. Archived from the original on 6 June 2021. Retrieved 6 June 2021.
- ↑ Deng X, Garcia-Knight MA, Khalid MM, Servellita V, Wang C, Morris MK, et al. (March 2021). "Transmission, infectivity, and antibody neutralization of an emerging SARS-CoV-2 variant in California carrying a L452R spike protein mutation". MedRxiv (Preprint). doi:10.1101/2021.03.07.21252647. PMC 7987058. PMID 33758899.
- ↑ Wadman M (23 February 2021). "California coronavirus strain may be more infectious – and lethal". Science News. doi:10.1126/science.abh2101. Archived from the original on 1 May 2021. Retrieved 17 March 2021.
- ↑ SARS-CoV-2 variants of concern and variants under investigation in England, technical briefing 10 (PDF) (Briefing). Public Health England. 7 May 2021. GOV-8226. Retrieved 6 June 2021.
- 1 2 3 "SARS-CoV-2 Variant Classifications and Definitions". CDC.gov. Centers for Disease Control and Prevention. 12 May 2021. Archived from the original on 16 June 2021. Retrieved 16 May 2021.
- ↑ SARS-CoV-2 variants of concern and variants under investigation in England, technical briefing 15 (PDF) (Briefing). Public Health England. 11 June 2021. Retrieved 15 June 2021.
- 1 2 Yadav PD, Sapkal GN, Abraham P, Ella R, Deshpande G, Patil DY, et al. (7 May 2021). "Neutralization of variant under investigation B.1.617 with sera of BBV152 vaccinees". Clinical Infectious Diseases. Oxford University Press. bioRxiv 10.1101/2021.04.23.441101. doi:10.1093/cid/ciab411. PMID 33961693. Archived from the original on 3 July 2021. Retrieved 18 June 2021.
- ↑ Nuki, Paul; Newey, Sarah (16 April 2021). "Arrival of India's 'double mutation' adds to variant woes, but threat posed remains unclear". The Telegraph. ISSN 0307-1235. Archived from the original on 21 June 2021. Retrieved 17 April 2021.
- ↑ "B.1.525 international lineage report". cov-lineages.org. Pango team. Archived from the original on 22 June 2021. Retrieved 4 June 2021.
- ↑ "Date mismatch between international report and lineage description - cov-lineages/pangolin". GitHub (Software issue). 13 June 2021. Archived from the original on 27 August 2021. Retrieved 14 June 2021.
- 1 2 "B.1.525". cov-lineages.org. Pango team. Archived from the original on 22 June 2021. Retrieved 22 March 2021.
- ↑ "B.1.525". cov-lineages.org. Pango team. Archived from the original on 22 June 2021. Retrieved 22 March 2021.
- ↑ This table is an adaptation and expansion of Alm et al., figure 1.
- 1 2 Rambaut A, Holmes EC, O'Toole Á, Hill V, McCrone JT, Ruis C, et al. (November 2020). "A dynamic nomenclature proposal for SARS-CoV-2 lineages to assist genomic epidemiology". Nature Microbiology. 5 (11): 1403–1407. doi:10.1038/s41564-020-0770-5. PMC 7610519. PMID 32669681. S2CID 220544096. Cited in Alm et al.
- 1 2 Alm E, Broberg EK, Connor T, Hodcroft EB, Komissarov AB, Maurer-Stroh S, et al. (The WHO European Region sequencing laboratories and GISAID EpiCoV group) (August 2020). "Geographical and temporal distribution of SARS-CoV-2 clades in the WHO European Region, January to June 2020". Euro Surveillance. 25 (32). doi:10.2807/1560-7917.ES.2020.25.32.2001410. PMC 7427299. PMID 32794443.
- ↑ "Nextclade" (What are the clades?). nextstrain.org. Archived from the original on 19 January 2021. Retrieved 19 January 2021.
- 1 2 3 Bedford T, Hodcroft B, Neher RA (6 January 2021). "Updated Nextstrain SARS-CoV-2 clade naming strategy". nextstrain.org. Archived from the original on 18 January 2021. Retrieved 19 January 2021.
- 1 2 3 4 5 6 Zhukova A, Blassel L, Lemoine F, Morel M, Voznica J, Gascuel O (November 2020). "Origin, evolution and global spread of SARS-CoV-2". Comptes Rendus Biologies: 1–20. doi:10.5802/crbiol.29. PMID 33274614.
- ↑ "Genomic epidemiology of novel coronavirus – Global subsampling (Filtered to B.1.617)". nextstrain.org. Archived from the original on 13 July 2021. Retrieved 5 May 2021.
- 1 2 3 4 Zhang W, Davis B, Chen SS, Martinez JS, Plummer JT, Vail E (2021). "Emergence of a novel SARS-CoV-2 strain in Southern California, USA". MedRxiv. doi:10.1101/2021.01.18.21249786. S2CID 231646931. Archived from the original on 12 July 2021. Retrieved 18 June 2021.
- ↑ "PANGO lineages-Lineage B.1.1.28". cov-lineages.org. Archived from the original on 24 February 2021. Retrieved 4 February 2021.
- ↑ "Variant: 20J/501Y.V3". covariants.org. 1 April 2021. Archived from the original on 23 March 2021. Retrieved 6 April 2021.
- ↑ "clade tree (from 'Clade and lineage nomenclature')". GISAID. 4 July 2020. Archived from the original on 9 January 2021. Retrieved 7 January 2021.
- 1 2 3 4 WHO Headquarters (8 January 2021). "3.6 Considerations for virus naming and nomenclature". SARS-CoV-2 genomic sequencing for public health goals: Interim guidance, 8 January 2021. World Health Organization. p. 6. Archived from the original on 23 January 2021. Retrieved 2 February 2021.
- ↑ "Don't call it the 'British variant.' Use the correct name: B.1.1.7". STAT. 9 February 2021. Archived from the original on 4 June 2021. Retrieved 12 February 2021.
- ↑ Flanagan R (2 February 2021). "Why the WHO won't call it the 'U.K. variant', and you shouldn't either". CTV News. Archived from the original on 1 May 2021. Retrieved 12 February 2021.
- ↑ For a list of sources using names referring to the country in which the variants were first identified, see, for example, Talk:South African COVID variant and Talk:U.K. Coronavirus variant.
- ↑ "The name game for coronavirus variants just got a little easier". Archived from the original on 17 June 2021. Retrieved 18 June 2021.
- ↑ World Health Organization (15 January 2021). "Statement on the sixth meeting of the International Health Regulations (2005) Emergency Committee regarding the coronavirus disease (COVID-19) pandemic". Archived from the original on 7 February 2021. Retrieved 18 January 2021.
- ↑ Koyama T, Platt D, Parida L (July 2020). "Variant analysis of SARS-CoV-2 genomes". Bulletin of the World Health Organization. 98 (7): 495–504. doi:10.2471/BLT.20.253591. PMC 7375210. PMID 32742035.
We detected in total 65776 variants with 5775 distinct variants.
- ↑ "Global phylogeny, updated by Nextstrain". GISAID. 18 January 2021. Archived from the original on 20 January 2021. Retrieved 19 January 2021.
- ↑ Hadfield J, Megill C, Bell SM, Huddleston J, Potter B, Callender C, et al. (December 2018). Kelso J (ed.). "Nextstrain: real-time tracking of pathogen evolution". Bioinformatics. 34 (23): 4121–4123. doi:10.1093/bioinformatics/bty407. PMC 6247931. PMID 29790939.
- ↑ "Nextstrain COVID-19". Nextstrain. Archived from the original on 20 April 2020. Retrieved 1 June 2021.
- ↑ "cov-lineages/pangolin: Software package for assigning SARS-CoV-2 genome sequences to global lineages". Github. Archived from the original on 15 February 2021. Retrieved 2 January 2021.
- ↑ Rambaut A, Holmes EC, O'Toole Á, Hill V, McCrone JT, Ruis C, et al. (March 2021). "Addendum: A dynamic nomenclature proposal for SARS-CoV-2 lineages to assist genomic epidemiology". Nature Microbiology. 6 (3): 415. doi:10.1038/s41564-021-00872-5. PMC 7845574. PMID 33514928.
- ↑ "A new coronavirus associated with human respiratory disease in China" Archived 19 June 2021 at the Wayback Machine Fan Wu, Su Zhao, Bin Yu, Yan-Mei Chen, Wen Wang, Zhi-Gang Song, Yi Hu, Zhao-Wu Tao, Jun-Hua Tian, Yuan-Yuan Pei, Ming-Li Yuan, Yu-Ling Zhang, Fa-Hui Dai, Yi Liu, Qi-Min Wang, Jiao-Jiao Zheng, Lin Xu, Edward C Holmes, Yong-Zhen Zhang. PMID 32015508. PMC PMC7094943 doi:10.1038/s41586-020-2008-3.
- ↑ Comparative genomics reveals early emergence and biased spatio-temporal distribution of SARS-CoV-2 Archived 27 August 2021 at the Wayback Machine Matteo Chiara, David S Horner, Carmela Gissi, Graziano Pesole PMID 33605421 PMCID: PMC7928790 DOI: 10.1093/molbev/msab049
- ↑ Zhengli, Shi; Team of 29 researchers at the WIV (3 February 2020). "A pneumonia outbreak associated with a new coronavirus of probable bat origin". Nature. 579 (7798): 270–273. Bibcode:2020Natur.579..270Z. doi:10.1038/s41586-020-2012-7. PMC 7095418. PMID 32015507.
- ↑ Okada, Pilailuk; Buathong, Rome; Phuygun, Siripaporn; Thanadachakul, Thanutsapa; Parnmen, Sittiporn; Wongboot, Warawan; Waicharoen, Sunthareeya; Wacharapluesadee, Supaporn; Uttayamakul, Sumonmal; Vachiraphan, Apichart; Chittaganpitch, Malinee; Mekha, Nanthawan; Janejai, Noppavan; Iamsirithaworn, Sopon; Lee, Raphael TC; Maurer-Stroh, Sebastian (2020). "Early transmission patterns of coronavirus disease 2019 (COVID-19) in travellers from Wuhan to Thailand, January 2020". Eurosurveillance. 25 (8). doi:10.2807/1560-7917.ES.2020.25.8.2000097. PMC 7055038. PMID 32127124. Archived from the original on 26 May 2021. Retrieved 18 June 2021.
- ↑ Official hCoV-19 Reference Sequence Archived 6 May 2021 at the Wayback Machine. www.gisaid.org. Retrieved 14 May 2021.
- ↑ IDSA Contributor (2 February 2021). "COVID "Mega-variant" and eight criteria for a template to assess all variants". Science Speaks: Global ID News. Archived from the original on 21 April 2021. Retrieved 20 February 2021.
- ↑ Griffiths E, Tanner J, Knox N, Hsiao W, Van Domselaar G (15 January 2021). "CanCOGeN Interim Recommendations for Naming, Identifying, and Reporting SARS-CoV-2 Variants of Concern" (PDF). CanCOGeN (nccid.ca). Archived (PDF) from the original on 17 April 2021. Retrieved 25 February 2021.
- ↑ "Covid: Ireland, Italy, Belgium and Netherlands ban flights from UK". BBC News. 20 December 2020. Archived from the original on 21 December 2020. Retrieved 18 June 2021.
- ↑ Chand M, Hopkins S, Dabrera G, Achison C, Barclay W, Ferguson N, et al. (21 December 2020). Investigation of novel SARS-COV-2 variant: Variant of Concern 202012/01 (PDF) (Report). Public Health England. Archived (PDF) from the original on 22 February 2021. Retrieved 23 December 2020.
- ↑ "PHE investigating a novel strain of COVID-19". Public Health England (PHE). 14 December 2020. Archived from the original on 15 December 2021. Retrieved 18 June 2021.
- 1 2 3 4 5 6 7 Weekly epidemiological update on COVID-19 - 8 June 2021 (Situation report). World Health Organization. 8 June 2021. Retrieved 14 June 2021.
- ↑ Rambaut A, Loman N, Pybus O, Barclay W, Barrett J, Carabelli A, et al. (2020). Preliminary genomic characterisation of an emergent SARS-CoV-2 lineage in the UK defined by a novel set of spike mutations (Report). Written on behalf of COVID-19 Genomics Consortium UK. Archived from the original on 22 February 2021. Retrieved 20 December 2020.
- ↑ Kupferschmidt K (20 December 2020). "Mutant coronavirus in the United Kingdom sets off alarms but its importance remains unclear". Science Mag. Archived from the original on 21 December 2020. Retrieved 21 December 2020.
- ↑ "New evidence on VUI-202012/01 and review of the public health risk assessment". khub.net. 15 December 2020. Archived from the original on 24 July 2021. Retrieved 18 June 2021.
- ↑ "COG-UK Showcase Event". Archived from the original on 14 June 2021. Retrieved 25 December 2020 – via YouTube.
- ↑ "New evidence on VUI-202012/01 and review of the public health risk assessment". Archived from the original on 24 July 2021. Retrieved 4 January 2021.
- ↑ "Estimated transmissibility and severity of novel SARS-CoV-2 Variant of Concern 202012/01 in England". CMMID Repository. 23 December 2020. Archived from the original on 24 January 2021. Retrieved 24 January 2021 – via GitHub.
Cited in European Centre for Disease Prevention and Control (21 January 2021). "Risk related to the spread of new SARS-CoV-2 variants of concern in the EU/EEA – first update" (PDF). Stockholm: ECDC. p. 9. Archived (PDF) from the original on 22 February 2021. Retrieved 24 January 2021. - ↑ Gallagher J (22 January 2021). "Coronavirus: UK variant 'may be more deadly'". BBC News. Archived from the original on 23 May 2021. Retrieved 22 January 2021.
- ↑ Peter Horby; Catherine Huntley; Nick Davies; John Edmunds; Neil Ferguson; Graham Medley; Andrew Hayward; Muge Cevik; Calum Semple (11 February 2021). "NERVTAG paper on COVID-19 variant of concern B.1.1.7: NERVTAG update note on B.1.1.7 severity (2021-02-11)" (PDF). GOV.UK. Archived (PDF) from the original on 13 April 2021. Retrieved 18 June 2021.
- ↑ Genomic characteristics and clinical effect of the emergent SARS-CoV-2 B.1.1.7 lineage in London, UK: a whole-genome sequencing and hospital-based cohort study Archived 19 June 2021 at the Wayback Machine, Dan Frampton, et al., The Lancet, Online, April 12, 2021
- ↑ PANGO lineages Lineage B.1.1.7 Archived 16 June 2021 at the Wayback Machine cov-lineages.org, accessed 15 May 2021
- ↑ Mandavilli A (5 March 2021). "In Oregon, Scientists Find a Virus Variant With a Worrying Mutation – In a single sample, geneticists discovered a version of the coronavirus first identified in Britain with a mutation originally reported in South Africa". The New York Times. Archived from the original on 6 March 2021. Retrieved 6 March 2021.
- ↑ Chen RE, Zhang X, Case JB, Winkler ES, Liu Y, VanBlargan LA, et al. (March 2021). "Resistance of SARS-CoV-2 variants to neutralization by monoclonal and serum-derived polyclonal antibodies". Nature Medicine. 27 (4): 717–726. doi:10.1038/s41591-021-01294-w. PMC 8058618. PMID 33664494.
{{cite journal}}: CS1 maint: PMC embargo expired (link) - ↑ "B.1.1.7 Lineage with S:E484K Report". outbreak.info. 5 March 2021. Archived from the original on 7 March 2021. Retrieved 7 March 2021.
- ↑ Moustafa AM, Bianco C, Denu L, Ahmed A, Neide B, Everett J, et al. (21 April 2021). "Comparative Analysis of Emerging B.1.1.7+E484K SARS-CoV-2 isolates from Pennsylvania". bioRxiv 10.1101/2021.04.21.440801v1.
- ↑ B.1.1.7 Lineage with S:E484K Report Archived 3 July 2021 at the Wayback Machine, outbreak.info
- 1 2 3 4 "South Africa announces a new coronavirus variant". The New York Times. 18 December 2020. Archived from the original on 21 December 2020. Retrieved 20 December 2020.
- 1 2 Wroughton L, Bearak M (18 December 2020). "South Africa coronavirus: Second wave fueled by new strain, teen 'rage festivals'". The Washington Post. Archived from the original on 27 December 2020. Retrieved 20 December 2020.
- ↑ Mkhize Z (18 December 2020). "Update on Covid-19 (18th December 2020)" (Press release). South Africa. COVID-19 South African Online Portal. Archived from the original on 4 May 2021. Retrieved 23 December 2020.
Our clinicians have also warned us that things have changed and that younger, previously healthy people are now becoming very sick.
- ↑ Abdool Karim, Salim S. (19 December 2020). "The 2nd Covid-19 wave in South Africa:Transmissibility & a 501.V2 variant, 11th slide". www.scribd.com. Archived from the original on 6 January 2021. Retrieved 18 June 2021.
- ↑ Lowe D (22 December 2020). "The New Mutations". In the Pipeline. American Association for the Advancement of Science. Archived from the original on 29 January 2021. Retrieved 23 December 2020.
I should note here that there's another strain in South Africa that is bringing on similar concerns. This one has eight mutations in the Spike protein, with three of them (K417N, E484K and N501Y) that may have some functional role.
- ↑ "Statement of the WHO Working Group on COVID-19 Animal Models (WHO-COM) about the UK and South African SARS-CoV-2 new variants" (PDF). World Health Organization. 22 December 2020. Archived (PDF) from the original on 4 May 2021. Retrieved 23 December 2020.
- ↑ "Novel mutation combination in spike receptor binding site" (Press release). GISAID. 21 December 2020. Archived from the original on 22 February 2021. Retrieved 23 December 2020.
- ↑ "Japan finds new coronavirus variant in travelers from Brazil". Japan Today. Japan. 11 January 2021. Archived from the original on 11 January 2021. Retrieved 14 January 2021.
- 1 2 3 4 5 6 Faria NR, Claro IM, Candido D, Moyses Franco LA, Andrade PS, Coletti TM, et al. (12 January 2021). "Genomic characterisation of an emergent SARS-CoV-2 lineage in Manaus: preliminary findings". CADDE Genomic Network. virological.org. Archived from the original on 20 May 2021. Retrieved 23 January 2021.
- ↑ "P.1". cov-lineages.org. Pango team. Archived from the original on 9 June 2021. Retrieved 22 March 2021.
- ↑ Covid-19 Genomics UK Consortium (15 January 2021). "COG-UK Report on SARS-CoV-2 Spike mutations of interest in the UK" (PDF). www.cogconsortium.uk. Archived (PDF) from the original on 16 April 2021. Retrieved 25 January 2021.
- ↑ "P.1 report". cov-lineages.org. Archived from the original on 9 June 2021. Retrieved 8 February 2021.
- 1 2 3 Voloch CM, da Silva Francisco R, de Almeida LG, Cardoso CC, Brustolini OJ, Gerber AL, et al. (Covid19-UFRJ Workgroup) (2020). "Genomic characterization of a novel SARS-CoV-2 lineage from Rio de Janeiro, Brazil". MedRxiv: 2020.12.23.20248598. doi:10.1101/2020.12.23.20248598. S2CID 229379623. Archived from the original on 29 June 2021. Retrieved 18 June 2021.
- ↑ Nascimento V, Souza V (25 February 2021). "COVID-19 epidemic in the Brazilian state of Amazonas was driven by long-term persistence of endemic SARS-CoV-2 lineages and the recent emergence of the new Variant of Concern P.1". Research Square. doi:10.21203/rs.3.rs-275494/v1. Archived from the original on 1 March 2021. Retrieved 2 March 2021.
{{cite journal}}: Cite journal requires|journal=(help) - ↑ Andreoni M, Londoño E, Casado L (3 March 2021). "Brazil's Covid Crisis Is a Warning to the Whole World, Scientists Say – Brazil is seeing a record number of deaths, and the spread of a more contagious coronavirus variant that may cause reinfection". The New York Times. Archived from the original on 3 March 2021. Retrieved 3 March 2021.
- ↑ Zimmer C (1 March 2021). "Virus Variant in Brazil Infected Many Who Had Already Recovered From Covid-19 – The first detailed studies of the so-called P.1 variant show how it devastated a Brazilian city. Now scientists want to know what it will do elsewhere". The New York Times. Archived from the original on 3 March 2021. Retrieved 3 March 2021.
- ↑ Garcia-Beltran W, Lam E, Denis K (12 March 2021). "Circulating SARS-CoV-2 variants escape neutralization by vaccine-induced humoral immunity". doi:10.1101/2021.02.14.21251704. Archived from the original on 13 April 2021. Retrieved 14 April 2021 – via medrxiv.
- ↑ Sofia Moutinho (4 May 2021). "Chinese COVID-19 vaccine maintains protection in variant-plagued Brazil". Archived from the original on 16 June 2021. Retrieved 18 June 2021.
- ↑ Gaier R (5 March 2021). "Exclusive: Oxford study indicates AstraZeneca effective against Brazil variant, source says". Reuters. Rio de Janeiro. Archived from the original on 9 March 2021. Retrieved 9 March 2021.
- ↑ "Exclusive: Oxford study indicates AstraZeneca effective against Brazil variant, source says". Reuters. Rio de Janeiro. 8 March 2021. Archived from the original on 9 March 2021. Retrieved 9 March 2021.
- ↑ Simões E, Gaier R (8 March 2021). "CoronaVac e Oxford são eficazes contra variante de Manaus, dizem laboratórios" [CoronaVac and Oxford are effective against Manaus variant, say laboratories]. UOL Notícias (in português). Reuters Brazil. Archived from the original on 8 March 2021. Retrieved 9 March 2021.
- ↑ "PANGO lineages". cov-lineages.org. Archived from the original on 3 June 2021. Retrieved 18 April 2021.
- 1 2 3 4 Koshy J (8 April 2021). "Coronavirus | Indian 'double mutant' strain named B.1.617". The Hindu. Archived from the original on 26 May 2021. Retrieved 18 June 2021.
- ↑ "India's variant-fuelled second wave coincided with spike in infected flights landing in Canada". Toronto Sun. 10 April 2021. Archived from the original on 2 June 2021. Retrieved 10 April 2021.
- ↑ "Weekly epidemiological update on COVID-19 - 11 May 2021". World Health Organization. 11 May 2021. Archived from the original on 11 May 2021. Retrieved 12 May 2021.
- ↑ "COVID strain first detected in India found in 53 territories: WHO". Archived from the original on 19 June 2021. Retrieved 18 June 2021.
- ↑ "British scientists warn over Indian coronavirus variant". Reuters. 7 May 2021. Archived from the original on 22 May 2021. Retrieved 7 May 2021.
- ↑ "SARS-CoV-2 variants of concern as of 6 May 2021". European Centre for Disease Prevention and Control. Archived from the original on 16 June 2021. Retrieved 12 May 2021.
- ↑ "expert reaction to VUI-21APR-02/B.1.617.2 being classified by PHE as a variant of concern". Science Media Centre. 7 May 2021. Archived from the original on 13 July 2021. Retrieved 15 May 2021.
- ↑ SARS-CoV-2 variants of concern and variants under investigation in England ― Technical briefing 15 (PDF). London: Public Health England. 11 June 2021. Archived (PDF) from the original on 11 June 2021. Retrieved 12 June 2021.
- ↑ Pearson, Heide; Pullen, Lauren; Dao, Christa (11 June 2021). "AHS breaks down vaccination data of COVID-19 Delta variant outbreak at Calgary hospital". Global News. Archived from the original on 12 June 2021. Retrieved 12 June 2021.
- ↑ Sharma, Milan. "New 'Delta Plus' variant of SARS-CoV-2 identified; here's what we know so far". India Today. Archived from the original on 17 June 2021. Retrieved 16 June 2021.
- ↑ "Southern California COVID-19 Strain Rapidly Expands Global Reach". Cedars-Sinai Newsroom. Los Angeles. 11 February 2021. Archived from the original on 16 April 2021. Retrieved 17 March 2021.
- ↑ B.1.429 Lineage Report. Alaa Abdel Latif, Julia L. Mullen, Manar Alkuzweny, Ginger Tsueng, Marco Cano, Emily Haag, Jerry Zhou, Mark Zeller, Nate Matteson, Chunlei Wu, Kristian G. Andersen, Andrew I. Su, Karthik Gangavarapu, Laura D. Hughes, and the Center for Viral Systems Biology. outbreak.info, (available at https://outbreak.info/situation-reports?pango=B.1.429&loc=USA&loc=USA_US-CA&selected=USA_US-CA Archived 3 July 2021 at the Wayback Machine). Accessed 28 May 2021.
- 1 2 3 "New California Variant May Be Driving Virus Surge There, Study Suggests". The New York Times. 19 January 2021. Archived from the original on 9 June 2021. Retrieved 18 June 2021.
- ↑ "SARS-CoV-2 Variant Classifications and Definitions". CDC.gov. Centers for Disease Control and Prevention. 24 March 2021. Archived from the original on 16 June 2021. Retrieved 4 April 2021.
- ↑ Shen X, Tang H, Pajon R, Smith G, Glenn GM, Shi W, et al. (April 2021). "Neutralization of SARS-CoV-2 Variants B.1.429 and B.1.351". The New England Journal of Medicine. doi:10.1056/NEJMc2103740. PMC 8063884. PMID 33826819.
- ↑ "Local COVID-19 Strain Found in Over One-Third of Los Angeles Patients". news wise (Press release). California: Cedars Sinai Medical Center. 19 January 2021. Archived from the original on 13 June 2021. Retrieved 3 March 2021.
- 1 2 "B.1.429". Rambaut Group, University of Edinburgh. PANGO Lineages. 15 February 2021. Archived from the original on 28 April 2021. Retrieved 16 February 2021.
- 1 2 "B.1.429 Lineage Report". Scripps Research. outbreak.info. 15 February 2021. Archived from the original on 9 June 2021. Retrieved 16 February 2021.
- ↑ "COVID-19 Variant First Found in Other Countries and States Now Seen More Frequently in California". California Department of Public Health. Archived from the original on 16 June 2021. Retrieved 30 January 2021.
- ↑ Weise E, Weintraub K. "New strains of COVID swiftly moving through the US need careful watch, scientists say". USA Today. Archived from the original on 4 March 2021. Retrieved 30 January 2021.
- 1 2 Zimmer, Carl; Mandavilli, Apoorva (14 May 2021). "How the United States Beat the Variants, for Now". New York Times. Archived from the original on 16 May 2021. Retrieved 17 May 2021.
- ↑ "PANGO lineages Lineage P.2". COV lineages. Archived from the original on 28 April 2021. Retrieved 28 January 2021.
P.2… Alias of B.1.1.28.2, Brazilian lineage
- ↑ "Delta-PCR-testen" [The Delta PCR Test] (in Danish). Statens Serum Institut. 25 February 2021. Archived from the original on 2 May 2021. Retrieved 27 February 2021.
{{cite web}}: CS1 maint: unrecognized language (link) - 1 2 "GISAID hCOV19 Variants (see menu option 'G/484K.V3 (B.1.525)')". GISAID. Archived from the original on 23 June 2021. Retrieved 4 March 2021.
- 1 2 "Status for udvikling af SARS-CoV-2 Variants of Concern (VOC) i Danmark" [Status of development of SARS-CoV-2 Variants of Concern (VOC) in Denmark] (in Danish). Statens Serum Institut. 27 February 2021. Archived from the original on 1 May 2021. Retrieved 27 February 2021.
{{cite web}}: CS1 maint: unrecognized language (link) - ↑ "Varianten van het coronavirus SARS-CoV-2" [Variants of the coronavirus SARS-CoV-2] (in Dutch). Rijksinstituut voor Volksgezondheid en Milieu, RIVM. 16 February 2021. Archived from the original on 16 February 2021. Retrieved 16 February 2021.
{{cite web}}: CS1 maint: unrecognized language (link) - ↑ "A coronavirus variant with a mutation that 'likely helps it escape' antibodies is already in at least 11 countries, including the US". Business Insider. 16 February 2021. Archived from the original on 22 February 2021. Retrieved 16 February 2021.
- ↑ "En ny variant av koronaviruset er oppdaget i Norge. Hva vet vi om den?" [A new variant of the coronavirus has been discovered in Norway. What do we know about it?] (in Norwegian). Aftenposten. 18 February 2021. Archived from the original on 27 August 2021. Retrieved 18 February 2021.
{{cite news}}: CS1 maint: unrecognized language (link) - ↑ Cullen P (25 February 2021). "Coronavirus: Variant discovered in UK and Nigeria found in State for first time". The Irish Times. Archived from the original on 25 February 2021. Retrieved 25 February 2021. Gataveckaite G (25 February 2021). "First Irish case of B1525 strain of Covid-19 confirmed as R number increases". Irish Independent. Archived from the original on 25 February 2021. Retrieved 25 February 2021. McGlynn M (25 February 2021). "Nphet confirm new variant B1525 detected in Ireland as 35 deaths and 613 cases confirmed". Irish Examiner. Archived from the original on 27 February 2021. Retrieved 25 February 2021.
- ↑ Roberts M (16 February 2021). "Another new coronavirus variant seen in the UK". BBC News. Archived from the original on 20 June 2021. Retrieved 16 February 2021.
- ↑ "DOH confirms detection of 2 SARS-CoV-2 mutations in Region 7". ABS-CBN News. 18 February 2021. Archived from the original on 3 May 2021. Retrieved 13 March 2021.
- ↑ Santos E (13 March 2021). "DOH reports COVID-19 variant 'unique' to PH, first case of Brazil variant". CNN Philippines. Archived from the original on 16 March 2021. Retrieved 17 March 2021.
- ↑ "DOH confirms new COVID-19 variant first detected in PH, first case of Brazil variant". ABS-CBN News. 13 March 2021. Archived from the original on 2 May 2021. Retrieved 13 March 2021.
- ↑ "PH discovered new COVID-19 variant earlier than Japan, expert clarifies". CNN Philippines. 13 March 2021. Archived from the original on 17 March 2021. Retrieved 17 March 2021.
- ↑ "Japan detects new coronavirus variant from traveler coming from PH". CNN Philippines. 13 March 2021. Archived from the original on 17 March 2021. Retrieved 21 March 2021.
- ↑ "UK reports 2 cases of COVID-19 variant first detected in Philippines". ABS-CBN. 17 March 2021. Archived from the original on 18 March 2021. Retrieved 21 March 2021.
- ↑ "Covid-19: Sarawak detects variant reported in the Philippines". 30 April 2021. Archived from the original on 1 May 2021. Retrieved 30 April 2021.
- ↑ Mandavilli A (24 February 2021). "A New Coronavirus Variant Is Spreading in New York, Researchers Report". The New York Times. Archived from the original on 26 April 2021. Retrieved 18 June 2021.
- ↑ "Tracking SARS-CoV-2 variants". www.who.int. 31 May 2021. Archived from the original on 9 June 2021. Retrieved 5 June 2021.
- ↑ Weekly epidemiological update on COVID-19 - 27 April 2021 (Situation report). World Health Organization. 27 April 2021. Retrieved 14 June 2021.
- ↑ Le Page, Michael (4 June 2021). "Indian covid-19 variant (B.1.617)". New Scientist. Archived from the original on 23 June 2021. Retrieved 8 June 2021.
- ↑ SARS-CoV-2 variants of concern and variants under investigation in England - Technical briefing 10 (PDF) (Report). London. Public Health England. 7 May 2021. Archived (PDF) from the original on 8 May 2021. Retrieved 5 June 2021.
A variant first detected in India was designated under investigation on 1 April 2021 as VUI-21APR-01 (B.1.617.1).
File:UKOpenGovernmentLicence.svg This article incorporates text published under the British Open Government Licence v3.0: - ↑ "Tracking SARS-CoV-2 variants". World Health Organization. Archived from the original on 9 June 2021. Retrieved 17 June 2021.
- 1 2 "Detection of SARS-CoV-2 P681H Spike Protein Variant in Nigeria". Virological. 23 December 2020. Archived from the original on 13 June 2021. Retrieved 1 January 2021.
- ↑ "Lineage B.1.1.207". cov-lineages.org. Pango team. Archived from the original on 27 January 2021. Retrieved 11 March 2021.
- 1 2 3 "COVID-19: African variant reveals sequencing lag". Archived from the original on 18 June 2021. Retrieved 18 June 2021.
- ↑ Unidentified coronavirus strain found in eastern Lithuania Archived 3 July 2021 at the Wayback Machine 20 April 2021 www.lrt.lt accessed 6 May 2021
- ↑ "The travel-related origin and spread of SARS-CoV-2 B.1.620 strain". Archived from the original on 3 June 2021. Retrieved 18 June 2021.
- ↑ New coronavirus variant found in West Bengal Archived 26 May 2021 at the Wayback Machine www.thehindu.com, accessed 23 April 2021
- ↑ What is the new 'triple mutant variant' of Covid-19 virus found in Bengal? How bad is it? Archived 28 April 2021 at the Wayback Machine www.indiatoday.in, accessed 23 April 2021
- ↑ PANGO lineages Lineage B.1.618 Archived 14 May 2021 at the Wayback Machine cov-lineages.org, accessed 23 April 2021
- ↑ "Latest update: New Variant Under Investigation designated in the UK". GOV.UK. 4 March 2021. Archived from the original on 7 May 2021. Retrieved 5 March 2021.
- ↑ "Queensland travellers have hotel quarantine extended after Russian variant of coronavirus detected". www.abc.net.au. 3 March 2021. Archived from the original on 3 March 2021. Retrieved 3 March 2021.
- ↑ Peltier, Elain; Kolata, Gina (29 May 2021). "Vietnam says it has detected a more contagious hybrid of variants first seen in India and Britain". The New York Times. Archived from the original on 29 May 2021. Retrieved 29 May 2021.
- ↑ ‘No New Hybrid Variant’ In Vietnam, World Health Organization Official Says Archived 12 June 2021 at the Wayback Machine 3 June 2021, www.forbes.com, accessed 13 June 2021
- ↑ Lassaunière R, Fonager J, Rasmussen M, Frische A, Strandh C, Rasmussen T, et al. (10 November 2020). SARS-CoV-2 spike mutations arising in Danish mink, their spread to humans and neutralization data (Preprint). Statens Serum Institut. Archived from the original on 10 November 2020. Retrieved 11 November 2020.
- ↑ "Detection of new SARS-CoV-2 variants related to mink" (PDF). ECDC.eu. European Centre for Disease Prevention and Control. 12 November 2020. Archived (PDF) from the original on 8 January 2021. Retrieved 12 November 2020.
- ↑ "SARS-CoV-2 mink-associated variant strain – Denmark". WHO Disease Outbreak News. 6 November 2020. Archived from the original on 12 November 2020. Retrieved 19 March 2021.
- ↑ "Danish Covid mink variant 'very likely extinct', but controversial cull continues". Archived from the original on 24 April 2021. Retrieved 18 June 2021.
- ↑ Larsen HD, Fonager J, Lomholt FK, Dalby T, Benedetti G, Kristensen B, et al. (February 2021). "Preliminary report of an outbreak of SARS-CoV-2 in mink and mink farmers associated with community spread, Denmark, June to November 2020". Euro Surveillance. 26 (5). doi:10.2807/1560-7917.ES.2021.26.5.210009. PMC 7863232. PMID 33541485.
- ↑ "Archive copy". Archived from the original on 8 June 2021. Retrieved 18 June 2021.
{{cite web}}: CS1 maint: archived copy as title (link) - 1 2 3 4 5 Greenwood M (15 January 2021). ""What Mutations of SARS-CoV-2 are Causing Concern?"]". News Medical Lifesciences. Archived from the original on 16 January 2021. Retrieved 16 January 2021.
- ↑ Tandel, Dixit; Gupta, Divya; Sah, Vishal; Harshan, Krishnan Harinivas (30 April 2021). "N440K variant of SARS-CoV-2 has Higher Infectious Fitness". bioRxiv: 2021.04.30.441434. doi:10.1101/2021.04.30.441434. Archived from the original on 12 May 2021. Retrieved 18 June 2021.
- ↑ Bhattacharjee, Sumit (3 May 2021). "COVID-19 | A.P. strain at least 15 times more virulent". The Hindu. Archived from the original on 10 May 2021. Retrieved 18 June 2021.
- ↑ "Hyderabad: Mutant N440K 10 times more infectious than parent strain". Archived from the original on 3 May 2021. Retrieved 18 June 2021.
- ↑ "University of Graz". www.uni-graz.at. Archived from the original on 6 May 2021. Retrieved 22 February 2021.
- ↑ "Coronavirus SARS-CoV-2 (formerly known as Wuhan coronavirus and 2019-nCoV) – what we can find out on a structural bioinformatics level". Innophore. 23 January 2020. Archived from the original on 13 December 2021. Retrieved 22 February 2021.
- ↑ Singh A, Steinkellner G, Köchl K, Gruber K, Gruber CC (February 2021). "Serine 477 plays a crucial role in the interaction of the SARS-CoV-2 spike protein with the human receptor ACE2". Scientific Reports. 11 (1): 4320. Bibcode:2021NatSR..11.4320S. doi:10.1038/s41598-021-83761-5. PMC 7900180. PMID 33619331.
- ↑ "BioNTech: We aspire to individualize cancer medicine". BioNTech. Archived from the original on 18 June 2021. Retrieved 22 February 2021.
- ↑ Schroers B, Gudimella R, Bukur T, Roesler T, Loewer M, Sahin U (4 February 2021). "Large-scale analysis of SARS-CoV-2 spike-glycoprotein mutants demonstrates the need for continuous screening of virus isolates". bioRxiv: 2021.02.04.429765. doi:10.1101/2021.02.04.429765. S2CID 231885609. Archived from the original on 9 June 2021. Retrieved 18 June 2021.
- 1 2 3 Mandavilli A, Mueller B (2 March 2021). "Why Virus Variants Have Such Weird Names". The New York Times. ISSN 0362-4331. Archived from the original on 20 June 2021. Retrieved 2 March 2021.
- ↑ "escape mutation". HIV i-Base. 11 October 2012. Archived from the original on 9 May 2021. Retrieved 19 February 2021.
- ↑ Wise J (February 2021). "Covid-19: The E484K mutation and the risks it poses". BMJ. 372: n359. doi:10.1136/bmj.n359. PMID 33547053. S2CID 231821685.
- 1 2 3 "Brief report: New Variant Strain of SARS-CoV-2 Identified in Travelers from Brazil" (PDF) (Press release). Japan: NIID (National Institute of Infectious Diseases). 12 January 2021. Archived (PDF) from the original on 15 January 2021. Retrieved 14 January 2021.
- ↑ "Technical briefing 5" (PDF). GOV.UK. Public Health England. p. 17. Archived (PDF) from the original on 2 February 2021. Retrieved 2 February 2021.
- ↑ Greaney A (4 January 2021). "Comprehensive mapping of mutations to the SARS-CoV-2 receptor-binding domain that affect recognition by polyclonal human serum antibodies". bioRxiv 10.1101/2020.12.31.425021.
- ↑ Kupferschmidt K (January 2021). "New mutations raise specter of 'immune escape'". Science. 371 (6527): 329–330. Bibcode:2021Sci...371..329K. doi:10.1126/science.371.6527.329. PMID 33479129.
- ↑ Rettner R (2 February 2021). "UK coronavirus variant develops vaccine-evading mutation – In a handful of instances, the U.K. coronavirus variant has developed a mutation called E484K, which may impact vaccine effectiveness". Live Science. Archived from the original on 2 February 2021. Retrieved 2 February 2021.
- ↑ Achenbach J, Booth W (2 February 2021). "Worrisome coronavirus mutation seen in U.K. variant and in some U.S. samples". The Washington Post. Archived from the original on 2 February 2021. Retrieved 2 February 2021.
- ↑ "People Are Talking About A 'Double Mutant' Variant In India. What Does That Mean?". NPR.org. Archived from the original on 27 April 2021. Retrieved 27 April 2021.
...scientifically, the term "double mutant" makes no sense, Andersen says. "SARS-CoV-2 mutates all the time. So there are many double mutants all over the place. The variant in India really shouldn't be called that."
- 1 2 COG-UK update on SARS-CoV-2 Spike mutations of special interest: Report 1 (PDF) (Report). COVID-19 Genomics UK Consortium (COG-UK). 20 December 2020. p. 7. Archived from the original (PDF) on 25 December 2020. Retrieved 31 December 2020.
- ↑ "Researchers Discover New Variant of COVID-19 Virus in Columbus, Ohio". wexnermedical.osu.edu. 13 January 2021. Archived from the original on 15 January 2021. Retrieved 16 January 2021.
- ↑ Tu H, Avenarius MR, Kubatko L, Hunt M, Pan X, Ru P, et al. (26 January 2021). "Distinct Patterns of Emergence of SARS-CoV-2 Spike Variants including N501Y in Clinical Samples in Columbus Ohio". bioRxiv: 2021.01.12.426407. doi:10.1101/2021.01.12.426407. S2CID 231666860. Archived from the original on 3 June 2021. Retrieved 18 June 2021.
- 1 2 3 Maison DP, Ching LL, Shikuma CM, Nerurkar VR (January 2021). "Genetic Characteristics and Phylogeny of 969-bp S Gene Sequence of SARS-CoV-2 from Hawaii Reveals the Worldwide Emerging P681H Mutation". bioRxiv: 2021.01.06.425497. doi:10.1101/2021.01.06.425497. PMC 7805472. PMID 33442699.
 Available under CC BY 4.0 Archived 16 October 2017 at the Wayback Machine.
Available under CC BY 4.0 Archived 16 October 2017 at the Wayback Machine. - ↑ Schraer R (18 July 2020). "Coronavirus: Are mutations making it more infectious?". BBC News. Archived from the original on 30 December 2020. Retrieved 3 January 2021.
- ↑ "New, more infectious strain of COVID-19 now dominates global cases of virus: study". medicalxpress.com. Archived from the original on 17 November 2020. Retrieved 16 August 2020.
- ↑ Korber B, Fischer WM, Gnanakaran S, Yoon H, Theiler J, Abfalterer W, et al. (August 2020). "Tracking Changes in SARS-CoV-2 Spike: Evidence that D614G Increases Infectivity of the COVID-19 Virus". Cell. 182 (4): 812–827.e19. doi:10.1016/j.cell.2020.06.043. PMC 7332439. PMID 32697968.
- ↑ Hou YJ, Chiba S, Halfmann P, Ehre C, Kuroda M, Dinnon KH, et al. (December 2020). "SARS-CoV-2 D614G variant exhibits efficient replication ex vivo and transmission in vivo". Science. 370 (6523): 1464–1468. Bibcode:2020Sci...370.1464H. doi:10.1126/science.abe8499. PMC 7775736. PMID 33184236.
an emergent Asp614→Gly (D614G) substitution in the spike glycoprotein of SARS-CoV-2 strains that is now the most prevalent form globally
- ↑ Butowt R, Bilinska K, Von Bartheld CS (October 2020). "Chemosensory Dysfunction in COVID-19: Integration of Genetic and Epidemiological Data Points to D614G Spike Protein Variant as a Contributing Factor". ACS Chemical Neuroscience. 11 (20): 3180–3184. doi:10.1021/acschemneuro.0c00596. PMC 7581292. PMID 32997488.
- ↑ "Study shows P681H mutation is becoming globally prevalent among SARS-CoV-2 sequences". News-Medical.net. 10 January 2021. Archived from the original on 14 February 2021. Retrieved 11 February 2021.
- ↑ "Malaysia identifies new Covid-19 strain, similar to one found in 3 other countries". The Straits Times. 23 December 2020. Archived from the original on 23 December 2020. Retrieved 10 January 2021.
Tan Sri Dr Noor Hisham Abdullah, said it is still unknown whether the strain - dubbed the "A701B" mutation - is more infectious than usual
- ↑ "Duterte says Sulu seeking help after new COVID-19 variant detected in nearby Sabah, Malaysia". GMA News. 27 December 2020. Archived from the original on 3 January 2021. Retrieved 10 January 2021.
- 1 2 3 "The current situation and Information on the Spike protein mutation of Covid-19 in Malaysia". Kementerian Kesihatan Malaysia/ covid-19 Malaysia/ covid-19.moh.gov.my. 25 December 2020. Archived from the original on 2 July 2021. Retrieved 15 January 2021.
- 1 2 3 COVID-19 A701V mutation spreads to third wave clusters Archived 14 May 2021 at the Wayback Machine 25 December 2020 focusmalaysia.my, accessed 13 May 2021
- 1 2 The current situation and Information on the Spike protein mutation of Covid-19 in Malaysia Archived 2 July 2021 at the Wayback Machine 25 December 2020 covid-19.moh.gov.my, accessed 13 May 2021
- ↑ Variants of Concerns (VOC), B.1.524, B.1.525, South African B.1.351, STRAIN D614G, A701V, B1.1.7 Archived 2 July 2021 at the Wayback Machine 14 April 2021, covid-19.moh.gov.my, accessed 15 May 2021
- ↑ Smout A (26 January 2021). "Britain to help other countries track down coronavirus variants". Reuters. Archived from the original on 26 January 2021. Retrieved 27 January 2021.
- ↑ Donnelly L (26 January 2021). "UK to help sequence mutations of Covid around world to find dangerous new variants". The Telegraph. Archived from the original on 27 January 2021. Retrieved 28 January 2021.
- ↑ Kupferschmidt K (23 December 2020). "U.K. variant puts spotlight on immunocompromised patients' role in the COVID-19 pandemic". Science. Archived from the original on 24 June 2021. Retrieved 18 June 2021.
- ↑ Sutherland S (23 February 2021). "COVID Variants May Arise in People with Compromised Immune Systems". Scientific American. Archived from the original on 6 June 2021. Retrieved 18 June 2021.
- ↑ McCarthy KR, Rennick LJ, Nambulli S, Robinson-McCarthy LR, Bain WG, Haidar G, Duprex WP (March 2021). "Recurrent deletions in the SARS-CoV-2 spike glycoprotein drive antibody escape". Science. 371 (6534): 1139–1142. Bibcode:2021Sci...371.1139M. doi:10.1126/science.abf6950. PMC 7971772. PMID 33536258.