Pelvic Organ Prolapse Quantification System
| Pelvic Organ Prolapse Quantification System | |
|---|---|
| Purpose | assessing the degree of prolapse of pelvic organs |
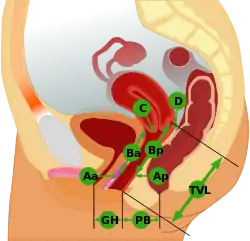
The Pelvic Organ Prolapse Quantifications System (POP-Q) is a system for assessing the degree of prolapse of pelvic organs to help standardize diagnosing, comparing, documenting, and sharing of clinical findings.[1][2] This assessment is the most frequently used[3][4] among research publications related to pelvic organ prolapse.[4]
When assessed using the POP-Q, the prevalence of pelvic organ prolapse is estimated to be up to 50% while diagnosis by symptoms has a prevalence of 3–6%.[2] Some advocate that the system of assessment be modified.[5]
The POP-Q was developed in 1996; it quantifies the descent of pelvic organs into the vagina.[3][6][2] The POP-Q provides reliable description of the support of the anterior, posterior and apical vaginal wall. It uses objective and precise distance measurements to the reference point, the hymen. Cystocele and prolapse of the vagina from other causes is staged using POP-Q criteria and can range from good support (no descent into the vagina) reported as a POP-Q stage 0 or I to a POP-Q score of IV, which includes prolapse beyond the hymen. It also used to quantify the movement of other structures into the vaginal lumen and their descent.[6][2]
Stages
| Stage | Description |
|---|---|
| 0 | No prolapse anterior and posterior points are all −3 cm, and C or D is between −TVL and −(TVL−2) cm. |
| 1 | The criteria for stage 0 are not met, and the most distal prolapse is more than 1 cm above the level of the hymen (less than −1 cm). |
| 2 | The most distal prolapse is between 1 cm above and 1 cm below the hymen (at least one point is −1, 0, or +1). |
| 3 | The most distal prolapse is more than 1 cm below the hymen but no further than 2 cm less than TVL. |
| 4 | Represents complete procidentia or vault eversion; the most distal prolapse protrudes to at least (TVL−2) cm. |
The POP-Q assessment tool measures nine points in the vagina. The hymen is the reference point to which the other points are compared. The prolapsed organs are measured in centimeters to the hymen. The measurements are taken when the Valsalva maneuver is performed while The woman is in the dorsal lithotomy position.[7][3] The anatomical landmarks used are anterior vaginal wall, cervix, hymen, perineal body, total vaginal length, posterior vaginal wall and posterior fornix.[8] A three-by-three centimeter grid is used to record the proximal and distal numbers. The information on the grid is translated to the appropriate stage of prolapse.[3]
This system of assessing pelvic organ prolapse is used widely in China and the US.[9]
Other assessments
Other assessment tools are abailable to determine the impact of pelvic floor prolapse. These are Pelvic Floor Impact Questionnaire (PFIQ), The Pelvic Floor Distress Inventory (PFDI) and the shorter forms PFIQ-7 and PFDI-20.[7]
The evaluation of pelvic organ prolapse includes other diagnostic tests in addition to the POP-Q. These can be:[3]
- voiding cystometry
- ultrasound
- defecating proctography
- anal manometry
- electromyography
- MRI
In the US, greater than 200,000 surgeries are performed each year for pelvic organ prolapse. Examples of pelvic organ prolapse are cystocele, rectocele, urethrocele, enterocele and sigmoidocele. Cystocele is the most common.[10][2]
History
The Porges or Severity prolapse assessment system was proposed in 1963.[11] In 1972, the Baden–Walker Halfway Scoring System was developed and is the second most used system.[11][1] In 1980, the Beecham system was developed. The POP was developed in 1996.[11]
See also
References
- 1 2 Persu, C; Chapple, CR; Cauni, V; Gutue, S; Geavlete, P (2011-02-15). "Pelvic Organ Prolapse Quantification System (POP–Q) – a new era in pelvic prolapse staging". Journal of Medicine and Life. 4 (1): 75–81. ISSN 1844-122X. PMC 3056425. PMID 21505577.
- 1 2 3 4 5 Barber, Matthew D.; Maher, Christopher (2013-11-01). "Epidemiology and outcome assessment of pelvic organ prolapse". International Urogynecology Journal. 24 (11): 1783–1790. doi:10.1007/s00192-013-2169-9. ISSN 0937-3462. PMID 24142054. S2CID 9305151.
- 1 2 3 4 5 Beckley, Ian; Harris, Neil (2013-03-26). "Pelvic organ prolapse: a urology perspective". Journal of Clinical Urology. 6 (2): 68–76. doi:10.1177/2051415812472675. S2CID 75886698.
- 1 2 Boyd, S. S.; O'Sullivan, D. M.; Tulikangas, P. (2017-03-01). "29: Implementation of the pelvic organ prolapse quantification system in peer-reviewed journals". American Journal of Obstetrics & Gynecology. 216 (3): S591. doi:10.1016/j.ajog.2016.12.076. ISSN 0002-9378.
- ↑ Oyama, Ian A.; Steinberg, Adam C.; Watai, Travis K.; Minaglia, Steven M. (2012). "Pelvic Organ Prolapse Quantification Use in the Literature". Female Pelvic Medicine & Reconstructive Surgery. 18 (1): 33–34. doi:10.1097/spv.0b013e31823bd1ab. PMID 22453265. S2CID 26251358.
- 1 2 Hoffman, Barbara L.; Williams, J. Whitridge (2012). Williams gynecology (2nd ed.). New York: McGraw-Hill Medical. pp. 647–653. ISBN 9780071716727. OCLC 779244257.
- 1 2 Sengupta, Niladri; Hilliard, Timothy (2013). "Urogynecological Risk Assessment in Postmenopausal Women". www.medscape.com. Retrieved 2017-12-29.
- ↑ Practitioners, The Royal Australian College of General. "RACGP – Pelvic organ prolapse – a review". www.racgp.org.au. Retrieved 2017-12-29.
- ↑ Wang, Yi-ting; Jiang, Jun-ying; Han, Jin-song (2016-02-01). "A review of the pelvic organ prolapse quantification system in China". International Urogynecology Journal. 27 (2): 287–290. doi:10.1007/s00192-015-2830-6. ISSN 0937-3462. PMID 26353847. S2CID 20771630.
- ↑ Halpern-Elenskaia, Ksenia; Umek, Wolfgang; Bodner-Adler, Barbara; Hanzal, Engelbert (2017-12-06). "Anterior colporrhaphy: a standard operation? Systematic review of the technical aspects of a common procedure in randomized controlled trials". International Urogynecology Journal. 29 (6): 781–788. doi:10.1007/s00192-017-3510-5. ISSN 0937-3462. PMC 5948274. PMID 29214325.
- 1 2 3 Zimmern, Philippe E.; Haab, Francois; Chapple, Christopher R. (2007-12-09). Vaginal Surgery for Incontinence and Prolapse. Springer Science & Business Media. p. 40. ISBN 9781846283468.