Retinopathy of prematurity
| Retinopathy of prematurity | |
|---|---|
| Other names: Terry syndrome,[1] retrolental fibroplasia (RLF) | |
 | |
| Hybrid form of retinopathy of prematurity, zone 1 disease in right eye, aggressive posterior retinopathy of prematurity in left eye. | |
Retinopathy of prematurity (ROP), also called retrolental fibroplasia (RLF) and Terry syndrome, is a disease of the eye affecting prematurely born babies generally having received neonatal intensive care, in which oxygen therapy is used due to the premature development of their lungs. It is thought to be caused by disorganized growth of retinal blood vessels which may result in scarring and retinal detachment. ROP can be mild and may resolve spontaneously, but it may lead to blindness in serious cases. Thus, all preterm babies are at risk for ROP, and very low birth-weight is an additional risk factor. Both oxygen toxicity and relative hypoxia can contribute to the development of ROP.
Signs and symptoms
The clinical presentation of this ocular condition is consistent with the following:[2]
- Abnormal eye movements
- Severe nearsightedness
- Crossed eye
Causes
By the fourth month of pregnancy, the fetal retina has begun to develop vascularization. Such formation of blood vessels appears to be very sensitive to the amount of oxygen supplied, either naturally or artificially. In rare cases ROP has been found in some patients with a mutation in the NDP gene, which is normally associated with the more damaging Norrie disease.[3][4][5]
Risk factors
Various risk factors contribute to the development of ROP. They are:
- Prematurity[6]
- High exposure to oxygen
- Low birth weight
- Various types of infections
- Cardiac defects
- Anaemia
- Low vitamin E level
Pathophysiology
During development, blood vessels grow from the central part of the retina outwards. This process is completed a few weeks before the normal time of delivery. However, in premature babies it is incomplete. If blood vessels grow normally, ROP does not occur. If the vessels grow and branch abnormally the baby develops ROP. These abnormal blood vessels may grow up from the plane of the retina and may bleed inside the eye. When the blood and abnormal vessels are reabsorbed, it may give rise to multiple band like membranes which can pull up the retina, causing detachment of the retina and eventually blindness before 6 months.
Normally, maturation of the retina proceeds in utero, and at term, the medial portion (Nasal retina) of the retina is fully vascularized, while the lateral portion (Temporal retina) is only incompletely vascularized.[7] The normal growth of the blood vessels is directed to relatively low-oxygen areas of the retina, but the vessels remain in the plane of the retina and do not grow into the vitreous humor. If excess oxygen is given, normal blood vessels degrade and cease to develop. When the excess oxygen environment is removed, the blood vessels rapidly begin forming again and grow into the vitreous humor of the eye from the retina.[7][8]
The key disease element in ROP is fibrovascular proliferation. This is growth of abnormal new vessels; this may regress, but frequently progresses. Associated with the growth of these new vessels is fibrous tissue (scar tissue) that may contract to cause retinal detachment. Multiple factors can determine whether the disease progresses, including overall health, birth weight, the stage of ROP at initial diagnosis, and the presence or absence of "plus disease". Supplemental oxygen exposure, while a risk factor, is not the main risk factor for development of this disease. Restricting supplemental oxygen use reduces the rate of ROP, but may raise the risk of other hypoxia-related systemic complications, including death.[9]
Patients with ROP, particularly those who have developed severe disease needing treatment are at greater risk for strabismus, glaucoma, cataracts and shortsightedness (myopia) later in life and should be examined yearly to help prevent or detect and treat these conditions.
Diagnosis
The stages of ROP disease have been defined by the International Classification of Retinopathy of Prematurity (ICROP).
In older patients, the appearance of the disease is less well described but includes the residua of the ICROP stages as well as secondary retinal responses.
International classification
The system used for describing the findings of active ROP is entitled The International Classification of Retinopathy of Prematurity (ICROP).[10] ICROP uses a number of parameters to describe the disease. They are location (zone) of the disease, the circumferential extent of the disease based on the clock hours, the severity (stage) of the disease and the presence or absence of "Plus Disease". Each aspect of the classification has a technical definition. This classification was used for the major clinical trials. It was revised in 2005.[11]
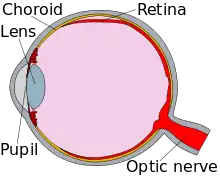
The zones are centered on the optic nerve. Zone I is the posterior zone of the retina, defined as the circle with a radius extending from the optic nerve to double the distance to the macula. Zone II is an annulus with the inner border defined by zone I and the outer border defined by the radius defined as the distance from the optic nerve to the nasal ora serrata. Zone III is the residual temporal crescent of the retina.
The circumferential extent of the disease is described in segments as if the top of the eye were 12 on the face of an analog clock, e.g. stage 1 from 4:00 to 7:00. (The extent is a bit less important since the treatment indications from the Early Treatment for ROP.)[12]
The Stages describe the ophthalmoscopic findings at the junction between the vascularized and avascular retina.
- Stage 1 is a faint demarcation line.
- Stage 2 is an elevated ridge.
- Stage 3 is extraretinal fibrovascular tissue.
- Stage 4 is sub-total retinal detachment.
- Stage 5 is total retinal detachment.
Plus disease
Plus disease can be present as a major complicating factor at any stage. It is characterised by:
- Significant level of vascular dilation and tortuosity observed at the posterior retinal arterioles. This reflects the increase of blood flow through the retina.[13]
- Vitreous haze and anterior chamber haze[13]
- Iris vascular engorgement[13]
- Persistent tunica vasculosa lentis or immature blood vessels growing over the lens which also restrict the dilatation of the pupils.[13]
Differential diagnosis
The most difficult aspect of the differential diagnosis may arise from the similarity of two other diseases:
- Familial exudative vitreoretinopathy which is a genetic disorder that also disrupts the retinal vascularization in full-term infants.
- Persistent fetal vasculature syndrome also known as persistent hyperplastic primary vitreous that can cause a traction retinal detachment difficult to differentiate but typically unilateral.
Screening
Almost all infants with ROP have a gestational age of 31 weeks or less (regardless of birth weight) or a birth weight of 1250 g (2.76 lbs) or less; these indications are generally used to decide whether a baby should be screened for ROP, but some centres, especially in developing countries Archived 28 August 2021 at the Wayback Machine extend birth weight screening criteria to 1500 g (3.3 lbs).[14]
Any premature baby with severe illness in perinatal period (Respiratory distress syndrome, sepsis, blood transfusion, Intra ventricular haemorrhage, apnoeic episodes, etc.) may also be offered ROP screening.
Timing
Retinal examination with scleral depression is generally recommended for patients born before 30–32 weeks gestation, or 4–6 weeks of life, whichever is later. It is then repeated every 1–3 weeks until vascularization is complete (or until disease progression mandates treatment).
Procedure
Following pupillary dilation using eye drops, the retina is examined using a special lighted instrument (an indirect ophthalmoscope). The peripheral portions of the retina are sometimes pushed into view using scleral depression. Examination of the retina of a premature infant is performed to determine how far the retinal blood vessels have grown (the zone), and whether or not the vessels are growing flat along the wall of the eye (the stage). Once the vessels have grown into zone III (see below) it is usually safe to discharge the child from further screening for ROP. The stage of ROP refers to the character of the leading edge of growing retinal blood vessels (at the vascular-avascular border).
Monitoring
In order to allow timely intervention, a system of monitoring is undertaken for infants at risk of developing ROP. These monitoring protocols differ geographically because the definition of high-risk is not uniform or perfectly defined. In the USA the consensus statement of experts is informed by data derived by clinical trials and published in Pediatrics 2006. They included infants with birthweights under 1500 grams or under 30 weeks gestation in most cases. The first examination should take place within the first 4 weeks of birth, and regular, weekly examination is required until it is clear that the eyes are not going to develop disease needing treatment, or one or both eyes develop disease requiring treatment. Treatment should be administered within a 48 hours, as the condition can progress rapidly.
Management
Treatment
- Peripheral retinal ablation is the mainstay of ROP treatment. The destruction of the avascular retina is performed with a solid state laser photocoagulation device, as these are easily portable to the operating room or neonatal ICU. Cryotherapy, an earlier technique in which regional retinal destruction was done using a probe to freeze the desired areas, has also been evaluated in multi-center clinical trials as an effective modality for prevention and treatment of ROP. However, when laser treatment is available, cryotherapy is no longer preferred for routine avascular retinal ablation in premature babies, due to the side effects of inflammation and lid swelling. Furthermore, recent trials have shown that treatment at an earlier stage of the disease gives better results.[15]
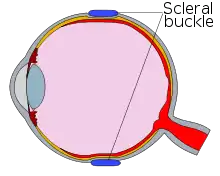
- Scleral buckling and/or vitrectomy surgery may be considered for severe ROP (stages 4 and 5) for eyes that progress to retinal detachment. Few centers in the world specialize in this surgery, because of its attendant surgical risks and generally poor outcomes.
- Intravitreal injection of bevacizumab (Avastin) has been reported as a supportive measure in aggressive posterior retinopathy of prematurity.[16] In a 2011 clinical trial comparing bevacizumab with conventional laser therapy, intravitreal bevacizumab monotherapy showed a significant benefit for zone I but not zone II disease when used to treat infants with stage 3+ retinopathy of prematurity.[17] Potential benefits of intravitreal Avastin injection over laser therapy include: reduction in level of anesthesia required, preservation of viable peripheral retina, and, possibly, reduced incidence of subsequent high refractive error. However, the safety of this new treatment has not yet been established in terms of ocular complications as well as systemic complications. The latter are theoretically possible, as the active ingredient of bevacizumab not only blocks the development of abnormal blood vessels in the eye but may also prevent the normal development ofother tissues such as the lung and kidney. A 2018 Cochrane review also examined the effectiveness of Anti-vascular Endothelial Growth Factor Drugs and their use for ROP.[18]
- Oral propranolol is being evaluated for counteracting the progression of ROP, but safety is a concern. A prospective randomized trial in which pre-term newborns were randomized to receiving oral propranolol with standard treatment or standard treatment alone found that oral propranolol showed a 48% relative risk reduction for progression to stage 3, 58% reduction for progression to stage 3 plus, and 100% reduction for progression to stage 4. Furthermore, there was a 52% relative risk reduction for the need for laser treatment or intravitreal bevacizumab. However 19% of the newborns experienced serious adverse effects including hypotension and bradycardia.[19] A study in a mouse model of human ROP has shown that beta-blockade is protective against retinal angiogenesis and ameliorate blood-retinal barrier dysfunction.[20]
Follow up
- Once diagnosed with ROP lifelong follow up (yearly) is performed in some centers. In others, only children treated for ROP are followed yearly.
- Follow up after laser or anti-VEGF treatment is individualized.
- Follow up of premature children (with or without ROP) is varying among centers and countries, mirroring the diverse states of health care system in different countries.
Prognosis
Stages 1 and 2 do not lead to blindness. However, they can progress to the more severe stages. Threshold disease is defined as disease that has a 50% likelihood of progressing to retinal detachment. Threshold disease is considered to be present when stage 3 ROP is present in either zone I or zone II, with at least five continuous or eight total clock hours of disease, and the presence of plus disease.[21] Progression to stage 4 (partial retinal detachment), or to stage 5 (total retinal detachment), will result in substantial or total loss of vision for the infant.
- Refractive errors including myopia (most common)
- Squint
- Amblyopia
- Retinal detachment, traction of the retina and blindness
- Glaucoma
- Impairments in visual acuity, contrast sensitivity, visual field, convergence, and accommodation[22]
Epidemiology
ROP prevalence varies, from 5 to 8% in developed countries with adequate neonatological facilities, to up to 30% in middle-income developing countries.[23]
There is increasing evidence that ROP and blindness due to ROP are now public health problems in the middle income countries of Latin America, Eastern Europe and the more advanced economies in South East Asia and the Middle east region. In these countries ROP is often the most common cause of blindness in children.[24][25] ROP is highly likely to become an increasing problem in India, China and other countries in Asia as these countries expand the provision of services for premature infants.
There is also evidence that the population of premature infants at risk of severe ROP varies depending on the level of neonatal intensive care being provided.[24] In countries with high development indices and very low neonatal mortality rates (e.g. North America, Western Europe), severe ROP is generally limited to extremely preterm infants i.e. those weighing less than 1 kg (2.2 lbs) at birth. At the other end of the development spectrum, countries with very low development indices and very high neonatal mortality rates (e.g. much of subSaharan Africa) ROP is rare as most premature babies do not have access to neonatal intensive care and so do not survive. Countries with moderate development indices are improving access to neonatal intensive care, and in these settings bigger, more mature babies are also at risk of severe ROP as neonatal care may be suboptimal. These findings have two main implications: firstly, much can be done in countries with moderate development indices to improve neonatal care, to reduce the risk of severe ROP in bigger babies and increase survival of extremely preterm infants, and secondly, in these settings bigger more mature babies need to be included in ROP programs and examined regularly so as to detect those babies developing ROP requiring treatment.
In 2012, the World Health Organization published data on rates of preterm birth and the number of premature babies born in different regions of the world.[26] This report contained three main findings:
- Premature birth has many different causes, and prevention is challenging,
- Prematurity is the most common cause of neonatal death in many countries, totaling as many as 1 million infants annually due to complications of preterm birth, and
- the number of preterm births is currently estimated to be 15 million, and increasing.
History
This disease was first described in a premature baby in 1942 as reported by Theodore L. Terry.[27] Between 1941 and 1953, over 12,000 babies worldwide were affected by it. Soul musician Stevie Wonder, actor Tom Sullivan, and jazz singer Diane Schuur are a few famous people who have the disease.
The first case of the epidemic was seen on St. Valentine's Day in 1941 when a premature baby in Boston was diagnosed. Cases were then seen all over the world and the cause was, at that point, unknown. By 1951 a clear link between incidence and affluence became clear: many cases were seen in developed countries with organized and well-funded health care. Two British scientists suggested that it was oxygen toxicity that caused the disease. Babies born prematurely in such affluent areas were treated in incubators which had artificially high levels of oxygen. Studies on rats made this cause seem more likely, but the link was eventually confirmed by a controversial study undertaken by American pediatricians. The study involved two groups of babies. Some[28] given the usual oxygen concentrations in their incubators, while the other group had "curtailed" oxygen levels. The latter group was shown to have a lower incidence of the disease. As a result, oxygen levels in incubators were lowered and consequently, the epidemic was halted. Each case of ROP avoided by withholding oxygen "may have cost some 16 deaths".[29]
References
- ↑ "Terry Syndrome". Stedman's Medical Dictionary. Lippincott Williams & Wilkins. 2006. Archived from the original on 4 March 2016. Retrieved 20 July 2022.
- ↑ "Retinopathy of prematurity: MedlinePlus Medical Encyclopedia". medlineplus.gov. Archived from the original on 8 July 2022. Retrieved 22 July 2022.
- ↑ Shastry, BS; Pendergast, SD; Hartzer, MK; Liu, X; Trese, MT (May 1997). "Identification of missense mutations in the Norrie disease gene associated with advanced retinopathy of prematurity". Archives of Ophthalmology. 115 (5): 651–5. doi:10.1001/archopht.1997.01100150653015. PMID 9152134.
- ↑ Dickinson, JL; Sale, MM; Passmore, A; FitzGerald, LM; Wheatley, CM; Burdon, KP; Craig, JE; Tengtrisorn, S; Carden, SM; Maclean, H; Mackey, DA (September–October 2006). "Mutations in the NDP gene: contribution to Norrie disease, familial exudative vitreoretinopathy and retinopathy of prematurity". Clinical & Experimental Ophthalmology. 34 (7): 682–8. doi:10.1111/j.1442-9071.2006.01314.x. PMID 16970763. S2CID 43683713.
- ↑ Shastry, Barkur S (1 January 2010). "Genetic susceptibility to advanced retinopathy of prematurity (ROP)". Journal of Biomedical Science. 17 (1): 69. doi:10.1186/1423-0127-17-69. PMC 2933676. PMID 20738858.
- ↑ Karna, P.; Muttineni, J.; Angell, L.; Karmaus, W. (2005). "Retinopathy of prematurity and risk factors: A prospective cohort study". BMC Pediatrics. 5 (1): 18. doi:10.1186/1471-2431-5-18. PMC 1175091. PMID 15985170.
- 1 2 Kumar, Vinay (2007). "Chapter 29: Eye, Retina and Vitreous, Retinal Vascular Disease". Robbins basic pathology (8th ed.). Philadelphia: Saunders/Elsevier. ISBN 978-1416029731.
- ↑ Guyton, Arthur; Hall, John (2006). "Chapter 17: Local and Humoral Control of Blood Flow by the Tissues". In Gruliow, Rebecca (ed.). Textbook of Medical Physiology (Book) (11th ed.). Philadelphia, Pennsylvania: Elsevier Inc. p. 200. ISBN 978-0-7216-0240-0.
- ↑ Stenson; BOOST ll Cooperative Groups (2013). "Oxygen Saturation and Outcomes in Preterm Infants" (PDF). New England Journal of Medicine. 368 (22): 2094–2104. doi:10.1056/nejmoa1302298. PMID 23642047.
- ↑ Committee for the Classification of Retinopathy of Prematurity (August 1984). "An international classification of retinopathy of prematurity". Arch. Ophthalmol. 102 (8): 1130–1134. doi:10.1001/archopht.1984.01040030908011. PMID 6547831.
- ↑ Committee for the Classification of Retinopathy of Prematurity (July 2005). "The International Classification of Retinopathy of Prematurity revisited". Arch. Ophthalmol. 123 (7): 991–999. doi:10.1001/archopht.123.7.991. PMID 16009843.
- ↑ Early Treatment for Retinopathy of Prematurity Cooperative Group (2003). "Revised indications for the treatment of retinopathy of prematurity: results of the early treatment for retinopathy of prematurity randomized trial". Arch. Ophthalmol. 121 (12): 1684–1696. doi:10.1001/archopht.121.12.1684. PMID 14662586.
- 1 2 3 4 Retinopathy of Prematurity at eMedicine
- ↑ Jefferies, AL; Canadian Paediatric Society; Fetus and Newborn Committee (1 December 2010). "Retinopathy of prematurity: Recommendations for screening". Paediatrics & Child Health. 15 (10): 667–0. doi:10.1093/pch/15.10.667. PMC 3006218. PMID 22131866. Archived from the original on 4 October 2017. Retrieved 9 March 2013.
- ↑ Dobson, V.; Quinn, G. E.; Summers, C. G.; Hardy, R. J.; Tung, B.; Good, W. V.; Good, W. V. (2011). "Grating Visual Acuity Results in the Early Treatment for Retinopathy of Prematurity Study". Archives of Ophthalmology. 129 (7): 840–846. doi:10.1001/archophthalmol.2011.143. PMC 4374597. PMID 21746974.
- ↑ Shah PK, Narendran V, Tawansy KA, Raghuram A, Narendran K (2007). "Intravitreal bevacizumab (Avastin) for post laser anterior segment ischemia in aggressive posterior retinopathy of prematurity". Indian Journal of Ophthalmology. 55 (1): 75–76. doi:10.4103/0301-4738.29505. PMID 17189897.
- ↑ Mintz-Hittner, HA; Kennedy, KA; Chuang, AZ; Beat-Rop Cooperative, Group (2011). "Efficacy of intravitreal bevacizumab for stage 3+ retinopathy of prematurity". The New England Journal of Medicine. 364 (7): 603–15. doi:10.1056/NEJMoa1007374. PMC 3119530. PMID 21323540.
- ↑ Sankar, Mari Jeeva; Sankar, Jhuma; Chandra, Parijat (8 January 2018). "Anti-vascular endothelial growth factor (VEGF) drugs for treatment of retinopathy of prematurity". The Cochrane Database of Systematic Reviews. 1: CD009734. doi:10.1002/14651858.CD009734.pub3. ISSN 1469-493X. PMC 6491066. PMID 29308602.
- ↑ Filippi L (2013). Archived 30 June 2016 at the Wayback Machine J Pediatr. 2013 Dec;163(6):1570-1577.e6
- ↑ Ristori C (2011). Archived 8 April 2016 at the Wayback Machine Invest Ophthalmol Vis Sci. 2011 Jan 5;52(1):155-70.
- ↑ Phelps, D.L. (2001). "Retinopathy of Prematurity: History, Classification, and Pathophysiology". NeoReviews. 2 (7): e153–e166. doi:10.1542/neo.2-7-e153.
- ↑ HEIDARY, Fatemeh; GHAREBAGHI, Reza (2016). "Outcomes of Retinopathy of Prematurity". Medical Hypothesis, Discovery and Innovation in Ophthalmology. 5 (4): 112–114. ISSN 2322-4436. PMC 5346299. PMID 28293657.
- ↑ Gergely, K.; Gerinec, A. (2010). "Retinopathy of prematurity—epidemics, incidence, prevalence, blindness". Bratislavske Lekarske Listy. 111 (9): 514–517. PMID 21180268.
- 1 2 Gilbert, C.; Fielder, A.; Gordillo, L.; Quinn, G.; Semiglia, R.; Visintin, P.; Zin, A.; International No-Rop, G. (2005). "Characteristics of Infants with Severe Retinopathy of Prematurity in Countries with Low, Moderate, and High Levels of Development: Implications for Screening Programs". Pediatrics. 115 (5): e518–e525. doi:10.1542/peds.2004-1180. PMID 15805336. Archived from the original on 3 May 2017. Retrieved 9 June 2013.
- ↑ Limburg, H.; Gilbert, C.; Hon, D. N.; Dung, N. C.; Hoang, T. H. (2012). "Prevalence and Causes of Blindness in Children in Vietnam". Ophthalmology. 119 (2): 355–361. doi:10.1016/j.ophtha.2011.07.037. PMID 22035577.
- ↑ "Born Too Soon: The Global Action Report on Preterm Birth". World Health Organization. 2012. Archived from the original on 20 January 2019. Retrieved 9 June 2013.
- ↑ Lambert, Scott R.; Lyons, Christopher J. (31 October 2016). Taylor and Hoyt's pediatric ophthalmology and strabismus. Lambert, Scott R.,, Lyons, Christopher J. (Fifth ed.). Edinburgh. ISBN 9780702066160. OCLC 960162637.
- ↑ Silverman, William A. (November 1980). Retrolental fibroplasia: a modern parable. Grune & Stratton. ISBN 9780808912644. Archived from the original on 27 June 2014. Retrieved 21 September 2013.
- ↑ Silverman, William A. (November 1980). Retrolental fibroplasia: a modern parable. Grune & Stratton. ISBN 9780808912644. Archived from the original on 27 June 2014. Retrieved 21 September 2013.
Chapter 8: "The Consequences of Oxygen Restriction"
External links
- Retinopathy of Prematurity Resource Guide from the National Eye Institute (NEI).
- Merck Manual entry on ROP Archived 28 February 2015 at the Wayback Machine
- World ROP Congress Archived 3 August 2021 at the Wayback Machine Archives of the International Conferences on ROP.
| Classification | |
|---|---|
| External resources |