Breast measurement
Breast measurement involves the measurement of the breasts for quantifying physical characteristics such as size, shape, and developmental state. A variety of different approaches have been employed for measuring the breasts.
Tanner staging

Tanner staging can be used to assess the developmental state of the breasts during puberty, from childhood (Tanner stage 1) to adulthood (Tanner stage 5).
Breast volume
Breast volume is a method of measuring the size of the breasts.[1][2] A variety of techniques have been used to measure breast volume, including water displacement, plaster casting, medical imaging (e.g., mammography, magnetic resonance imaging (MRI), ultrasound), and 3D scanning.[2][1] There is substantial measurement error with many breast volume measures, but MRI imaging appears to have among the lowest error and hence to be the most accurate measure.[1][2] However, 3D scanning might have the potential to become the new gold standard for clinical assessment.[3][4]
In a normative study of breast volumes in women using 3D scanning, breast volumes were median 515 mL, mean 650 mL, interquartile range 310 to 850 mL, and range ~50 to 3,100 mL.[5] In transgender women, breast volume measured with 3D scanning has been reported to reach a plateau of around 100 mL (but with an apparent range of up to 750 mL) after 3 to 4 years of hormone therapy.[6][7]
Breast circumference
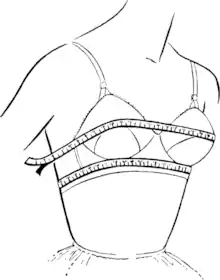
Breast circumference, also known as bust circumference, is a measurement of the circumference of the torso at the level of the breasts. It has been used as a measure of breast size in normal young women,[8] in women with pregnancy,[9][10] and in transgender women.[11][12][13][14] Breast circumference is generally measured using a flexible fabric tape measure, and is the circumference across the breasts over the nipples to the back. The breast–chest difference is breast circumference minus band or underbust circumference and is used in the determination of bra cup size.
Breast–chest difference
Breast–chest difference, also known as bust–band difference, is a measurement used for quantifying breast size. It is calculated as bust circumference minus the band or underbust circumference. Breast–chest difference has been used in the measurement of breast development in transgender women on feminizing hormone therapy.[15][6][16][17][13]
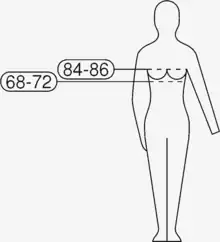
Bra size
Bra size, also bra cup size, is a measurement of the breasts for selecting bras, taking into account breast size and torso circumference. It is determined using the breast–chest difference, with 12–14 cm equating to an A cup, 14–16 cm a B cup, 16–18 cm a C cup, and 18–20 cm a D cup.
Breast hemicircumference
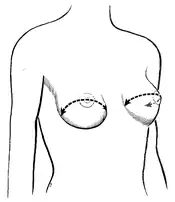
Breast hemicircumference, also sometimes referred to as breast width or as breast circumference (incorrectly), is an anthropometric measure of the breasts which has been used in studies to assess breast development and breast size, including in transgender women.[19][15][20][18][21][22][23] It is the medial horizontal length (measured with a flexible tape measure) from one side of the breast to the other side and running over the nipple.[20][18][21] A measurement of 7 inches is said to correspond to an A cup, 8 inches to a B cup, 9 inches to a C cup, and so on, with each further 1-cm increment or decrement corresponding to one cup size up or down.[21]
Breast unit
The breast unit is a measurement of the breasts in which the breasts are measured horizontally and vertically and then these values are multiplied to given an overall idea of breast size.[24][25][26] It was devised by Vincent J. Capraro and has been used in pediatric endocrinology to quantify breast development.[24][25][26] The method has been described as follows:[26]
At times it is desirable to know whether or not a girl's breasts are developing normally by observing their increasing size over a period of several months. In some cases it is also advantageous to determine whether or not differences in the sizes of the two breasts are of clinical significance. In order to more accurately measure breast size, one of us (V.J.C.) devised a technique for breast measurement. This technique may be used in following up the development of normal breasts as well as of breasts showing asymmetric development. With a centimeter tape measure, the breast is measured from 3 o'clock to 9 o'clock (Fig. 23-4, A) and from 12 o'clock to 6 o'clock (Fig. 23-4, B). These two measurements are multiplied, yielding a figure called the breast unit. Table 23-3 shows the typical spread of breast units in a normal adolescent.
The breast unit has also been used to quantify breast size in girls and women with complete androgen insensitivity syndrome (CAIS) and other individuals with disorders of sexual development.[27][28][29]
References
- Xi W, Perdanasari AT, Ong Y, Han S, Min P, Su W, Feng S, Pacchioni L, Zhang YX, Lazzeri D (December 2014). "Objective breast volume, shape and surface area assessment: a systematic review of breast measurement methods". Aesthetic Plast Surg. 38 (6): 1116–30. doi:10.1007/s00266-014-0412-5. PMID 25338712.
- Choppin SB, Wheat JS, Gee M, Goyal A (August 2016). "The accuracy of breast volume measurement methods: A systematic review". Breast. 28: 121–9. doi:10.1016/j.breast.2016.05.010. PMID 27288864.
- Killaars RC, Preuβ ML, de Vos NJ, van Berlo CC, Lobbes MB, van der Hulst RR, Piatkowski AA (November 2020). "Clinical Assessment of Breast Volume: Can 3D Imaging Be the Gold Standard?". Plast Reconstr Surg Glob Open. 8 (11): e3236. doi:10.1097/GOX.0000000000003236. PMC 7722547. PMID 33299702.
- Bai L, Lundström O, Johansson H, Meybodi F, Arver B, Sandelin K, Wickman M, Brandberg Y (2023). "Clinical assessment of breast symmetry and aesthetic outcome: can 3D imaging be the gold standard?". J Plast Surg Hand Surg. 57 (1–6): 145–152. doi:10.1080/2000656X.2021.2024553. PMID 35034560.
- Coltman CE, Steele JR, McGhee DE (November 2017). "Breast volume is affected by body mass index but not age". Ergonomics. 60 (11): 1576–1585. doi:10.1080/00140139.2017.1330968. PMID 28532249.
- de Blok CJ, Dijkman BA, Wiepjes CM, Staphorsius AS, Timmermans FW, Smit JM, Dreijerink KM, den Heijer M (January 2021). "Sustained Breast Development and Breast Anthropometric Changes in 3 Years of Gender-Affirming Hormone Treatment". J Clin Endocrinol Metab. 106 (2): e782–e790. doi:10.1210/clinem/dgaa841. PMID 33206172.
- Boogers, L., Infirri, S. S., Bouchareb, A., de Blok, C., Liberton, N., van Trotsenburg, P., ... & Hannema, S. (2022, September). The effect of timing of puberty suppression on breast development in trans girls; a cross-sectional study. Hormone Research in Paediatrics, 95(Suppl 2), 390–391. https://abstracts.eurospe.org/hrp/0095/hrp0095p1-379
- Kościński K, Makarewicz R, Bartoszewicz Z (April 2020). "Stereotypical and Actual Associations of Breast Size with Mating-Relevant Traits". Arch Sex Behav. 49 (3): 821–836. doi:10.1007/s10508-019-1464-z. PMC 7058577. PMID 31562583.
- Galbarczyk A (2011). "Unexpected changes in maternal breast size during pregnancy in relation to infant sex: an evolutionary interpretation". Am J Hum Biol. 23 (4): 560–2. doi:10.1002/ajhb.21177. PMID 21544894.
- Drąsutis, J. (2017). Krūtų morfologinių parametrų, kūno dydžio bei formos ir kraujo serumo prolaktino bei lipidų kitimai per nėštumą, daugialypės šių rodiklių sąsajos ir sveikatos rizikos morfologiniai žymenys (Doctoral dissertation, Vilniaus universitetas). https://epublications.vu.lt/object/elaba:23065971/
- Asscheman, H; Gooren, LJG; Megens, J (1989). "Physical Changes During Hormonal Treatment in Male-to-Female Transsexuals". In Billowitz, A (ed.). Proceedings of the XIth Harry Benjamin International Gender Dysphoria Association Symposium, Cleveland, Ohio, September 20–23, 1989. Palo Alto, California: Harry Benjamin International Gender Dysphoria Association. pp. 14–15.
- Kanhai RC, Hage JJ, Karim RB (June 2001). "Augmentation mammaplasty in male-to-female trans-sexuals: facts and figures from Amsterdam". Scand J Plast Reconstr Surg Hand Surg. 35 (2): 203–6. doi:10.1080/028443101300165354. PMID 11484531.
- Wierckx K, Van Caenegem E, Schreiner T, Haraldsen I, Fisher AD, Toye K, Kaufman JM, T'Sjoen G (August 2014). "Cross-sex hormone therapy in trans persons is safe and effective at short-time follow-up: results from the European network for the investigation of gender incongruence". J Sex Med. 11 (8): 1999–2011. doi:10.1111/jsm.12571. hdl:2158/1060207. PMID 24828032.
- de, Blok Christel; Klaver, Maartje; Nota, Nienke; Dekker, Marieke; den, Heijer Martin (13 May 2016). "Breast development in male-to-female transgender patients after one year cross-sex hormonal treatment". Endocrine Abstracts. doi:10.1530/endoabs.41.GP146. eISSN 1479-6848.
- Nolan BJ, Cheung AS (June 2021). "Relationship Between Serum Estradiol Concentrations and Clinical Outcomes in Transgender Individuals Undergoing Feminizing Hormone Therapy: A Narrative Review". Transgend Health. 6 (3): 125–131. doi:10.1089/trgh.2020.0077. PMC 8363983. PMID 34414268.
- de Blok CJ, Klaver M, Wiepjes CM, Nota NM, Heijboer AC, Fisher AD, Schreiner T, T'Sjoen G, den Heijer M (February 2018). "Breast Development in Transwomen After 1 Year of Cross-Sex Hormone Therapy: Results of a Prospective Multicenter Study". J Clin Endocrinol Metab. 103 (2): 532–538. doi:10.1210/jc.2017-01927. PMID 29165635.
- Meyer G, Mayer M, Mondorf A, Flügel AK, Herrmann E, Bojunga J (February 2020). "Safety and rapid efficacy of guideline-based gender-affirming hormone therapy: an analysis of 388 individuals diagnosed with gender dysphoria". Eur J Endocrinol. 182 (2): 149–156. doi:10.1530/EJE-19-0463. PMID 31751300.
- Meyer WJ, Webb A, Stuart CA, Finkelstein JW, Lawrence B, Walker PA (April 1986). "Physical and hormonal evaluation of transsexual patients: a longitudinal study". Arch Sex Behav. 15 (2): 121–38. doi:10.1007/BF01542220. PMID 3013122. S2CID 42786642.
- Wierckx K, Gooren L, T'Sjoen G (May 2014). "Clinical review: Breast development in trans women receiving cross-sex hormones". J Sex Med. 11 (5): 1240–7. doi:10.1111/jsm.12487. PMID 24618412.
- Meyer WJ, Finkelstein JW, Stuart CA, Webb A, Smith ER, Payer AF, Walker PA (August 1981). "Physical and hormonal evaluation of transsexual patients during hormonal therapy". Arch Sex Behav. 10 (4): 347–56. doi:10.1007/BF01565538. PMID 6794543. S2CID 6664163.
- Pechter EA (September 1998). "A new method for determining bra size and predicting postaugmentation breast size". Plast Reconstr Surg. 102 (4): 1259–65. doi:10.1097/00006534-199809040-00056. PMID 9734454.
- Pechter, Edward A. (2009). "Method for Determining Bra Size and Predicting Postaugmentation Breast Size". Breast Augmentation. Springer Berlin Heidelberg. pp. 77–83. doi:10.1007/978-3-540-78948-2_11.
- Pechter EA (May 2008). "An improved technique for determining bra size with applicability to breast surgery". Plast Reconstr Surg. 121 (5): 348e–350e. doi:10.1097/PRS.0b013e31816b1286. PMID 18453960.
- Capraro, Vincent J.; Dewhurst, Christopher J. (June 1975). "Breast Disorders in Childhood and Adolescence". Clinical Obstetrics and Gynecology. 18 (2): 25–50. doi:10.1097/00003081-197506000-00003. ISSN 0009-9201. PMID 1170054.
- Vincent J. Capraro (1977). "Breast problems in adolescence". In Ross Laboratories (ed.). Adolescent Gynecology: Report of the Seventh Ross Roundtable on Critical Approaches to Common Pediatric Problems in Collaboration with the Ambulatory Pediatric Association. Ross Laboratories. pp. 25–31. OCLC 29172030.
- John William Huffman; Sir Christopher John Dewhurst; Vincent J. Capraro (1981). "The Breast and its Disorders in Childhood and Adolescence". The Gynecology of Childhood and Adolescence (2 ed.). Saunders. pp. 542–559. ISBN 978-0-7216-4816-3. OCLC 1011891134.
- Wisniewski AB, Migeon CJ, Meyer-Bahlburg HF, Gearhart JP, Berkovitz GD, Brown TR, Money J (August 2000). "Complete androgen insensitivity syndrome: long-term medical, surgical, and psychosexual outcome". J Clin Endocrinol Metab. 85 (8): 2664–9. doi:10.1210/jcem.85.8.6742. PMID 10946863.
- Wisniewski AB, Migeon CJ, Gearhart JP, Rock JA, Berkovitz GD, Plotnick LP, Meyer-Bahlburg HF, Money J (2001). "Congenital micropenis: long-term medical, surgical and psychosexual follow-up of individuals raised male or female". Horm Res. 56 (1–2): 3–11. doi:10.1159/000048083. PMID 11815721.
- Migeon CJ, Wisniewski AB, Gearhart JP, Meyer-Bahlburg HF, Rock JA, Brown TR, Casella SJ, Maret A, Ngai KM, Money J, Berkovitz GD (September 2002). "Ambiguous genitalia with perineoscrotal hypospadias in 46,XY individuals: long-term medical, surgical, and psychosexual outcome". Pediatrics. 110 (3): e31. doi:10.1542/peds.110.3.e31. PMID 12205281.