NCR3
Natural cytotoxicity triggering receptor 3 is a protein that in humans is encoded by the NCR3 gene.[3][4][5] NCR3 has also been designated as CD337 (cluster of differentiation 337) and as NKp30. NCR3 belongs to the family of NCR membrane receptors together with NCR1 (NKp46) and NCR2 (NKp44).[6]
Identification
NKp30 receptor was first identified in 1999. According to Western blot analysis specific monoclonal antibodies reacted with 30kDa molecule, therefore was the protein named NKp30.[7]
Structure
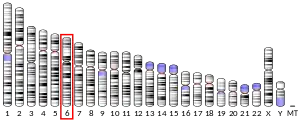
Gene for NKp30 is located in the MHC class III region of the human MHC locus and encodes 190 amino acid long type I transmembrane receptor which belongs to immunoglobulin super family (IgSF).[7][8] NKp30 has a mass of 30 kDa and includes one Ig-like extracellular domain which is 138 amino acids long, a 19 amino acid transmembrane (TM) domain and a 33 amino acid cytoplasmic tail.[7][6][9] The Ig-like domain consists of 2 antiparallel beta-sheets linked by a disulphide bond.[9][10] The extracellular domain contains two potential sites for N-linked glycosylation involved in ligand binding.[7] The TM domain contains a positivelly charged arginine residue, which associates with negatively charged aspartate in TM domain of ITAM adaptor molecules CD3ζ and FCεRIγ. This is a common feature of other NK cell activating receptors as well.[7][9][11] Accordingly the cytoplasmic tail lacks typical ITAM consensus sequence.
Splicing variants
We can find six different splicing variants on the cell surface. NKp30a, NKp30b and NKp30c encode molecules with extracellular V-type Ig domain. NKp30d, NKp30e and NKp30f encode extracellular C-type Ig domain. Splicing variants also differ in their cytosolic intracellular domains depending on the translation of variants of exon 4 (NKp30a,b or c).[6][8]
The distribution of splicing variants of NKp30 varies in tissues and results in different NK cell responses. NKp30a/b engagement stimulates the release of high amounts of IFN-γ, whereas activation of NKp30c induces IL-10 production and only small amounts of IFN-γ. First two are therefore considered as immunostimulatory isoforms which enhance Th1 immune response, while NKp30c mediates immunosuppressive signaling most likely because of reduced association with CD3ζ adaptor after cross-linking with ligand.[8]
Gastrointestinal stromal tumor patients who express NKp30c isoform have worse prognosis compared with patients expressing other isoforms, mainly as a consequence of NK cell immunosuppressive character.[8][12]
Expression
NCR3 is expressed mainly on cytoplasmic membrane of mature NK cells and functions as an activating receptor of NK cells. However it is also expressed on surface of CD8+ T cells, γδ T cells with Vδ1 TCR and ILC2.[6][11] The presence of IL-15 stimulates the expression of NKp30+ CD8+ T cells with anti-tumor activity.[6][13] Expression of NKp30 in γδ T cells is induced by IL-2 or IL-15.[6][14] After progesteron stimulation NKp30 can be found on the cytoplasmic membrane of endometrial epithelial cells as well.[8]
Function
NKp30 plays a major role in NK anti-tumor response and immunosurveillance, mainly by activating NK cell cytotoxicity and cytokine secretion.[6][15] Direct killing happens similarly to other natural cytotoxicity receptors (NCRs) such as NKp44 and NKp46.[7][16] NCR3 has a wide range of non-MHC ligands secreted or expressed by cancer or virus-infected cells, e.g. to heparan sulfate glycosaminoglycans (HS GAGs) and B7-H6.[6][9][17][15]
Heparan sulfate epitopes are in healthy tissue as well as on tumor cells, where HS GAGs are changed or differ in ligands (HMGB1, S100A8/A9) in contrast to healthy tissue. In addition, interaction of NCR with HS GAGs can facilitate binding to other cellular ligands. Thus via heparan sulfate epitopes NCRs can bind to the same ligands and exert similar reactions and at the same time also have their own unique interacting partners. It is also known that heparan sulfate epitopes lead to better signaling through growth factor receptors, NCRs could be thus evolved to recognize unusual HS GAGs on malignant cells as transformed cell patterns.[15]
Ligation of NKp30 and intracellular protein HLA-B-associated transcript 3 (BAT3) released by tumour cells to extracellular matrix results in NK and dendritic cell cross-talk.[6][17][10]
Human cytomegalovirus protein pp65 is another ligand of NKp30. The ligation leads to disruption of the interaction between NKp30 and CD3ζ and thus decreases the activation of NK cells and its cytotoxicity. This is a mechanism of HMCV to evade NK cell surveillance.[8][9][17]
Patients with primary Sjögren's syndrome express higher levels of NKp30+ NK cells (and its ligation with B7-H6 expressed in salivary glands) in comparison to healthy controls.[6]
NKp30 and dendritic cells
Immature dendritic cells can be lysed upon stimulation of NKp30 on NK cells.[8] Accordingly. patients with acute myeloid leukemia (AML), who often show downregulation in NKp30 expression, were incapable of effectively lysing both autologous and allogeneic immature dendritic cells. The ability of NK cells to kill immature dendritic cells may serve to check the quality of dendritic cell maturation process.[16] Interestingly at the same time immunostimulatory capacity of dendritic cells can be enhanced via interaction with NKp30 with ligands expressed on immature dendritic cells.[8] Upon such stimulation NK cells produce TNFα which is capable of inducing dendritic cell maturation.[16]
NCR3 during pregnancy
Uterine NK cells (uNK) are the most abundant lymphocyte population in uterus during pregnancy on the maternal-fetal interface. These cells are responsible for angiogenesis and vascular remodelling in trophoblast.[18][19] uNK cells express NKp30 and its ligands are expressed by trophoblast cells. Though these ligands have not yet been identified, this interaction has a potential to regulate fetal-maternal interface.[20][6] The uNK cells dominantly express the inhibitory NKp30c isoform.[21]
References
- ENSG00000236979, ENSG00000206430, ENSG00000237808, ENSG00000236315, ENSG00000223833, ENSG00000225211, ENSG00000204475 GRCh38: Ensembl release 89: ENSG00000237103, ENSG00000236979, ENSG00000206430, ENSG00000237808, ENSG00000236315, ENSG00000223833, ENSG00000225211, ENSG00000204475 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- Nalabolu SR, Shukla H, Nallur G, Parimoo S, Weissman SM (January 1996). "Genes in a 220-kb region spanning the TNF cluster in human MHC". Genomics. 31 (2): 215–22. doi:10.1006/geno.1996.0034. PMID 8824804.
- Sato M, Ohashi J, Tsuchiya N, Tadokoro K, Juji T, Hanaoka K, et al. (October 2001). "Identification of novel single nucleotide substitutions in the NKp30 gene expressed in human natural killer cells". Tissue Antigens. 58 (4): 255–8. doi:10.1034/j.1399-0039.2001.580406.x. PMID 11782277.
- "Entrez Gene: NCR3 natural cytotoxicity triggering receptor 3".
- Barrow AD, Martin CJ, Colonna M (2019-05-07). "The Natural Cytotoxicity Receptors in Health and Disease". Frontiers in Immunology. 10: 909. doi:10.3389/fimmu.2019.00909. PMC 6514059. PMID 31134055.
- Pende D, Parolini S, Pessino A, Sivori S, Augugliaro R, Morelli L, et al. (November 1999). "Identification and molecular characterization of NKp30, a novel triggering receptor involved in natural cytotoxicity mediated by human natural killer cells". The Journal of Experimental Medicine. 190 (10): 1505–16. doi:10.1084/jem.190.10.1505. PMC 2195691. PMID 10562324.
- Kruse PH, Matta J, Ugolini S, Vivier E (March 2014). "Natural cytotoxicity receptors and their ligands". Immunology and Cell Biology. 92 (3): 221–9. doi:10.1038/icb.2013.98. PMID 24366519. S2CID 38667462.
- Pinheiro PF, Justino GC, Marques MM (October 2020). "NKp30 - A prospective target for new cancer immunotherapy strategies". British Journal of Pharmacology. 177 (20): 4563–4580. doi:10.1111/bph.15222. PMC 7520444. PMID 32737988.
- Pazina T, Shemesh A, Brusilovsky M, Porgador A, Campbell KS (2017-03-30). "Regulation of the Functions of Natural Cytotoxicity Receptors by Interactions with Diverse Ligands and Alterations in Splice Variant Expression". Frontiers in Immunology. 8: 369. doi:10.3389/fimmu.2017.00369. PMC 5371597. PMID 28424697.
- Kaifu T, Escalière B, Gastinel LN, Vivier E, Baratin M (November 2011). "B7-H6/NKp30 interaction: a mechanism of alerting NK cells against tumors". Cellular and Molecular Life Sciences. 68 (21): 3531–9. doi:10.1007/s00018-011-0802-7. PMID 21877119. S2CID 22483622.
- Delahaye NF, Rusakiewicz S, Martins I, Ménard C, Roux S, Lyonnet L, et al. (June 2011). "Alternatively spliced NKp30 isoforms affect the prognosis of gastrointestinal stromal tumors". Nature Medicine. 17 (6): 700–7. doi:10.1038/nm.2366. PMID 21552268. S2CID 22671469.
- Correia MP, Stojanovic A, Bauer K, Juraeva D, Tykocinski LO, Lorenz HM, et al. (June 2018). "Distinct human circulating NKp30+FcεRIγ+CD8+ T cell population exhibiting high natural killer-like antitumor potential". Proceedings of the National Academy of Sciences of the United States of America. 115 (26): E5980–E5989. Bibcode:2018PNAS..115E5980C. doi:10.1073/pnas.1720564115. PMC 6042091. PMID 29895693.
- Correia DV, Fogli M, Hudspeth K, da Silva MG, Mavilio D, Silva-Santos B (July 2011). "Differentiation of human peripheral blood Vδ1+ T cells expressing the natural cytotoxicity receptor NKp30 for recognition of lymphoid leukemia cells". Blood. 118 (4): 992–1001. doi:10.1182/blood-2011-02-339135. hdl:2434/223196. PMID 21633088.
- Porgador A (February 2005). "Natural cytotoxicity receptors: pattern recognition and involvement of carbohydrates". TheScientificWorldJournal. 5: 151–4. doi:10.1100/tsw.2005.22. PMC 5936559. PMID 15759080.
- Moretta A, Bottino C, Vitale M, Pende D, Cantoni C, Mingari MC, et al. (April 2001). "Activating receptors and coreceptors involved in human natural killer cell-mediated cytolysis". Annual Review of Immunology. 19 (1): 197–223. doi:10.1146/annurev.immunol.19.1.197. PMID 11244035.
- Seidel E, Glasner A, Mandelboim O (December 2012). "Virus-mediated inhibition of natural cytotoxicity receptor recognition". Cellular and Molecular Life Sciences. 69 (23): 3911–20. doi:10.1007/s00018-012-1001-x. PMID 22547090. S2CID 16482529.
- Sojka DK, Yang L, Yokoyama WM (2019-05-01). "Uterine Natural Killer Cells". Frontiers in Immunology. 10: 960. doi:10.3389/fimmu.2019.00960. PMC 6504766. PMID 31118936.
- Moffett A, Colucci F (May 2014). "Uterine NK cells: active regulators at the maternal-fetal interface". The Journal of Clinical Investigation. 124 (5): 1872–9. doi:10.1172/JCI68107. PMC 4001528. PMID 24789879.
- Hanna J, Goldman-Wohl D, Hamani Y, Avraham I, Greenfield C, Natanson-Yaron S, et al. (September 2006). "Decidual NK cells regulate key developmental processes at the human fetal-maternal interface". Nature Medicine. 12 (9): 1065–74. doi:10.1038/nm1452. PMID 16892062. S2CID 19158471.
- Siewiera J, Gouilly J, Hocine HR, Cartron G, Levy C, Al-Daccak R, Jabrane-Ferrat N (December 2015). "Natural cytotoxicity receptor splice variants orchestrate the distinct functions of human natural killer cell subtypes". Nature Communications. 6 (1): 10183. Bibcode:2015NatCo...610183S. doi:10.1038/ncomms10183. PMC 4682172. PMID 26666685.
Further reading
- Djeu JY, Jiang K, Wei S (March 2002). "A view to a kill: signals triggering cytotoxicity". Clinical Cancer Research. 8 (3): 636–40. PMID 11895890.
- Holzinger I, de Baey A, Messer G, Kick G, Zwierzina H, Weiss EH (1995). "Cloning and genomic characterization of LST1: a new gene in the human TNF region". Immunogenetics. 42 (5): 315–22. doi:10.1007/BF00179392. PMID 7590964. S2CID 19916860.
- de Baey A, Fellerhoff B, Maier S, Martinozzi S, Weidle U, Weiss EH (November 1997). "Complex expression pattern of the TNF region gene LST1 through differential regulation, initiation, and alternative splicing". Genomics. 45 (3): 591–600. doi:10.1006/geno.1997.4963. PMID 9367684.
- Neville MJ, Campbell RD (April 1999). "A new member of the Ig superfamily and a V-ATPase G subunit are among the predicted products of novel genes close to the TNF locus in the human MHC". Journal of Immunology. 162 (8): 4745–54. doi:10.4049/jimmunol.162.8.4745. PMID 10202016. S2CID 46517924.
- Pende D, Parolini S, Pessino A, Sivori S, Augugliaro R, Morelli L, et al. (November 1999). "Identification and molecular characterization of NKp30, a novel triggering receptor involved in natural cytotoxicity mediated by human natural killer cells". The Journal of Experimental Medicine. 190 (10): 1505–16. doi:10.1084/jem.190.10.1505. PMC 2195691. PMID 10562324.
- Sivakamasundari R, Raghunathan A, Zhang CY, Chowdhury RR, Weissman SM (July 2000). "Expression and cellular localization of the protein encoded by the 1C7 gene: a recently described component of the MHC". Immunogenetics. 51 (8–9): 723–32. doi:10.1007/s002510000192. PMID 10941844. S2CID 27714493.
- Le Bouteiller P, Barakonyi A, Giustiniani J, Lenfant F, Marie-Cardine A, Aguerre-Girr M, et al. (December 2002). "Engagement of CD160 receptor by HLA-C is a triggering mechanism used by circulating natural killer (NK) cells to mediate cytotoxicity". Proceedings of the National Academy of Sciences of the United States of America. 99 (26): 16963–8. Bibcode:2002PNAS...9916963L. doi:10.1073/pnas.012681099. PMC 139252. PMID 12486241.
- Augugliaro R, Parolini S, Castriconi R, Marcenaro E, Cantoni C, Nanni M, et al. (May 2003). "Selective cross-talk among natural cytotoxicity receptors in human natural killer cells". European Journal of Immunology. 33 (5): 1235–41. doi:10.1002/eji.200323896. PMID 12731048. S2CID 10724743.
- Marcenaro E, Augugliaro R, Falco M, Castriconi R, Parolini S, Sivori S, et al. (December 2003). "CD59 is physically and functionally associated with natural cytotoxicity receptors and activates human NK cell-mediated cytotoxicity". European Journal of Immunology. 33 (12): 3367–76. doi:10.1002/eji.200324425. PMID 14635045. S2CID 40345630.
- Xie T, Rowen L, Aguado B, Ahearn ME, Madan A, Qin S, et al. (December 2003). "Analysis of the gene-dense major histocompatibility complex class III region and its comparison to mouse". Genome Research. 13 (12): 2621–36. doi:10.1101/gr.1736803. PMC 403804. PMID 14656967.
- Nowbakht P, Ionescu MC, Rohner A, Kalberer CP, Rossy E, Mori L, et al. (May 2005). "Ligands for natural killer cell-activating receptors are expressed upon the maturation of normal myelomonocytic cells but at low levels in acute myeloid leukemias". Blood. 105 (9): 3615–22. doi:10.1182/blood-2004-07-2585. PMID 15657183.
- Poggi A, Massaro AM, Negrini S, Contini P, Zocchi MR (March 2005). "Tumor-induced apoptosis of human IL-2-activated NK cells: role of natural cytotoxicity receptors". Journal of Immunology. 174 (5): 2653–60. doi:10.4049/jimmunol.174.5.2653. PMID 15728472.
- Vitale M, Della Chiesa M, Carlomagno S, Pende D, Aricò M, Moretta L, Moretta A (July 2005). "NK-dependent DC maturation is mediated by TNFalpha and IFNgamma released upon engagement of the NKp30 triggering receptor". Blood. 106 (2): 566–71. doi:10.1182/blood-2004-10-4035. PMID 15784725.
- Warren HS, Jones AL, Freeman C, Bettadapura J, Parish CR (July 2005). "Evidence that the cellular ligand for the human NK cell activation receptor NKp30 is not a heparan sulfate glycosaminoglycan". Journal of Immunology. 175 (1): 207–12. doi:10.4049/jimmunol.175.1.207. PMID 15972650.
- Joyce MG, Tran P, Zhuravleva MA, Jaw J, Colonna M, Sun PD (April 2011). "Crystal structure of human natural cytotoxicity receptor NKp30 and identification of its ligand binding site". Proceedings of the National Academy of Sciences of the United States of America. 108 (15): 6223–8. Bibcode:2011PNAS..108.6223J. doi:10.1073/pnas.1100622108. PMC 3076882. PMID 21444796.
External links
- NCR3+protein,+human at the U.S. National Library of Medicine Medical Subject Headings (MeSH)
- PDBe-KB provides an overview of all the structure information available in the PDB for Human Natural cytotoxicity triggering receptor 3 (NCR3)
This article incorporates text from the United States National Library of Medicine, which is in the public domain.