Coxsackie B virus
Coxsackie B is a group of six serotypes of coxsackievirus (CVB1-CVB6), a pathogenic enterovirus, that trigger illness ranging from gastrointestinal distress to full-fledged pericarditis and myocarditis (coxsackievirus-induced cardiomyopathy).[1][2]
| Coxsackie B virus | |
|---|---|
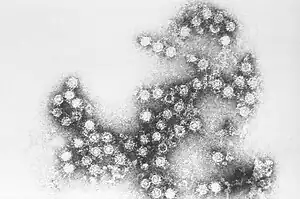 | |
| Coxsackie B4 virus | |
| Virus classification | |
| (unranked): | Virus |
| Realm: | Riboviria |
| Kingdom: | Orthornavirae |
| Phylum: | Pisuviricota |
| Class: | Pisoniviricetes |
| Order: | Picornavirales |
| Family: | Picornaviridae |
| Genus: | Enterovirus |
| Species: | Enterovirus B |
| Strain: | Coxsackie B virus |
The genome of Coxsackie B virus consists of approximately 7,400 base pairs.[3]
Geographic distribution
The various members of the Coxsackie B group were discovered almost entirely in the United States, appearing originally in Connecticut, Ohio, New York, and Kentucky, although a sixth member of the group has been found in the Philippines.[1] However, all six serotypes have a global distribution and are a relatively common cause of gastrointestinal upset. The name reflects the first isolation from Coxsackie, New York.
Transmission
Infections are most commonly spread by the oral-fecal route, emphasizing the importance of good hygiene, especially hand-washing.[2] Oral-oral and respiratory droplets can also be means of transmission.[4]
Epidemiology
Coxsackie B infections have been reported to account for nearly a quarter of all enterovirus infections.[5] Nearly half of all reported cases of Coxsackie B infections occur before the age of five.[5] For the CBV1 serotype, two-thirds of Centers for Disease Control and Prevention reported infections in the United States were for children under one year of age.[4]
Symptoms
Symptoms of infection with viruses in the Coxsackie B grouping include fever, headache, sore throat, gastrointestinal distress, extreme fatigue as well as chest and muscle pain. It can also lead to spasms in arms and legs. This presentation is known as pleurodynia or Bornholm disease in many areas. Patients with chest pain should see a doctor immediately—in some cases, viruses in the Coxsackie B family progress to myocarditis or pericarditis, which can result in permanent heart damage or death. Coxsackie B virus infection may also induce aseptic meningitis. As a group, they are the most common cause of unexpected sudden death, and may account for up to 50% of such cases.[6] The incubation period for the Coxsackie B viruses ranges from 2 to 6 days, and illness may last for up to 6 months in extreme cases, but may resolve as quickly as two days. Infection usually occurs between the months of May and June, but do not show symptoms until October in temperate Northern Hemisphere regions. People should ideally spend 1 month resting during the height of infection. Another cause of this virus is from a dirty wound from an accident.[1]
Diagnosis
Enterovirus infection is diagnosed mainly via serological tests such as ELISA[7] and from cell culture.[1] Because the same level and type of care is given regardless of type of Coxsackie B infection, it is mostly unnecessary for treatment purposes to diagnose which virus is causing the symptoms in question, though it may be epidemiologically useful.
Pathology
Coxsackie B infections usually do not cause serious disease, although for newborns in the first 1–2 weeks of life, Coxsackie B infections can easily be fatal.[2] The pancreas is a frequent target, which can cause pancreatitis.[2]
Coxsackie B3 (CB3) infections are the most common enterovirus cause of myocarditis and sudden cardiac death.[8] CB3 infection causes ion channel pathology in the heart, leading to ventricular arrhythmia.[8] Studies in mice suggest that CB3 enters cells by means of toll-like receptor 4.[9] Both CB3 and CB4 exploit cellular autophagy to promote replication.[9]
Diabetes
The B4 Coxsackie viruses (CB4) serotype was suggested to be a possible cause of diabetes mellitus type 1 (T1D).[10] An autoimmune response to Coxsackie virus B infection upon the islets of Langerhans may be a cause of T1D.[2]
Other research implicates strains B1, A4, A2 and A16 in the destruction of beta cells,[11][12] with some suggestion that strains B3 and B6 may have protective effects via immunological cross-protection.
Treatment and Prevention
As of 2008, there is no well-accepted treatment for the Coxsackie B group of viruses.[1] Palliative care is available, however, and patients with chest pain or stiffness of the neck should be examined for signs of cardiac or central nervous system involvement, respectively. Some measure of prevention can usually be achieved by basic sanitation on the part of food-service workers, though the viruses are highly contagious. Care should be taken in washing ones hands and in cleaning the body after swimming. In the event of Coxsackie-induced myocarditis or pericarditis, anti-inflammatories can be given to reduce damage to the heart muscle.
Persistent Coxsackie B virus (non-cytolytic infection)
Enteroviruses are usually only capable of acute infections that are rapidly cleared by the adaptive immune response.[13][14] However, mutations which enterovirus B serotypes such as coxsackievirus B and echovirus acquire in the host during the acute phase can transform these viruses into the non-cytolytic form (also known as non-cytopathic or defective enterovirus).[15] This form is a mutated quasispecies[13] of enterovirus which is capable of causing persistent infection in human tissues, and such infections have been found in the pancreas in type 1 diabetes,[16][17] in chronic myocarditis and dilated cardiomyopathy,[18][13][19] in valvular heart disease,[20] in myalgic encephalomyelitis,[21][22] and in Sjögren's syndrome.[23] In these persistent infections, viral RNA is present at very low levels, and some researchers believe it is just a fading remnant of the acute infection[14] although others scientists believe this persistent viral RNA may have pathological effects and cause disease.[24]
References
- Fields, Bernard N.; David M. Knipe; Robert M. Chanock; Joseph L. Melnick; Bernard Roizman; Robert E. Shope (1985). Fields Virology. New York: Raven Press. pp. 739–794. ISBN 978-0-88167-026-4.
- Tracy S, Gauntt C (2008). "Group B Coxsackievirus Virulence". Group B Coxsackieviruses. Current Topics in Microbiology and Immunology. Vol. 323. pp. 49–63. doi:10.1007/978-3-540-75546-3_3. ISBN 978-3-540-75545-6. PMID 18357765.
- Liu B, Li Z, Xiang F, Li F, Zheng Y, Wang G (2014). "The whole genome sequence of coxsackievirus B3 MKP strain leading to myocarditis and its molecular phylogenetic analysis". Virol. J. 11: 33. doi:10.1186/1743-422X-11-33. PMC 3996064. PMID 24555514.
- Wikswo ME, Khetsuriani N, Oberste MS (2009). "Increased activity of Coxsackievirus B1 strains associated with severe disease among young infants in the United States, 2007-2008". Clinical Infectious Diseases. 49 (5): e44–e51. doi:10.1086/605090. PMID 19622041.
- Moore M, Kaplan MH, Klein SW (1984). "Epidemiologic, clinical, and laboratory features of Coxsackie B1-B5 infections in the United States, 1970-79". Public Health Reports. 99 (5): 515–522. PMC 1424625. PMID 6091168.
- Maze, S. S.; Adolph, R. J. (February 1990). "Myocarditis: unresolved issues in diagnosis and treatment". Clinical Cardiology. 13 (2): 69–79. doi:10.1002/clc.4960130203. PMID 2407397.
- Bell, Eleanor J.; R.A. McCartney; Diane Basquill; A.K.R. Chaudhuri (1986). "Mu-Antibody capture elisa for the rapid diagnosis of enterovirus infections in patients with aseptic meningitis". Journal of Medical Virology. 19 (3): 213–7. doi:10.1002/jmv.1890190303. PMID 3016164. S2CID 32392085.
- Peischard S, Ho HT, Seebohm G (2019). "A Kidnapping Story: How Coxsackievirus B3 and Its Host Cell Interact". Cellular Physiology and Biochemistry. 53 (1): 121–140. doi:10.33594/000000125. PMID 31230428.
- Kemball CC, Alirezaei M, Whitton JL (2010). "Type B coxsackieviruses and their interactions with the innate and adaptive immune systems". Future Microbiology. 5 (9): 1329–1347. doi:10.2217/fmb.10.101. PMC 3045535. PMID 20860480.
- "Type of Enterovirus Linked to Type 1 Diabetes". November 2013.
- Laitinen, Olli H.; Honkanen, Hanna; Pakkanen, Outi; et al. (2014). "Coxsackievirus B1 Is Associated With Induction of β-Cell Autoimmunity That Portends Type 1 Diabetes". Diabetes. 63 (2): 446–455. doi:10.2337/db13-0619. PMID 23974921.
- Honkanen, Hanna; Oikarinen, Sami; Nurminen, Noora; et al. (2017). "Detection of enteroviruses in stools precedes islet autoimmunity by several months: possible evidence for slowly operating mechanisms in virus-induced autoimmunity". Diabetologia. 60 (3): 424–431. doi:10.1007/s00125-016-4177-z. PMID 28070615.
- Kim KS, Tracy S, Tapprich W, Bailey J, Lee CK, Kim K, Barry WH, Chapman NM (June 2005). "5'-Terminal deletions occur in coxsackievirus B3 during replication in murine hearts and cardiac myocyte cultures and correlate with encapsidation of negative-strand viral RNA". Journal of Virology. 79 (11): 7024–41. doi:10.1128/JVI.79.11.7024-7041.2005. PMC 1112132. PMID 15890942.
- Flynn CT, Kimura T, Frimpong-Boateng K, Harkins S, Whitton JL (December 2017). "Immunological and pathological consequences of coxsackievirus RNA persistence in the heart". Virology. 512: 104–112. doi:10.1016/j.virol.2017.09.017. PMC 5653433. PMID 28950225.
- Chapman, Nora M. (2022-05-12). "Persistent Enterovirus Infection: Little Deletions, Long Infections". Vaccines. 10 (5): 770. doi:10.3390/vaccines10050770. ISSN 2076-393X. PMC 9143164. PMID 35632526.
- Krogvold, Lars; Edwin, Bjørn; Buanes, Trond; Frisk, Gun; Skog, Oskar; Anagandula, Mahesh; Korsgren, Olle; Undlien, Dag; Eike, Morten C.; Richardson, Sarah J.; Leete, Pia; Morgan, Noel G.; Oikarinen, Sami; Oikarinen, Maarit; Laiho, Jutta E. (May 2015). "Detection of a low-grade enteroviral infection in the islets of langerhans of living patients newly diagnosed with type 1 diabetes". Diabetes. 64 (5): 1682–1687. doi:10.2337/db14-1370. ISSN 1939-327X. PMID 25422108.
- Chehadeh, W.; Kerr-Conte, J.; Pattou, F.; Alm, G.; Lefebvre, J.; Wattré, P.; Hober, D. (November 2000). "Persistent infection of human pancreatic islets by coxsackievirus B is associated with alpha interferon synthesis in beta cells". Journal of Virology. 74 (21): 10153–10164. doi:10.1128/jvi.74.21.10153-10164.2000. ISSN 0022-538X. PMID 11024144.
- Chapman, N. M.; Kim, K. S. (2008). "Persistent coxsackievirus infection: enterovirus persistence in chronic myocarditis and dilated cardiomyopathy". Current Topics in Microbiology and Immunology. 323: 275–292. doi:10.1007/978-3-540-75546-3_13. ISSN 0070-217X. PMID 18357775.
- "Persistent Coxsackievirus Infection: Enterovirus Persistence in Chronic Myocarditis and Dilated Cardiomyopathy". Group B coxsackieviruses. Tracy, S. (Steven), Oberste, M. Steven., Drescher, Kristen M. Berlin: Springer. 2008. pp. 275–286. ISBN 9783540755463. OCLC 233973571.
{{cite book}}: CS1 maint: others (link) - "Enterovirus replication in valvular tissue from patients with chronic rheumatic heart disease". academic.oup.com. Retrieved 2023-10-11.
- O'Neal, Adam J.; Hanson, Maureen R. (2021-06-18). "The Enterovirus Theory of Disease Etiology in Myalgic Encephalomyelitis/Chronic Fatigue Syndrome: A Critical Review". Frontiers in Medicine. 8: 688486. doi:10.3389/fmed.2021.688486. ISSN 2296-858X. PMC 8253308. PMID 34222292.
- Hanson, Maureen R. (2023-08-17). "The viral origin of myalgic encephalomyelitis/chronic fatigue syndrome". PLOS Pathogens. 19 (8): e1011523. doi:10.1371/journal.ppat.1011523. ISSN 1553-7366. PMID 37590180.
- Triantafyllopoulou, Antigoni; Tapinos, Nikos; Moutsopoulos, Haralampos M. (September 2004). "Evidence for coxsackievirus infection in primary Sjögren's syndrome". Arthritis and Rheumatism. 50 (9): 2897–2902. doi:10.1002/art.20463. ISSN 0004-3591. PMID 15457458.
- Zhang, Hongyi; Li, Yanwen; McClean, Dougal R; Richardson, Peter J; Latif, Najma; Dunn, Michael J; Archard, Leonard C; Florio, Richard; Sheppard, Mary; Morrison, Karen (2004). "Detection of enterovirus capsid protein VP1 in myocardium from cases of myocarditis or dilated cardiomyopathy by immunohistochemistry: Further evidence of enterovirus persistence in myocytes". Medical Microbiology and Immunology. 193 (2–3): 109–114. doi:10.1007/s00430-003-0208-8. PMID 14634804. S2CID 20457715.
- "Human coxsackievirus B1". NCBI Taxonomy Browser. 12071.
- "Human coxsackievirus B2". NCBI Taxonomy Browser. 82639.
- "Human coxsackievirus B3". NCBI Taxonomy Browser. 12072.
- "Human coxsackievirus B4". NCBI Taxonomy Browser. 12073.
- "Human coxsackievirus B5". NCBI Taxonomy Browser. 12074.