Disposition index
Disposition index (DI) is the product of insulin sensitivity times the amount of insulin secreted in response to blood glucose levels.[3][4] Insulin resistant individuals can maintain normal responses to blood glucose due to the fact that higher levels of insulin are secreted as long as the beta cells of the pancreas are able to increase their output of insulin to compensate for the insulin resistance. But the ratio of the incremental increase in plasma insulin associated with an incremental increase in plasma glucose (disposition index) provides a better measure of beta cell function than the plasma insulin response to a glucose challenge.[5] Loss of function of the beta cells, reducing their capacity to compensate for insulin resistance, results in a lower disposition index.[3]
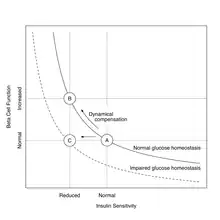
Disposition index is used as a measure of beta cell function and the ability of the body to dispose of a glucose load. Thus a lowering of disposition index predicts the conversion of insulin resistance to diabetes mellitus type 2.[6] Disposition index, but not insulin resistance, can predict type 2 diabetes in persons with normal blood glucose levels, but who do not have a family history (genetic predisposition) to type 2 diabetes.[7]
Disposition index can be increased by aerobic exercise, but only to the extent that insulin sensitivity is improved.[8]
References
- Cobelli, C; Toffolo, GM; Dalla Man, C; Campioni, M; Denti, P; Caumo, A; Butler, P; Rizza, R (July 2007). "Assessment of beta-cell function in humans, simultaneously with insulin sensitivity and hepatic extraction, from intravenous and oral glucose tests". American Journal of Physiology. Endocrinology and Metabolism. 293 (1): E1–E15. doi:10.1152/ajpendo.00421.2006. PMID 17341552.
- Hannon, TS; Kahn, SE; Utzschneider, KM; Buchanan, TA; Nadeau, KJ; Zeitler, PS; Ehrmann, DA; Arslanian, SA; Caprio, S; Edelstein, SL; Savage, PJ; Mather, KJ; RISE, Consortium (January 2018). "Review of methods for measuring β-cell function: Design considerations from the Restoring Insulin Secretion (RISE) Consortium". Diabetes, Obesity & Metabolism. 20 (1): 14–24. doi:10.1111/dom.13005. PMC 6095472. PMID 28493515.
- Bergman RN, Ader M, Huecking K, Van Citters G (2002). "Accurate assessment of beta-cell function: the hyperbolic correction". Diabetes. 51 (Supp 1): S212–S220. doi:10.2337/diabetes.51.2007.s212. PMID 11815482.
- Ferrannini, E; Mari, A (May 2004). "Beta cell function and its relation to insulin action in humans: a critical appraisal". Diabetologia. 47 (5): 943–56. doi:10.1007/s00125-004-1381-z. PMID 15105990.
- Defronzo RA (2009). "Banting Lecture. From the triumvirate to the ominous octet: a new paradigm for the treatment of type 2 diabetes mellitus". Diabetes. 58 (4): 773–795. doi:10.2337/db09-9028. PMC 2661582. PMID 19336687.
- Lorenzo C, Wagenknecht LE, Rewers MJ, Karter AJ, Bergman RN, Hanley AJ, Haffner SM (2011). "Disposition index, glucose effectiveness, and conversion to type 2 diabetes: the Insulin Resistance Atherosclerosis Study (IRAS)". Diabetes Care. 33 (9): 2098–2103. doi:10.2337/dc10-0165. PMC 2928371. PMID 20805282.
- Goldfine AB, Bouche C, Parker RA, Kim C, Kerivan A, Soeldner JS, Martin BC, Warram JH, Kahn CR (2003). "Insulin resistance is a poor predictor of type 2 diabetes in individuals with no family history of disease". Proceedings of the National Academy of Sciences of the United States of America. 100 (5): 2724–2729. Bibcode:2003PNAS..100.2724G. doi:10.1073/pnas.0438009100. PMC 151408. PMID 12591951.
- Solomon TP, Malin SK, Karstoft K, Kashyap SR, Haus JM, Kirwan JP (2013). "Pancreatic β-cell function is a stronger predictor of changes in glycemic control after an aerobic exercise intervention than insulin sensitivity". The Journal of Clinical Endocrinology and Metabolism. 98 (10): 4176–4186. doi:10.1210/jc.2013-2232. PMC 3790622. PMID 23966244.