Free fatty acid receptor 2
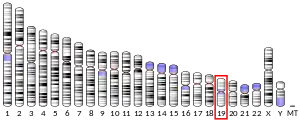
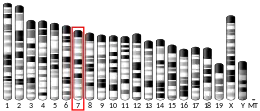
Free fatty acid receptor 2 (FFAR2), also termed G-protein coupled receptor 43 (GPR43), is a rhodopsin-like G-protein coupled receptor (also termed GPR or GPCR). It is coded (i.e., its synthesis is directed) by the FFAR2 gene.[5] (FFAR2 and Ffar2 are used respectively to designate the human and animal genes for FFAR2.) In humans, the FFAR2 gene is located on the long (i.e., "q") arm of chromosome 19 at position 13.12 (location notated as 19q13.12).[6] Like other GPCRs, FFAR2s reside on the surface membrane of cells and when bond to one of their activating ligands regulate the function of their parent cells.[7] FFAR2 is a member of a small family of structurally and functionally related GPRs termed free fatty acid receptors (FFARs). This family includes three other receptors which, like FFAR2, are activated by certain fatty acids: FFAR1 (also termed GPR40), FFAR3 (GPR41), and FFAR4 (GPR120). FFAR2 and FFAR3 are activated by short-chain fatty acids[8] whereas FFAR1 and FFAR4 are activated by long-chain fatty acids.[9]
Short-chain fatty acids (i.e., SCFAs) are made by intestinal bacteria (intestinal and intestine are used here to mean the small intestine plus the large intestine's longest portion, the colon). These SCFAs are excreted from the bacteria, enter the hosts tissues, and stimulate cells in these tissues. This stimulation regulates many normal body functions but may result in the inhibition or promotion of various diseases and disorders.[10] The types of bacteria in the intestines can be modified to increase the number of bacteria that make SCFAs by using foods that stimulate the growth of these bacteria (i.e., prebiotics), preparations of SCFA-producing bacteria (i.e., probiotics), or both methods (i.e., synbiotics).[11] Individuals with diseases or disorders that are associated with low levels of the SCFA-producing intestinal bacteria may show improvements in their conditions when treated with prebiotics, probiotics, or synbiotics while individuals with diseases or disorders associated with high levels of SCFAs may show improvements in their conditions when treated with methods, e.g., antibiotics, that reduce the intestinal levels of these bacteria.[10][9] It is now known that FFAR2 is activated by SCFAs and therefore may function not only in regulating normal body functions but also in inhibiting or promoting many diseases and disorders. Consequently, drugs are being tested for their ability to act more usefully, potently, and effectively than SCFAs to stimulate FFAR2 for treating conditions that appear inhibited by SCFAs; drugs are also being tested for their ability to inhibit FFAR2 and treat conditions that appear promoted by SCFAs.[12]
Studies have suggested that SCFA-activated FFAR2 regulates blood insulin and glucose levels, inflammation, the development of fat tissues, blood levels of fatty acids, the growth of certain cancerous and non-cancerous cells, and the infectiveness and severity of certain bacteria and viruses. As a result of these actions, FFAR2 may promote or inhibit the development and/or progression of diabetes, inflammatory reactions, obesity, ketoacidosis (i.e., life-threatening increases in blood acidity due to diabetes, starvation, excessive alcohol intake, certain medications, or certain toxins), some types of cancer, maturation of microglia (i.e., immune) cells in the brain and spinal cord,[9] certain neurological diseases,[13][14] and certain bacterial and viral infections.[15][16] Here, we review studies on the functions of FFAR2 in health as well as these diseases and disorders.
Activators and inhibitors of FFAR2
FFAR2 and FFR3 are activated primarily by short-chain fatty acids (SCFAs) that are 2 to 6 carbons in length (see length of fatty acids). In humans, acetic acid, which has 2 carbon atoms, is a strong activator of FFAR2 but very weak activator of FFAR3;[17] propionic and butyric acids, which have 3 and 4 carbons, respectively, are strong activators of both FFAR2 and FFAR3;[18] pentanoic acid, which has 5 carbon atoms, is a weak activator of FFAR2 but strong activator of FFAR3;[19] and hexanoic acid, which has 6 carbon atoms, is a weak activator of FFAR3[9] but its effect on FFAR2 has not been reported.[17] More recently, the ketone body fatty acid, acetoacetic acid, while not classified as a SCFA, has been shown to activate FFAR2 with a potency similar to acetic and propionic acids.[20]
Many drugs have been developed that bind to and regulate FFAR2's activity. 1) MOMBA, Sorbate,[18] and Compound 1[21] are orthostatic agonists, i.e., they bind to the same site as SCFAs to activate FFAR2. 2) Compound 58 and AZ1729 are positive allosteric agonists, i.e., they bind to FFAR2 at a site different than the orthostatic binding site and do not by themselves alter FFAR2 activity but enhance the ability of SCFAs and other FFAR2 orthostatic agonists to activate FFAR2.[21] 3) CATPB and BTI-A-404 are reverse agonists, i.e., they bind to the same site as SCFAs but induce a response opposite to that induced by SCFAs.[22]4) 4-CMTB[18] and TUG-1375[12][23] are classified as FFAR2 agonists but studies are needed to define their binding sites on FFAR2. And 5) GLPG0974 is an allosteric antagonist, i.e., it inhibits human FFAR2 by binding to a site different than the SCFAs' binding site. GLPGO908 does not bind to or inhibit rodent FFAR2[23] but nonetheless GLPG0974 does have effects in rodents. Off-target actions such as these need to be but often are not considered in studies on the actions of SCFAs and FFAR2 drugs.[18] Furthermore, SCFAs have many actions that do not involve FFAR2, e.g., they activate FFAR3, GPR109A (now termed hydroxycarboxylic acid receptor 2 or HCA2), and two other GPRs, Olfr78 and Olfr558.[10] Most of the studies reported here include experiments in which the actions of SCFAs and FFAR2-regulating drugs in cells and animals are further tested in the cells and animals that have been made to express relatively little or no FFAR2 using gene knockdown or gene knockout methods, respectively. The effects of SCFAs and the drugs should be reduced or absent in cells and animals that under-express or lack FFAR2.
Cells and tissues expressing FFAR2
Studies have detected FFAR2 protein and/or its messenger RNA (an indicator of FFAR2 protein expression) in the following cell types, cell lines, and tissues: 1) human and rodent enteroendocrine K cells, i.e., cells located in the epithelium of the small intestine; 2) human and rodent enteroendocrine L cells, i.e., cells located in the epithelium of the small intestine and colon;[24][25][26][27] 3) human and rodent fat tissue and/or cultured fat cells;[24] 4) cells in human and rodent pancreatic islets (these islets contain the beta cells and alpha cells that synthesize and secrete insulin and glucagon, respectively, into the blood);[28] 5) cells in and/or derived from cells in the human or mouse spleen, lymph nodes, bone marrow, and blood (e.g., monocytes, lymphocytes,[26] and neutrophils[29]); 6) mouse[30] and, based on indirect studies, human[31] dendritic cells; 7) cells in or derived from cells in human and/or rodent kidneys, hearts, brains (e.g., hypothalamus), fetal membranes, and placentas;[26][32] 8) cells in the taste buds' lingual papillae of human tongues;[26] 9) mouse renal arteries, aortas, and iliac arteries;[33] 10) various human cell lines including SW480, SW620, HT-29, and T84 colon cancer cells, NCI-H716 colon cancer cells that have a lymphoblast morphology, Caco-2 colorectal cancer cells, Hutu-80 duodenal cancer cells, SW872 liposarcoma cells, MDA-MB-231, MDA-MB-436, and MCF7 breast cancer cells, Huh7 and JHH-4 liver cancer cells, THP-1 acute myeloid leukemia cells, U937 acute promyelocytic leukemia cells, and K562 myelogenous leukemia cells;[26] and 11) the various mouse and rat cell lines discussed below. FFAR2 is also expressed in a wide range of tissues in other animals such as cows, pigs, sheep, cats, and dogs.[26]
Formation of SCFAs
The oral administration of glucose elicits a much greater rise in blood insulin levels and a much lower rise in blood glucose levels than those elicited by intravenous glucose infusions. This difference, termed the incretin effect, is due to the activation of FFAR2-bearing intestinal cells by the SCFAs that intestinal bacteria excrete.[34] The microbiotas inside the small intestine and colon of animals and humans consist of a wide range of microorganisms and viruses. The microorganisms ingest the food their hosts consume including soluble dietary fibers, e.g., resistant starch, xanthan gum, and inulin, all three of which are resistant to the hosts' digestive enzymes.[35] Certain microorganisms (e.g., anaerobic bacteria[36]), ferment[24] these dietary fibers to form and then excrete SCFAs (primarily acetic, propionic, and butyric acids[37]).[38] The relative levels of these three SCFAs in the intestines of humans are about 60:20:20, respectively.[15] Intestinal SCFAs activate FFAR2-bearing cells in the nearby intestinal walls and also enter the blood circulation to activate FFAR2-bearing cells in distant tissues.[10] SCFAs may also be made and released by the bacteria and/or host cells in tissue that contain bacterial infections.[15]
FFAR2 functions and actions
Type 2 diabetes
The SCFAs excreted by the soluble dietary fiber-consuming bacteria in the intestine activate FFAR2 on nearby intestinal L-cells. This stimules these cells to secrete GLP-1 (i.e., glucagon-like peptide-1) and PYY (i.e., peptide YY) into the blood. GLP-1 stimulates pancreatic beta cells to secrete insulin into the blood and inhibits pancreatic alpha cells from secreting glucagon into the blood. Since insulin causes cells to take up blood glucose and glucagon causes the liver to release glucose into the blood, FFAR2 activation of L cells lowers blood glucose levels. In addition, PYY[39] and GLP-1[11] reduce appetite and food consumption. The excreted SCFAs also activate FFAR2 on nearby intestinal K cells to simulate their secretion of GIP (i.e., glucose-dependent insulinotropic polypeptide). GIP stimulates insulin secretion but, perhaps paradoxically, also stimulates glucagon secretion; however, the net effect of GIP is to reduce blood glucose levels. GIP also slows gastric motility.[17][40] In addition, both GLP-1 and GIP protect pancreatic beta cells from dying by apoptosis (see programmed cell death).[17] The SCFAs excreted by the gut microorganisms also pass through the intestinal epithelium to enter the blood stream[37] and activate FFAR2 on cells located in distant tissues such as pancreas beta cells[39] and adipose tissue fat cells.[37]
Individuals with type 2 diabetes, particularly in advanced cases, have nearly completely lost the incretin effect.[41] A study treated non-diabetic, healthy men with the GLP-1 receptor antagonist (i.e., blocker of receptor activation) exendin(9-39)NH2a (also termed avexitide[42]), the GIP receptor antagonist GIP(3-30)NH2,[43] or both antagonists and challenged them with an oral glucose tolerance test. Men treated with either agent responded to the tolerance test with modest decreases in blood insulin levels and modest increases in blood glucose levels. However, men treated with both antagonists responded with very low insulin and very high glucose blood levels: their responses were similar to those in individuals with type 2 diabetes.[41][44] This study shows that 1) the stimulation of the FFAR2 on K and L cells by SCFAs underlies the differences between oral and intravenous glucose challenges defined by the incretin effect and 2) FFAR2 functions to regulate blood insulin and glucose levels. This does not prove that type 2 diabetes is a FFAR2-incretin disease: post-feeding secretion of the incretins (i.e.,GLP-1 and GIP) is impaired in type 2 diabetes, but the impairment appears to result primarily from decreases in the responsiveness of pancreas alpha cells to GLP-1. This conclusion is supported by studies showing that type 2 diabetic individuals who are treated with large amounts of GLP-1 and challenged with intravenous glucose show changes in blood insulin and glucose levels that are similar to those in non-diabetic individuals.[41] Indeed, GLP-1 agonists, e.g., Dulaglutide,[45] and a first-in-kind GLP-1 and GIP agonist, Tirzepatide,[46] are used to treat type 2 diabetes.
Type 1 diabetes
Ffar2 gene knockout mice (i.e., mice that have had their Ffar2 genes removed or inactivated) have decreased pancreatic beta cell masses at birth and throughout adulthood but do not develop diabetes.[47] However, they do develop defective insulin secretion, glucose intolerance (a prediabetic condition in humans manifested by elevated blood glucose levels),[48] and obesity.[26] This mouse model has some but not all of the features found in human type 1 diabetes. In particular, human type 1 diabetes is at least partly a genetically predisposed autoimmune disease in which an individual's immune system causes inflammation in their pancreatic islets that injures their beta, alpha, and other cells.[17] Non-obese Diabetic mice, i.e., NOD mice, may be a more appropriate model of the human disease. These mice are genetically predisposed to develop tissue-damaging inflammation in their pancreatic islets, insulin insufficiency, and overt diabetes. NOD mice fed a HAMSA or HAMSB diet (i.e., prebiotic diets which cause high intestinal levels of acetic acid or butyric acid, respectively), were partially protected and mice fed a combination of the two diets were fully protected from developing diabetes. Notably, Ffar2 gene knockout NOD mice had far more pancreatic islet inflammation and far less protection from becoming diabetic by either of these diets.[49] Finally, a study of children with pre-type 1 diabetes (base on their having antibodies against multiple pancreatic islet antigens) found that children who had low levels of SCFA-producing intestinal bacteria had a higher risk of progressing to type 1 diabetes than those with higher intestinal levels of these bacteria.[50] These results suggest that the activation of FFAR2 by intestinal SCFAs suppresses the development of type 1 diabetes in mice and humans and may do so by reducing the inflammation with injures pancreatic islet cells.[9][49][50][51]
Inflammation
FFAR2 is expressed in various cells involved in the development of inflammatory responses such as neutrophils, monocytes, macrophages, dendritic cells, regulatory T cells, and T helper cells. FFAR2 often appears to be involved in suppressing these cells' pro-inflammatory actions and thereby the development of inflammation. For example: 1) compared to control mice, Ffar2 gene knockout mice developed more severe and unresolving inflammation in colitis, arthritis, peritonitis, and asthma models of inflammation; 2) germ-free mice, which lack intestinal SCFAs, likewise had severer disease in these colitis, arthritis, and asthma models; 3) in a dextran sulphate sodium-induced model of colitis, Ffar2 gene knockout mice developed more severe disease than control mice;[9][52] 4) two studies found that normal mice but not Ffar2 gene knockout mice fed a prebiotic diet that produces higher intestinal levels of SCFAs were protected from developing allergic responses to food;[9][53] 5) the latter study also showed that the prebiotic diet was fully protective in Ffar3 gene knockout mice[53] (allergic responses are a subtype of the inflammatory reactions[54]); and 6) studies in mice and humans suggest that FFAR2 is involved in suppressing the pancreatic islet inflammation underlying the development of type 1 diabetes (see previous section). Other studies, however, have reported that FFAR2 promotes inflammation.[55] Two studies found that FFAR2 gene knockdown mice had less severe disease in a dextran sulphate sodium-induce colitis model compared to control mice.[9] And, another study reported that the level of FFAR2 messenger RNA in circulating blood monocytes was elevated in humans with gout compared to those who did not have gout and rose further during flare-ups of their disease; the study suggested that FFAR2 is involved in triggering gout flare-ups.[56] Notably, a study based on the premise that FFAR2 promotes inflammation examined the effect of GLPG0974, a potent allosteric antagonist inhibitor of FFAR2,[18][57] on patients with the inflammatory disease ulcerative colitis. The study progressed through phase I and II clinical studies that found the drug to be safe (i.e., non-toxic) but ineffective in reducing mild to moderate ulcerative colitis (further development of GLPG609 was terminated[58]).[18] While most studies suggest that FFAR2 suppresses human and mouse inflammation, further studies are needed to determine if and why FFAR2 promotes some types of inflammation.[9][26][55]
Angiogenesis and obesity
Studies have disagreed about the effects of FFAR2 on adipogenesis (i.e., formation of fat cells and fat tissue from precursor cells) as well as on the development of obesity.[9][24] The inconsistencies reported by different research groups need to be resolved through further research in order to develop a clear picture of the actions that FFAR2 has on adipogenesis and obesity.[24][55]
Lipolysis
Numerous studies have shown that SCFAs and FFAR2-activating drugs inhibit the lipolysis (i.e., enzymatic hydrolytic breakdown of cellular triglycerides into their component fatty acids and glycerol) in mice and their cultured fat cells.[24] For example: acetic and propionic acids inhibited lipolysis in mice (as defined by reducing their fatty acid blood levels) as well as their isolated cultured fat cells but did not do so in Ffar2 gene knockout mice or their isolated fat cells.[24][59] There have been very few studies on FFAR2 and lipolysis in humans. Two studies reported that acetic acid suppressed fatty acid blood levels in humans but did not determine if this effect involved FFAR2.[59][60][61] Note that in a mouse model of severe stress, i.e., starvation, FFAR2 activation stimulated lipolysis (see next section on Ketogenesis and ketoacidosis).[20] FFAR2 appears to have very different effects on lipolysis in mice depending on their energy conditions and nutritional status.[9] While SCFAs and FFAR2 have been suggested to stimulate lipolysis in humans on low glucose diets (study described in section on Ketogenesis and ketoacidosis), the role of FFAR2 in this stimulation is unclear and requires further study.[62]
Ketogenesis and ketoacidosis
Ketogenesis is a condition in which the liver releases ketone bodies, i.e., acetoacetic acid, beta-hydroxybutyric acid, and acetone, into the blood. This occurs when blood glucose levels are moderately low such as during sleep, fasting, dieting,[63] pregnancy, and the first 28 days after birth (i.e., the neonatal period); this form of ketogenesis is associated with modest elevations in the blood levels of the ketone bodies and, due to their increased release from adipose tissue, fatty acids.[62] The circulating ketone bodies and fatty acids serve as nutrients to sustain the functioning of critical organs such as muscle, heart, kidney and brain when blood glucose levels are too low to do so.[62] During serious stress conditions such as diabetic ketoacidosis and non-diabetic ketoacidosis due to excessive alcohol intake, medications, toxins, or starvation (see ketogenesis sections on each of these conditions), blood glucose levels are very low, blood ketone bodies and fatty acid levels are very high, and (due to the high blood levels of the ketone bodies and fatty acids) the blood is extremely acidic. This condition, a form of acidosis termed ketoacidosis, is life-threatening.[22] In addition to serving as a tissue nutrient and blood acidifier, one of the circulating ketone bodies appears to have another function: acetoacetic acid activates FFAR2. In a mouse model of starvation-induced ketogenesis: 1) the plasma concentration of acetoacetate was markedly increased in wild-type as well as Ffar2 gene knockout mice while at the same time plasma levels of acetic, propionic, and butyric acids were, as a consequence of starvation, far below those that would activate FFAR2; 2) plasma free fatty acid levels were elevated in wild type but not Ffar2 gene knockout mice; 3) fat tissue weight was significantly higher in Ffar2 gene knockout than wild-type mice; and 4) the lean body masses in the two groups of mice were comparable.[20] These results suggest that in mice the acetoacetic acid-induced activation of FFAR2 on fat cells stimulates lipolysis and thereby the rises in plasma fatty acid levels that occur in mild and severe ketoacidosis. Thus, FFAR2 appears to have a physiological role in mild but a pathological role in severe ketogenesis in mice.[20][62] The acetoacetic acid-FFAR2-lipolysis linkage may occur in humans. Ketogenic diets i.e., low-carbohydrate diets, have been used to treat various neurological diseases. Individuals on these diets develop a mild form of ketogenesis consisting of moderately high blood levels of the ketone bodies and fatty acids. The increased fatty acid levels of individuals on these diets may be due to the stimulation of lipolysis by acetoacetic acid-induced activation of FFAR2 on their fat cells. High blood levels of beta-hydroxybutyric acid may activate hydroxycarboxylic acid receptor 2 on fat cells to similarly cause elevated fatty acid blood levels. Further studies are needed to support this role for FFAR2 in elevating fatty acid blood levels in humans on the ketogenic diet.[62]
Blood pressure regulation and vascular disease
The infusion of a FFAR2-activating SCFA, i.e. acetic, propionic, or butyric acid, into mice causes short-term falls in their blood pressure.[64] Similarly, patients undergoing hemodialysis that uses a hemodialysis solution containing acetic acid have an increased risk of becoming hypotensive compared to patients dialyzed with an acetic acid-free solution.[65] Furthermore, FFAR2 gene knockout mice developed perivascular fibrosis (which is an indicator of blood vessel disease[66]), higher end-diastolic blood pressures, and higher pulse pressures.[67] Finally, in the angiotensin II–infusion model of hypertension, mice had reduced levels of FFAR2 in their kidney tissues compared to control mice[64] and a study in humans reported that the levels of FFAR2 in the circulating white blood cells of hypertensive individuals was significantly lower than that in individuals with normal blood pressures.[68] These findings suggest that FFAR2 functions to reduce blood pressure as well as hypertension induced vascular disease in mice and humans and support further studies to examine these relationships.[64]
Cancer
Preliminary studies suggest that FFAR2 may be involved in some types of cancer.[69] 1) One study found that FFAR2 levels were elevated in human stomach and colorectal cancers although another study reported that FFAR2 levels were markedly deceased in human colorectal cancer. These results suggest that FFAR2 may promote the development and/or progression of human stomach cancer but its impact on human colorectal cancer requires further study.[22] 2) In a dextran sulfate sodium-induced model of inflammation-associated colon cancer, FFAR2 knockdown mice developed larger and more tumors than control mice.[70] This study suggests that FFAR2 inhibits the development and/or progression of inflammation-associated colon carcinoma in mice; its role in human inflammation-associated colorectal cancer (e.g., colorectal cancer developing in ulcerative colitis) has not been clarified.[9] 3) Compared to their normal lung tissues, the lung cancer tissues of 42 patients had lower levels of FFAR2 but not FFAR1, FFAR3, or FFAR4.[71] 4) Butyric acid inhibited the proliferation of and triggered apoptosis in cultured human A549 lung cancer cells;[72] further studies in A549 as well as H1299 human lung cancer cells found that propionic acid inhibited their stimulated migration, invasiveness, and colony growth in cell culture assays but did not do so in FFAR2 gene knockout A549 or H1299 cells.[71] These results suggest that FFAR2 may inhibit the development and/or progression of human lung cancer.[71][72] (Studies have also reported that SCFAs inhibit the proliferation and caused apoptosis in cultured human breast cancer MCF-7[73] and human bladder cancer NaB cells[74] but neither study determined if their actions involved FFAR2.) Further studies are needed to confirm and broaden these preliminary findings and extend them to other types of cancer.[9][69]
Nervous system
Microglia are the resident immune cells of the central nervous system (i.e., brain and spinal cord). They are key contributors to the development and maintenance of neural tissues[75] and mediate inflammatory responses to, e.g., bacterial invasion as well as the pathological inflammations which underlie many neurological diseases.[13][14] Studies have reported that compared to control mice, germ-free mice (which lack SCFAs in their gastrointestinal tracts) have increased levels of immature microglia throughout their brains; SCFA supplementation normalized the microglial cell maturity. Furthermore, Ffar2 gene knockout mice likewise had increased levels of immature microglia throughout their brains. These studies suggest that FFAR2 is required for the maturation, and therefore functionality, of the microglia in mice.[9][10] Since mouse microglial cells do not express FFAR2, the FFAR2-bearing cells responsible for the maturation and thereby functionality of the mouse's microglia are unclear.[9]
Studies have suggested that promoting the intestinal microbiota's production of SCFAs may suppress the development and/or progression of various human neurological diseases, particularly Parkinson’s disease, Alzheimer's disease, neuromyelitis optica, and multiple sclerosis. This linkage is thought to involve at least in part SCFA-induced suppression of the inflammation associated with these diseases.[13][76] With somewhat less evidence, other studies have suggested that SCFRs may suppress the development and/or progression of human autism, schizophrenia, vascular dementia, strokes, pathological anxiety and depression disorders,[13][14] behavioral and social communication disorders,[77] and postoperative cognitive dysfunction.[78] Some of these studies mention the possibility that SCFA-induced activation of FFAR2 suppresses these diseases and disorders but give no evidence to support this. The studies often do suggest that the SCFAs act by various other mechanisms to achieve their neurological effects.[79] Furthermore, the role of SCFAs in humans with these diseases may be unclear. For example, two extensive reviews found that studies on the role of intestinal SCFAs in multiple sclerosis patients were inconclusive.[80][81] There is a need to define the precise roles of SCFAs, FFAR2, and the other proposed causal factors in these neurological diseases and disorders.[13][76]
Bacterial infections
Studies have shown that bacterial infections of the human urinary tract, vagina (i.e., bacterial vaginosis), gums (i.e., periodentitis), and abscesses in various tissues are associated with high concentrations of SCFAs, especially acetic acid, at the infection sites or, in urinary tract infections, the urine. These SCFAs may be made and released by the bacteria and/or host cells in the infected areas.[15] Several studies have suggested that SCFAs act through FFAR2 to suppress these infections. 1) Compared to control mice, Ffar2 gene knockout mice had more severe infections in models of Citrobacter rodentium, Klebsiella pneumoniae, Clostridioides difficile,[15] and Streptococcus pneumoniae bacterial infections.[82] 2) Injection of acetic acid into the peritoneum 1/2 hour before or 6 hours after injection of Staphylococcus aureus bacteria into the bloodstream of mice reduced signs of severe disease, the amount of body weight lost, and the numbers of bacteria recovered from the liver, spleen, and kidneys; these reductions did not occur in Fffar2 gene knockdown mice.[83] And, 3) higher circulating blood cell levels of FFAR2 messenger RNA were associated with higher survival rates in patients with sepsis, i.e., disseminated bacterial infections, compared to patients with lower levels of blood cell FFAR2 messenger RNA.[84] These studies suggest that FFAR2 reduces the severity of the cited bacterial infections in humans and mice and recommend further studies on the roles of FFAR2 in these and other bacterial infections.[15]
Viral infections
Mice pretreated for 4 weeks with diets that raised their intestinal SCFAs levels had reduced viral levels and pulmonary inflammation during the course of respiratory syncytial virus infection; these reductions did not occur in Ffar2 gene knockout mice or mice pretreated with antibiotics to reduce their intestines' SCFAs levels. Thus, SCFA activated FFAR2 appeared to reduce the severity of this viruses infection in mice.[15] Different results were found in a study examining influenza A virus's ability to enter and thereby infect human A549 lung cancer cells and mouse 264RAW .7 macrophages. Reduction of FFAR2 using gene knockdown methods reduced the virus's ability to enter into both cell types. Treating A549 cells with FFAR2 agonists, either 4-CMTB or compound 58, also inhibited the virus's entry into these cells. Analysis of this inhibition revealed that Influenza A virus entered these cells by binding to their surface membrane sialic acid receptors; this binding triggered endocytosis, i.e., internalization, of these cells' sialic acid receptors along with their attached viruses. A portion of the sialic acid receptor-bound virus also binds to and activates FFAR 2; this activation increased the endocytosis triggered by the virus's binding to the sialic acid receptors.[16] 4-CMTB and Compound 58 acted to block the ability of the sialic acid-bound virus to enhance endocytosis.[16][18]
FFAR2-FFAR3 receptor heteromer
The FFAR2-FFAR3 protein dimer, also termed FFAR2-FFAR3 receptor heteromer, consists of single FFAR2 and FFAR3 proteins joined together. This dimer has been detected in monocytes isolated from human blood and macrophages that were differentiated from these monocytes (see monocyte differentiation into macrophages). Like other protein dimers, the FFAR2-FFAR3 protein dimer had activities that differed from each of its FFAR monomer proteins. However, FFAR2-FFAR3 dimers have not yet been associated with specific functions, clinical disorders, or clinical diseases.[85]
References
- GRCh38: Ensembl release 89: ENSG00000126262 - Ensembl, May 2017
- GRCm38: Ensembl release 89: ENSMUSG00000051314 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Entrez Gene: FFAR1 free fatty acid receptor 1".
- Kalis M, Levéen P, Lyssenko V, Almgren P, Groop L, Cilio CM (November 2007). "Variants in the FFAR1 gene are associated with beta cell function". PLOS ONE. 2 (11): e1090. Bibcode:2007PLoSO...2.1090K. doi:10.1371/journal.pone.0001090. PMC 2042513. PMID 17987108.
- Weis WI, Kobilka BK (June 2018). "The Molecular Basis of G Protein-Coupled Receptor Activation". Annual Review of Biochemistry. 87: 897–919. doi:10.1146/annurev-biochem-060614-033910. PMC 6535337. PMID 29925258.
- Karmokar PF, Moniri NH (December 2022). "Oncogenic signaling of the free-fatty acid receptors FFA1 and FFA4 in human breast carcinoma cells". Biochemical Pharmacology. 206: 115328. doi:10.1016/j.bcp.2022.115328. PMID 36309079. S2CID 253174629.
- Kimura I, Ichimura A, Ohue-Kitano R, Igarashi M (January 2020). "Free Fatty Acid Receptors in Health and Disease". Physiological Reviews. 100 (1): 171–210. doi:10.1152/physrev.00041.2018. PMID 31487233.
- Ikeda T, Nishida A, Yamano M, Kimura I (November 2022). "Short-chain fatty acid receptors and gut microbiota as therapeutic targets in metabolic, immune, and neurological diseases". Pharmacology & Therapeutics. 239: 108273. doi:10.1016/j.pharmthera.2022.108273. PMID 36057320. S2CID 251992642.
- Kim YA, Keogh JB, Clifton PM (June 2018). "Probiotics, prebiotics, synbiotics and insulin sensitivity". Nutrition Research Reviews. 31 (1): 35–51. doi:10.1017/S095442241700018X. PMID 29037268.
- Loona DP, Das B, Kaur R, Kumar R, Yadav AK (2023). "Free Fatty Acid Receptors (FFARs): Emerging Therapeutic Targets for the Management of Diabetes Mellitus". Current Medicinal Chemistry. 30 (30): 3404–3440. doi:10.2174/0929867329666220927113614. PMID 36173072. S2CID 252598831.
- Castillo-Álvarez F, Marzo-Sola ME (2022). "Role of the gut microbiota in the development of various neurological diseases". Neurologia. 37 (6): 492–498. doi:10.1016/j.nrleng.2019.03.026. PMID 35779869.
- Mirzaei R, Bouzari B, Hosseini-Fard SR, Mazaheri M, Ahmadyousefi Y, Abdi M, Jalalifar S, Karimitabar Z, Teimoori A, Keyvani H, Zamani F, Yousefimashouf R, Karampoor S (July 2021). "Role of microbiota-derived short-chain fatty acids in nervous system disorders". Biomedicine & Pharmacotherapy. 139: 111661. doi:10.1016/j.biopha.2021.111661. PMID 34243604.
- Schlatterer K, Peschel A, Kretschmer D (2021). "Short-Chain Fatty Acid and FFAR2 Activation - A New Option for Treating Infections?". Frontiers in Cellular and Infection Microbiology. 11: 785833. doi:10.3389/fcimb.2021.785833. PMC 8674814. PMID 34926327.
- Wang G, Jiang L, Wang J, Zhang J, Kong F, Li Q, Yan Y, Huang S, Zhao Y, Liang L, Li J, Sun N, Hu Y, Shi W, Deng G, Chen P, Liu L, Zeng X, Tian G, Bu Z, Chen H, Li C (January 2020). "The G Protein-Coupled Receptor FFAR2 Promotes Internalization during Influenza A Virus Entry". Journal of Virology. 94 (2). doi:10.1128/JVI.01707-19. PMC 6955252. PMID 31694949.
- Priyadarshini M, Lednovich K, Xu K, Gough S, Wicksteed B, Layden BT (May 2021). "FFAR from the Gut Microbiome Crowd: SCFA Receptors in T1D Pathology". Metabolites. 11 (5): 302. doi:10.3390/metabo11050302. PMC 8151283. PMID 34064625.
- Milligan G, Barki N, Tobin AB (March 2021). "Chemogenetic Approaches to Explore the Functions of Free Fatty Acid Receptor 2" (PDF). Trends in Pharmacological Sciences. 42 (3): 191–202. doi:10.1016/j.tips.2020.12.003. PMID 33495026. S2CID 231712546.
- Brown AJ, Goldsworthy SM, Barnes AA, Eilert MM, Tcheang L, Daniels D, Muir AI, Wigglesworth MJ, Kinghorn I, Fraser NJ, Pike NB, Strum JC, Steplewski KM, Murdock PR, Holder JC, Marshall FH, Szekeres PG, Wilson S, Ignar DM, Foord SM, Wise A, Dowell SJ (March 2003). "The Orphan G protein-coupled receptors GPR41 and GPR43 are activated by propionate and other short chain carboxylic acids". The Journal of Biological Chemistry. 278 (13): 11312–9. doi:10.1074/jbc.M211609200. PMID 12496283.
- Miyamoto J, Ohue-Kitano R, Mukouyama H, Nishida A, Watanabe K, Igarashi M, Irie J, Tsujimoto G, Satoh-Asahara N, Itoh H, Kimura I (November 2019). "Ketone body receptor GPR43 regulates lipid metabolism under ketogenic conditions". Proceedings of the National Academy of Sciences of the United States of America. 116 (47): 23813–23821. Bibcode:2019PNAS..11623813M. doi:10.1073/pnas.1912573116. PMC 6876247. PMID 31685604.
- Lind S, Holdfeldt A, Mårtensson J, Granberg KL, Forsman H, Dahlgren C (November 2021). "Multiple ligand recognition sites in free fatty acid receptor 2 (FFA2R) direct distinct neutrophil activation patterns". Biochemical Pharmacology. 193: 114762. doi:10.1016/j.bcp.2021.114762. PMID 34499871. S2CID 237471881.
- Carretta MD, Quiroga J, López R, Hidalgo MA, Burgos RA (2021). "Participation of Short-Chain Fatty Acids and Their Receptors in Gut Inflammation and Colon Cancer". Frontiers in Physiology. 12: 662739. doi:10.3389/fphys.2021.662739. PMC 8060628. PMID 33897470.
- Hansen AH, Sergeev E, Bolognini D, Sprenger RR, Ekberg JH, Ejsing CS, McKenzie CJ, Rexen Ulven E, Milligan G, Ulven T (November 2018). "Discovery of a Potent Thiazolidine Free Fatty Acid Receptor 2 Agonist with Favorable Pharmacokinetic Properties". Journal of Medicinal Chemistry. 61 (21): 9534–9550. doi:10.1021/acs.jmedchem.8b00855. PMID 30247908.
- Al Mahri S, Malik SS, Al Ibrahim M, Haji E, Dairi G, Mohammad S (February 2022). "Free Fatty Acid Receptors (FFARs) in Adipose: Physiological Role and Therapeutic Outlook". Cells. 11 (4): 750. doi:10.3390/cells11040750. PMC 8870169. PMID 35203397.
- Iwasaki K, Harada N, Sasaki K, Yamane S, Iida K, Suzuki K, Hamasaki A, Nasteska D, Shibue K, Joo E, Harada T, Hashimoto T, Asakawa Y, Hirasawa A, Inagaki N (March 2015). "Free fatty acid receptor GPR120 is highly expressed in enteroendocrine K cells of the upper small intestine and has a critical role in GIP secretion after fat ingestion". Endocrinology. 156 (3): 837–46. doi:10.1210/en.2014-1653. hdl:2433/215430. PMID 25535828.
- Mishra SP, Karunakar P, Taraphder S, Yadav H (June 2020). "Free Fatty Acid Receptors 2 and 3 as Microbial Metabolite Sensors to Shape Host Health: Pharmacophysiological View". Biomedicines. 8 (6): 154. doi:10.3390/biomedicines8060154. PMC 7344995. PMID 32521775.
- Jorsal T, Rhee NA, Pedersen J, Wahlgren CD, Mortensen B, Jepsen SL, Jelsing J, Dalbøge LS, Vilmann P, Hassan H, Hendel JW, Poulsen SS, Holst JJ, Vilsbøll T, Knop FK (February 2018). "Enteroendocrine K and L cells in healthy and type 2 diabetic individuals". Diabetologia. 61 (2): 284–294. doi:10.1007/s00125-017-4450-9. PMID 28956082.
- Lorza-Gil E, Kaiser G, Rexen Ulven E, König GM, Gerst F, Oquendo MB, Birkenfeld AL, Häring HU, Kostenis E, Ulven T, Ullrich S (October 2020). "FFA2-, but not FFA3-agonists inhibit GSIS of human pseudoislets: a comparative study with mouse islets and rat INS-1E cells". Scientific Reports. 10 (1): 16497. doi:10.1038/s41598-020-73467-5. PMC 7536384. PMID 33020504.
- Lind S, Holdfeldt A, Mårtensson J, Sundqvist M, Kenakin TP, Björkman L, Forsman H, Dahlgren C (June 2020). "Interdependent allosteric free fatty acid receptor 2 modulators synergistically induce functional selective activation and desensitization in neutrophils". Biochimica et Biophysica Acta (BBA) - Molecular Cell Research. 1867 (6): 118689. doi:10.1016/j.bbamcr.2020.118689. PMID 32092308.
- Lavoie S, Chun E, Bae S, Brennan CA, Gallini Comeau CA, Lang JK, Michaud M, Hoveyda HR, Fraser GL, Fuller MH, Layden BT, Glickman JN, Garrett WS (April 2020). "Expression of Free Fatty Acid Receptor 2 by Dendritic Cells Prevents Their Expression of Interleukin 27 and Is Required for Maintenance of Mucosal Barrier and Immune Response Against Colorectal Tumors in Mice". Gastroenterology. 158 (5): 1359–1372.e9. doi:10.1053/j.gastro.2019.12.027. PMC 7291292. PMID 31917258.
- Xiu W, Chen Q, Wang Z, Wang J, Zhou Z (December 2020). "Microbiota-derived short chain fatty acid promotion of Amphiregulin expression by dendritic cells is regulated by GPR43 and Blimp-1". Biochemical and Biophysical Research Communications. 533 (3): 282–288. doi:10.1016/j.bbrc.2020.09.027. PMID 32958255. S2CID 221843901.
- Nilsson NE, Kotarsky K, Owman C, Olde B (April 2003). "Identification of a free fatty acid receptor, FFA2R, expressed on leukocytes and activated by short-chain fatty acids". Biochemical and Biophysical Research Communications. 303 (4): 1047–52. doi:10.1016/S0006-291X(03)00488-1. PMID 12684041.
- Pluznick JL, Protzko RJ, Gevorgyan H, Peterlin Z, Sipos A, Han J, Brunet I, Wan LX, Rey F, Wang T, Firestein SJ, Yanagisawa M, Gordon JI, Eichmann A, Peti-Peterdi J, Caplan MJ (March 2013). "Olfactory receptor responding to gut microbiota-derived signals plays a role in renin secretion and blood pressure regulation". Proceedings of the National Academy of Sciences of the United States of America. 110 (11): 4410–5. Bibcode:2013PNAS..110.4410P. doi:10.1073/pnas.1215927110. PMC 3600440. PMID 23401498.
- Nauck MA, Meier JJ (February 2018). "Incretin hormones: Their role in health and disease". Diabetes, Obesity & Metabolism. 20 (Suppl 1): 5–21. doi:10.1111/dom.13129. PMID 29364588.
- de Vos WM, Tilg H, Van Hul M, Cani PD (May 2022). "Gut microbiome and health: mechanistic insights". Gut. 71 (5): 1020–1032. doi:10.1136/gutjnl-2021-326789. PMC 8995832. PMID 35105664.
- Mazhar M, Zhu Y, Qin L (February 2023). "The Interplay of Dietary Fibers and Intestinal Microbiota Affects Type 2 Diabetes by Generating Short-Chain Fatty Acids". Foods (Basel, Switzerland). 12 (5): 1023. doi:10.3390/foods12051023. PMC 10001013. PMID 36900540.
- Kasarello K, Cudnoch-Jedrzejewska A, Czarzasta K (2023). "Communication of gut microbiota and brain via immune and neuroendocrine signaling". Frontiers in Microbiology. 14: 1118529. doi:10.3389/fmicb.2023.1118529. PMC 9907780. PMID 36760508.
- Bermudez LE, Young LS (1987). "Phagocytosis and intracellular killing of Mycobacterium avium complex by human and murine macrophages". Brazilian Journal of Medical and Biological Research = Revista Brasileira de Pesquisas Medicas e Biologicas. 20 (2): 191–201. PMID 3690054.
- Ghislain J, Poitout V (March 2021). "Targeting lipid GPCRs to treat type 2 diabetes mellitus - progress and challenges". Nature Reviews. Endocrinology. 17 (3): 162–175. doi:10.1038/s41574-020-00459-w. PMID 33495605. S2CID 231695737.
- Müller TD, Finan B, Bloom SR, D'Alessio D, Drucker DJ, Flatt PR, Fritsche A, Gribble F, Grill HJ, Habener JF, Holst JJ, Langhans W, Meier JJ, Nauck MA, Perez-Tilve D, Pocai A, Reimann F, Sandoval DA, Schwartz TW, Seeley RJ, Stemmer K, Tang-Christensen M, Woods SC, DiMarchi RD, Tschöp MH (December 2019). "Glucagon-like peptide 1 (GLP-1)". Molecular Metabolism. 30: 72–130. doi:10.1016/j.molmet.2019.09.010. PMC 6812410. PMID 31767182.
- Holst JJ, Gasbjerg LS, Rosenkilde MM (July 2021). "The Role of Incretins on Insulin Function and Glucose Homeostasis". Endocrinology. 162 (7). doi:10.1210/endocr/bqab065. PMC 8168943. PMID 33782700.
- Tan M, Lamendola C, Luong R, McLaughlin T, Craig C (August 2020). "Safety, efficacy and pharmacokinetics of repeat subcutaneous dosing of avexitide (exendin 9-39) for treatment of post-bariatric hypoglycaemia". Diabetes, Obesity & Metabolism. 22 (8): 1406–1416. doi:10.1111/dom.14048. PMID 32250530. S2CID 214809891.
- Lynggaard MB, Gasbjerg LS, Christensen MB, Knop FK (December 2020). "GIP(3-30)NH2 - a tool for the study of GIP physiology". Current Opinion in Pharmacology. 55: 31–40. doi:10.1016/j.coph.2020.08.011. PMID 33053504. S2CID 222420789.
- Gasbjerg LS, Helsted MM, Hartmann B, Jensen MH, Gabe BN, Sparre-Ulrich AH, Veedfald S, Stensen S, Lanng AR, Bergmann NC, Christensen MB, Vilsbøll T, Holst JJ, Rosenkilde MM, Knop FK (May 2019). "Separate and Combined Glucometabolic Effects of Endogenous Glucose-Dependent Insulinotropic Polypeptide and Glucagon-like Peptide 1 in Healthy Individuals". Diabetes. 68 (5): 906–917. doi:10.2337/db18-1123. PMID 30626611.
- Scott LJ (February 2020). "Dulaglutide: A Review in Type 2 Diabetes". Drugs. 80 (2): 197–208. doi:10.1007/s40265-020-01260-9. PMID 32002850. S2CID 210954338.
- Bradley CL, McMillin SM, Hwang AY, Sherrill CH (July 2023). "Tirzepatide, the Newest Medication for Type 2 Diabetes: A Review of the Literature and Implications for Clinical Practice". The Annals of Pharmacotherapy. 57 (7): 822–836. doi:10.1177/10600280221134127. PMID 36367094. S2CID 253457679.
- Villa SR, Priyadarshini M, Fuller MH, Bhardwaj T, Brodsky MR, Angueira AR, Mosser RE, Carboneau BA, Tersey SA, Mancebo H, Gilchrist A, Mirmira RG, Gannon M, Layden BT (June 2016). "Loss of Free Fatty Acid Receptor 2 leads to impaired islet mass and beta cell survival". Scientific Reports. 6: 28159. Bibcode:2016NatSR...628159V. doi:10.1038/srep28159. PMC 4914960. PMID 27324831.
- McNelis JC, Lee YS, Mayoral R, van der Kant R, Johnson AM, Wollam J, Olefsky JM (September 2015). "GPR43 Potentiates β-Cell Function in Obesity". Diabetes. 64 (9): 3203–17. doi:10.2337/db14-1938. PMC 4542437. PMID 26023106.
- Mariño E, Richards JL, McLeod KH, Stanley D, Yap YA, Knight J, McKenzie C, Kranich J, Oliveira AC, Rossello FJ, Krishnamurthy B, Nefzger CM, Macia L, Thorburn A, Baxter AG, Morahan G, Wong LH, Polo JM, Moore RJ, Lockett TJ, Clarke JM, Topping DL, Harrison LC, Mackay CR (May 2017). "Gut microbial metabolites limit the frequency of autoimmune T cells and protect against type 1 diabetes". Nature Immunology. 18 (5): 552–562. doi:10.1038/ni.3713. PMID 28346408. S2CID 30078908.
- Harbison JE, Roth-Schulze AJ, Giles LC, Tran CD, Ngui KM, Penno MA, Thomson RL, Wentworth JM, Colman PG, Craig ME, Morahan G, Papenfuss AT, Barry SC, Harrison LC, Couper JJ (August 2019). "Gut microbiome dysbiosis and increased intestinal permeability in children with islet autoimmunity and type 1 diabetes: A prospective cohort study". Pediatric Diabetes. 20 (5): 574–583. doi:10.1111/pedi.12865. hdl:11343/285878. PMID 31081243. S2CID 153308576.
- Simon MC, Reinbeck AL, Wessel C, Heindirk J, Jelenik T, Kaul K, Arreguin-Cano J, Strom A, Blaut M, Bäckhed F, Burkart V, Roden M (January 2020). "Distinct alterations of gut morphology and microbiota characterize accelerated diabetes onset in nonobese diabetic mice". The Journal of Biological Chemistry. 295 (4): 969–980. doi:10.1074/jbc.RA119.010816. PMC 6983849. PMID 31822562.
- Maslowski KM, Vieira AT, Ng A, Kranich J, Sierro F, Yu D, Schilter HC, Rolph MS, Mackay F, Artis D, Xavier RJ, Teixeira MM, Mackay CR (October 2009). "Regulation of inflammatory responses by gut microbiota and chemoattractant receptor GPR43". Nature. 461 (7268): 1282–6. Bibcode:2009Natur.461.1282M. doi:10.1038/nature08530. PMC 3256734. PMID 19865172.
- Tan J, McKenzie C, Vuillermin PJ, Goverse G, Vinuesa CG, Mebius RE, Macia L, Mackay CR (June 2016). "Dietary Fiber and Bacterial SCFA Enhance Oral Tolerance and Protect against Food Allergy through Diverse Cellular Pathways". Cell Reports. 15 (12): 2809–24. doi:10.1016/j.celrep.2016.05.047. hdl:1885/153817. PMID 27332875.
- Han X, Krempski JW, Nadeau K (December 2020). "Advances and novel developments in mechanisms of allergic inflammation". Allergy. 75 (12): 3100–3111. doi:10.1111/all.14632. PMID 33068299.
- Ang Z, Ding JL (2016). "GPR41 and GPR43 in Obesity and Inflammation - Protective or Causative?". Frontiers in Immunology. 7: 28. doi:10.3389/fimmu.2016.00028. PMC 4734206. PMID 26870043.
- Orji OC, López-Domínguez MB, Sandoval-Plata G, Guetta-Baranes T, Valdes AM, Doherty M, Morgan K, Abhishek A (February 2023). "Upregulated expression of FFAR2 and SOC3 genes is associated with gout". Rheumatology. 62 (2): 977–983. doi:10.1093/rheumatology/keac360. PMC 9891400. PMID 35731142.
- Namour F, Galien R, Van Kaem T, Van der Aa A, Vanhoutte F, Beetens J, Van't Klooster G (July 2016). "Safety, pharmacokinetics and pharmacodynamics of GLPG0974, a potent and selective FFA2 antagonist, in healthy male subjects". British Journal of Clinical Pharmacology. 82 (1): 139–48. doi:10.1111/bcp.12900. PMC 4917808. PMID 26852904.
- Sergeev E, Hansen AH, Bolognini D, Kawakami K, Kishi T, Aoki J, Ulven T, Inoue A, Hudson BD, Milligan G (October 2017). "A single extracellular amino acid in Free Fatty Acid Receptor 2 defines antagonist species selectivity and G protein selection bias". Scientific Reports. 7 (1): 13741. Bibcode:2017NatSR...713741S. doi:10.1038/s41598-017-14096-3. PMC 5653858. PMID 29061999.
- Ge H, Li X, Weiszmann J, Wang P, Baribault H, Chen JL, Tian H, Li Y (September 2008). "Activation of G protein-coupled receptor 43 in adipocytes leads to inhibition of lipolysis and suppression of plasma free fatty acids". Endocrinology. 149 (9): 4519–26. doi:10.1210/en.2008-0059. PMID 18499755.
- Suokas A, Kupari M, Heikkilä J, Lindros K, Ylikahri R (February 1988). "Acute cardiovascular and metabolic effects of acetate in men". Alcoholism: Clinical and Experimental Research. 12 (1): 52–8. doi:10.1111/j.1530-0277.1988.tb00132.x. PMID 3279860.
- Laurent C, Simoneau C, Marks L, Braschi S, Champ M, Charbonnel B, Krempf M (July 1995). "Effect of acetate and propionate on fasting hepatic glucose production in humans". European Journal of Clinical Nutrition. 49 (7): 484–91. PMID 7588498.
- Spigoni V, Cinquegrani G, Iannozzi NT, Frigeri G, Maggiolo G, Maggi M, Parello V, Dei Cas A (2022). "Activation of G protein-coupled receptors by ketone bodies: Clinical implication of the ketogenic diet in metabolic disorders". Frontiers in Endocrinology. 13: 972890. doi:10.3389/fendo.2022.972890. PMC 9631778. PMID 36339405.
- Aalling, Nadia Nielsen; Nedergaard, Maiken; DiNuzzo, Mauro (July 16, 2018). "Cerebral Metabolic Changes During Sleep". Current Neurology and Neuroscience Reports. 18 (9): 57. doi:10.1007/s11910-018-0868-9. PMC 6688614. PMID 30014344.
- Xu J, Moore BN, Pluznick JL (October 2022). "Short-Chain Fatty Acid Receptors and Blood Pressure Regulation: Council on Hypertension Mid-Career Award for Research Excellence 2021". Hypertension. 79 (10): 2127–2137. doi:10.1161/HYPERTENSIONAHA.122.18558. PMC 9458621. PMID 35912645. S2CID 251222823.
- de Sequera P, Pérez-García R, Molina M, Álvarez-Fernández G, Muñoz-González RI, Mérida E, Camba MJ, Blázquez LA, Alcaide MP, Echarri R (2022). "Advantages of the use of citrate over acetate as a stabilizer in hemodialysis fluid: A randomized ABC-treat study". Nefrologia. 42 (3): 327–337. doi:10.1016/j.nefroe.2021.12.003. PMID 36210622.
- Zhuang R, Chen J, Cheng HS, Assa C, Jamaiyar A, Pandey AK, Pérez-Cremades D, Zhang B, Tzani A, Khyrul Wara A, Plutzky J, Barrera V, Bhetariya P, Mitchell RN, Liu Z, Feinberg MW (May 2022). "Perivascular Fibrosis Is Mediated by a KLF10-IL-9 Signaling Axis in CD4+ T Cells". Circulation Research. 130 (11): 1662–1681. doi:10.1161/CIRCRESAHA.121.320420. PMC 9149118. PMID 35440172.
- Kaye DM, Shihata WA, Jama HA, Tsyganov K, Ziemann M, Kiriazis H, Horlock D, Vijay A, Giam B, Vinh A, Johnson C, Fiedler A, Donner D, Snelson M, Coughlan MT, Phillips S, Du XJ, El-Osta A, Drummond G, Lambert GW, Spector TD, Valdes AM, Mackay CR, Marques FZ (April 2020). "Deficiency of Prebiotic Fiber and Insufficient Signaling Through Gut Metabolite-Sensing Receptors Leads to Cardiovascular Disease". Circulation. 141 (17): 1393–1403. doi:10.1161/CIRCULATIONAHA.119.043081. PMID 32093510. S2CID 211476145.
- Nakai M, Ribeiro RV, Stevens BR, Gill P, Muralitharan RR, Yiallourou S, Muir J, Carrington M, Head GA, Kaye DM, Marques FZ (September 2021). "Essential Hypertension Is Associated With Changes in Gut Microbial Metabolic Pathways: A Multisite Analysis of Ambulatory Blood Pressure". Hypertension. 78 (3): 804–815. doi:10.1161/HYPERTENSIONAHA.121.17288. PMID 34333988.
- Mirzaei R, Afaghi A, Babakhani S, Sohrabi MR, Hosseini-Fard SR, Babolhavaeji K, Khani Ali Akbari S, Yousefimashouf R, Karampoor S (July 2021). "Role of microbiota-derived short-chain fatty acids in cancer development and prevention". Biomedicine & Pharmacotherapy. 139: 111619. doi:10.1016/j.biopha.2021.111619. PMID 33906079.
- Pan P, Oshima K, Huang YW, Agle KA, Drobyski WR, Chen X, Zhang J, Yearsley MM, Yu J, Wang LS (August 2018). "Loss of FFAR2 promotes colon cancer by epigenetic dysregulation of inflammation suppressors". International Journal of Cancer. 143 (4): 886–896. doi:10.1002/ijc.31366. PMC 6041131. PMID 29524208.
- Kim MJ, Kim JY, Shin JH, Kang Y, Lee JS, Son J, Jeong SK, Kim D, Kim DH, Chun E, Lee KY (June 2023). "FFAR2 antagonizes TLR2- and TLR3-induced lung cancer progression via the inhibition of AMPK-TAK1 signaling axis for the activation of NF-κB". Cell & Bioscience. 13 (1): 102. doi:10.1186/s13578-023-01038-y. PMC 10249240. PMID 37287005.
- Xiao X, Xu Y, Chen H (May 2020). "Sodium butyrate-activated TRAF6-TXNIP pathway affects A549 cells proliferation and migration". Cancer Medicine. 9 (10): 3477–3488. doi:10.1002/cam4.2564. PMC 7221305. PMID 31578830.
- Semaan J, El-Hakim S, Ibrahim JN, Safi R, Elnar AA, El Boustany C (July 2020). "Comparative effect of sodium butyrate and sodium propionate on proliferation, cell cycle and apoptosis in human breast cancer cells MCF-7". Breast Cancer (Tokyo, Japan). 27 (4): 696–705. doi:10.1007/s12282-020-01063-6. PMID 32095987. S2CID 211265423.
- Wang F, Wu H, Fan M, Yu R, Zhang Y, Liu J, Zhou X, Cai Y, Huang S, Hu Z, Jin X (March 2020). "Sodium butyrate inhibits migration and induces AMPK-mTOR pathway-dependent autophagy and ROS-mediated apoptosis via the miR-139-5p/Bmi-1 axis in human bladder cancer cells". FASEB Journal. 34 (3): 4266–4282. doi:10.1096/fj.201902626R. PMID 31957111. S2CID 210832147.
- Borst K, Dumas AA, Prinz M (October 2021). "Microglia: Immune and non-immune functions". Immunity. 54 (10): 2194–2208. doi:10.1016/j.immuni.2021.09.014. PMID 34644556. S2CID 238858388.
- Sun Y, Zhang H, Zhang X, Wang W, Chen Y, Cai Z, Wang Q, Wang J, Shi Y (June 2023). "Promotion of astrocyte-neuron glutamate-glutamine shuttle by SCFA contributes to the alleviation of Alzheimer's disease". Redox Biology. 62: 102690. doi:10.1016/j.redox.2023.102690. PMC 10122027. PMID 37018970.
- Stilling RM, van de Wouw M, Clarke G, Stanton C, Dinan TG, Cryan JF (October 2016). "The neuropharmacology of butyrate: The bread and butter of the microbiota-gut-brain axis?". Neurochemistry International. 99: 110–132. doi:10.1016/j.neuint.2016.06.011. PMID 27346602. S2CID 207124576.
- Luo A, Li S, Wang X, Xie Z, Li S, Hua D (2021). "Cefazolin Improves Anesthesia and Surgery-Induced Cognitive Impairments by Modulating Blood-Brain Barrier Function, Gut Bacteria and Short Chain Fatty Acids". Frontiers in Aging Neuroscience. 13: 748637. doi:10.3389/fnagi.2021.748637. PMC 8548472. PMID 34720997.
- Eicher TP, Mohajeri MH (June 2022). "Overlapping Mechanisms of Action of Brain-Active Bacteria and Bacterial Metabolites in the Pathogenesis of Common Brain Diseases". Nutrients. 14 (13): 2661. doi:10.3390/nu14132661. PMC 9267981. PMID 35807841.
- Valburg C, Sonti A, Stern JN, Najjar S, Harel A (April 2021). "Dietary factors in experimental autoimmune encephalomyelitis and multiple sclerosis: A comprehensive review". Multiple Sclerosis (Houndmills, Basingstoke, England). 27 (4): 494–502. doi:10.1177/1352458520923955. PMID 32406797. S2CID 218633615.
- Ghezzi L, Cantoni C, Pinget GV, Zhou Y, Piccio L (July 2021). "Targeting the gut to treat multiple sclerosis". The Journal of Clinical Investigation. 131 (13). doi:10.1172/JCI143774. PMC 8245171. PMID 34196310.
- Galvão I, Tavares LP, Corrêa RO, Fachi JL, Rocha VM, Rungue M, Garcia CC, Cassali G, Ferreira CM, Martins FS, Oliveira SC, Mackay CR, Teixeira MM, Vinolo MA, Vieira AT (2018). "The Metabolic Sensor GPR43 Receptor Plays a Role in the Control of Klebsiella pneumoniae Infection in the Lung". Frontiers in Immunology. 9: 142. doi:10.3389/fimmu.2018.00142. PMC 5826235. PMID 29515566.
- Schlatterer K, Beck C, Schoppmeier U, Peschel A, Kretschmer D (July 2021). "Acetate sensing by GPR43 alarms neutrophils and protects from severe sepsis". Communications Biology. 4 (1): 928. doi:10.1038/s42003-021-02427-0. PMC 8324776. PMID 34330996.
- Carr ZJ, Van De Louw A, Fehr G, Li JD, Kunselman A, Ruiz-Velasco V (January 2018). "Increased whole blood FFA2/GPR43 receptor expression is associated with increased 30-day survival in patients with sepsis". BMC Research Notes. 11 (1): 41. doi:10.1186/s13104-018-3165-4. PMC 5771199. PMID 29338778.
- Ang Z, Xiong D, Wu M, Ding JL (January 2018). "FFAR2-FFAR3 receptor heteromerization modulates short-chain fatty acid sensing". FASEB Journal. 32 (1): 289–303. doi:10.1096/fj.201700252RR. PMC 5731126. PMID 28883043.
Further reading
- Kimura I, Ichimura A, Ohue-Kitano R, Igarashi M (January 2020). "Free Fatty Acid Receptors in Health and Disease". Physiological Reviews. 100 (1): 171–210. doi:10.1152/physrev.00041.2018. PMID 31487233.
- Castillo-Álvarez F, Marzo-Sola ME (2022). "Role of the gut microbiota in the development of various neurological diseases". Neurologia. 37 (6): 492–498. doi:10.1016/j.nrleng.2019.03.026. PMID 35779869.
- Ikeda T, Nishida A, Yamano M, Kimura I (November 2022). "Short-chain fatty acid receptors and gut microbiota as therapeutic targets in metabolic, immune, and neurological diseases". Pharmacology & Therapeutics. 239: 108273. doi:10.1016/j.pharmthera.2022.108273. PMID 36057320. S2CID 251992642.