Hydroxycarboxylic acid receptor 2
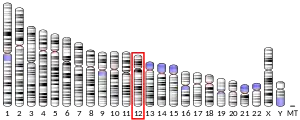
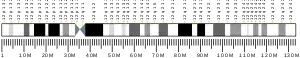
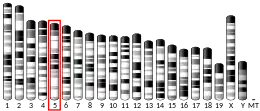
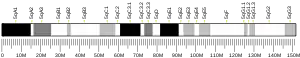
Hydroxycarboxylic acid receptor 2 (HCA2), also known as GPR109A and niacin receptor 1 (NIACR1), is a protein which in humans is encoded (its formation is directed) by the HCAR2 gene and in rodents by the Hcar2 gene.[5][6][7][8] The human HCAR2 gene is located on the long (i.e., "q") arm of chromosome 12 at position 24.31 (notated as 12q24.31).[9] Like the two other hydroxycarboxylic acid receptors, HCA1 and HCA3, HCA2 is a G protein-coupled receptor (GPCR) located on the surface membrane of cells.[5][10] HCA2 binds and thereby is activated by D-β-hydroxybutyric acid (hereafter termed β-hydroxybutyric acid), butyric acid, and niacin (also known as nicotinic acid).[7][8] β-Hydroxybutyric and butyric acids are regarded as the endogenous agents that activate HCA2. Under normal conditions, niacin's blood levels are too low to do so: it is given as a drug in high doses in order to reach levels that activate HCA2.[11]
| HCAR2 | |||||||||||||||||||||||||||||||||||||||||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| Identifiers | |||||||||||||||||||||||||||||||||||||||||||||||||||
| Aliases | HCAR2, GPR109A, HCA2, HM74a, HM74b, NIACR1, PUMAG, Puma-g, Niacin receptor 1, hydroxycarboxylic acid receptor 2 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| External IDs | OMIM: 609163 MGI: 1933383 HomoloGene: 4391 GeneCards: HCAR2 | ||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
| Wikidata | |||||||||||||||||||||||||||||||||||||||||||||||||||
| |||||||||||||||||||||||||||||||||||||||||||||||||||
β-Hydroxybutyric acid, butyric acid, and niacin have actions that are independent of HCA2. For example: 1) β-hydroxybutyric acid activates free fatty acid receptor 3[12] and inhibits some histone deacetylases that regulate the expression of various genes, increase mitochondrial adenosine triphosphate production, and promote antioxidant defenses;[13] 2) butyric acid activates free fatty acid receptor 2 and like β-hydroxybutyric acid activates free fatty acid receptor 3[14] and inhibits some histone deacetylases;[15] and 3) niacin is an NAD+ precursor (see nicotinamide adenine dinucleotide) which when converted to NAD+ can alter over 500 enzymatic reactions that play key roles in regulating inflammation, mitochondrion functions, autophagy, and apoptosis.[13] Consequently, studies examining the functions of HCA2 based on the actions of butyric acid, β-hydroxybutyric acid, niacin, or other HCA2 activators need to provide data indicating that they actually do so by activating HCA2. One commonly used way to do this is to show that the activators have no or reduced effects on Hca2 gene knockout cells or animals (i.e., cells or animals that had their HCa2 genes removed or inactivated) or gene knockdown cells or animals (i.e., cells or animals that had their HCa2 genes ability to express HCA2 greatly reduced).[16] The studies reported here on HCA2 activators focus on those that included experiments in Hca2 gene knockout and/or knockdown cells and animals.
Studies, done mostly in animals and the cells taken from animals or humans, show or suggest that HCA2 functions to 1) inhibit lipolysis and 2) inhibit inflammation and thereby suppress the development of certain diseases in which inflammation contributes to their development and/or severity.[13][17][18] These diseases include: atherosclerosis,[19] stroke, Alzheimer's disease, Parkinson's disease, multiple sclerosis, pathological pain (i.e. pain due to the abnormal activation of neurons),[13] mastitis,[20] hepatitis due to heavy alcohol consumption,[21] inflammatory bowel diseases, cancer of the colon,[22] and, possibly, psoriasis[23] and brain damage due to heavy alcohol consumption.[24]
HCA2 and HCA3 homodimer and heterodimer proteins
HCA2 is commonly formed and regarded as a homodimer, i.e. to be composed of two adjoined HCA2 proteins. However, a heterodimer composed of the HCA2 protein adjoined to the HCA3 protein has been detected in human embryonic kidney HEK 293 cells. The human HCAR2 and HCAR3 genes sit next to each other on chromosome 12 at position 24.31 and have an amino acid sequence homology greater than 95%. While there appears to be no significant difference in the responses triggered by activation of cells expressing the HCA2 homodimer versus the HCA2/HCA3 heterodimer proteins, more studies are needed to confirm this.[13] Furthermore: 1) HCA2 and HCA1 are found in most mammalian species but HCA3 is found only in higher primates[5] and 2) monodimeric HCA2 and HCA3 proteins may show very different ligand sensitivities, e.g., niacin binds to and activates HCA2 but does not or only weakly binds to and activates HCA3.[25] Studies on HCA2 in human cells and tissues have not determined the extent to which these cells and tissues also express HCA3 and form HCA3-HCA3 heterodimers. The studies cited here may need to be revised if future studies find that HCA2-HCA3 heterodimers are involved in the effects of "HCA2 activators".[13]
Cells and tissues expressing HCA2
HCA2 is expressed by: 1) certain cells in the immune system, e.g., neutrophils, monocytes, macrophages, dermal dendritic cells,[18] and lymphocytes;[13] 2) cells in the small intestine and colon epithelum that face the intestinal lumen;[26] 3) the skin's epithelial cells, keratinocytes, and Langerhans cells;[27] 4) brown and white adipose tissue fat cells;[28] 5) cells in the mammary gland's epithelium;[20] 6) hepatocytes; 7) multinucleated osteoclasts in bone tissues; 8) kidney podocytes;[13] and 9) cells in the nervous system, e.g., microglia cells in the brain's cerebral cortex and hippocampus,[24] cells in the eye's retinal pigment epithelium,[29][30] the astrocytes and neurons in the brain's rostral ventrolateral medulla, and the peripheral nervous system's Schwann and satellite glial cells.[13]
HCA2 activating agents
In addition to butyric acid, β-hydroxybutyric acid, and niacin, the following agents have been reported to activate HCA2: monomethyl fumarate,[27] dimethyl fumarate (dimethyl fumarate is a prodrug, i.e. it does not directly activate HCA2 but is rapidly converted in animal intestines to monomethyl fumarate[23][31]),[13][32] Acifran (Acifran also binds to HCA3 but with less affinity for it than for HCA3[25]), Acipimox, SCH 900271,[27] MK-6892,[33] MK-1903,[34] GSK256073,[35] and N2L.[36]
HCA2's function in lipolysis
Lipolysis is the metabolic pathway in which triglycerides are hydrolyzed, i.e., enzymatically broken down, into their component free fatty acids and glycerol. The activation of this pathway leads fat cells to release the newly freed fatty acids into the circulation and thereby raises serum free fatty acid levels; the inhibition of this lipolysis leads to falls in serum free fatty acid levels. The intravascular injection of niacin into control mice rapidly reduced their serum fatty acid levels but did not do so in Hcar2 gene knockout mice. Thus, HCA2 functions to inhibit lipolysis and lower serum fatty acid levels in mice.[37] Niacin likewise inhibits lipolysis to lower free fatty acid plasma levels in humans. Furthermore, the HCA2-activating drug, MK-1903, when taken orally by healthy volunteers in phase 1 and 2 clinical trials, dramatically lowered their plasma free fatty acids levels. Like niacin, flushing was the drug's only major adverse effect. Unlike niacin, however, MK-1903 had far less effects than niacin on the plasma levels of triglycerides and HDL-c] (i.e., cholesterol-associated High density lipoprotein) which are niacin's therapeutic targets for treating primary hyperlipidemia and hypertriglyceridemia. These findings suggest but need further studies to determine if niacin and Mk-1903 inhibit lipolysis in humans by activating HCA2.[38] Studies suggest that HCA1 and, possibly, HCA3 also inhibit lipolysis.[27]
HCA2's functions in various diseases
Atherosclerosis
Atherosclerosis is a chronic inflammatory arterial disease that can cause the narrowing or occlusion of arteries and thereby various cardiovascular diseases such as heart attacks and strokes. In a murine ApoE−/− model of atherosclerosis, mice were feed a cholesterol‐rich (i.e., atherosclerosis-promoting) diet concurrently with β-hydroxybutyric acid, nicotine, or salt water daily for 9 weeks. The aortas of β-hydroxybutyric acid-treated and niacin-treated mice had far less histological evidence of atherosclerosis (i.e., less atherosclerotic plaques, lipid depositions, and infiltrating M1 inflammation-promoting macrophages) than salt water-treated mice. β-Hydroxybutyric acid-fed mice also had significantly lower blood plasma levels of three pro-inflammatory cytokines, tumor necrosis factor-α, interleukin-6, and interleukin-1β, than salt water-treated mice. Further studies found that 1) β-hydroxybutyric acid inhibited lipopolysaccharide-simulated maturation of normal bone marrow‐derived macrophages to M1 macrophages but did not do so in macrophages taken from the bone marrows of Hcar2 gene knockout mice and 2) mice constructed to have Hcar2 gene knockout but no normal bone marrow cells who were treated with β-hydroxybutyric acid had significantly more evidence of arterial inflammation and atherosclerosis than β-hydroxybutyric acid-treated mice who had normal bone marrow cells. These results indicate that the anti-inflammatory and anti-atherosclerotic effects of β-hydroxybutyric acid in ApoE−/− mice depend on bone‐marrow‐derived HCA2-expressing cells, possibly M1 macrophages. Further studies are needed to determine if HCA2 acts to suppress the development and/or progression of human atherosclerosis.[13][39]
Stroke
Stroke is the development of persistent brain disfunction caused by the interruption of blow flow and subsequent damage to the brain. The inflammation that develops in damaged areas of the brain causes further brain damage.[13] Studies have reported that HCA2 reduces the inflammation and thereby the extent of brain damage in animal models of stroke. Mice that had a distal portion of their middle cerebral arteries occluded were treated with either β-hydroxybutyric acid or niacin shortly before and up to 48 hours after occluding the artery. β-Hydroxybutyric acid-treated mice had less damaged brain tissue and better performances in corner testing (i.e., control mice but not β-hydroxybutyric acid-treated mice tended to turn toward the side opposite the damaged brain site). β-Hydroxybutyric acid did not reduce the brain damage or improve corner test performance in Hca2 gene knockout mice. Niacin likewise reduced the size of the damaged brain site in normal but not in Hca2 gene knockout mice. And, mice feed a ketogenic diet for 14 days (which increased their plasma levels of β-hydroxybutyric acid) also had reductions in the size of their brains' damaged sites. The diet had no such effect inHca2 gene knockout mice. Further studies indicated that the effect of niacin in reducing the size of damage brain sites involved the stimulation of HCA2-bearing monocytes and/or macrophages to produce prostaglandin D2.[40] (Prostaglandin D2 has anti-inflammatory actions.[41]) Finally, several other studies, while not examining Hcar2 gene knockout or knockdown animals, reported that β-hydroxybutyric acid, niacin. monomethyl fumarate, and dimethyl fumarate reduced the inflammation, tissue damage, and/or symptoms in middle cerebral artery occlusion animal models of stroke. These results indicate that HCA2 reduces the clinical consequences of stroke in rodents and support further studies that may lead to the development of novel treatments for stroke in humans.[13]
Alzheimer's disease
Alzheimer's disease is a form of dementia that is associated with the activation of the brain's pro-inflammatory microglial cells; the increased production of pro-inflammatory cytokines; and the accumulation in the brain of a) extracellular amyloid plaques consisting of misfolded amyloid-β protein, b) amyloid-beta precursor protein (which is enzymatically broken down to amyloid-β protein), and c) intracellular aggregates of hyperphosphorylated tau protein. Individuals with Alzheimer's disease commonly show progressively worsening declines in cognitive, behavioral, and sensorimotor functions[42] along with increasing accumulations of aggregated amyloid-β proteins (which may be a key factor in the development of Alzheimer's disease).[43] In the 5XFAD murine model of Alzheimer's disease, mice were treated with β-hydroxybutyric acid or a placebo. Compared to placebo-treated mice, β-hydroxybutyric acid-mice showed better performances in cognitive/memory testing; lower brain levels of the pro-inflammatory cytokines interleukin-1 beta, tumor necrosis factor-alpha, and interleukin-6; lower levels of brain amyloid-beta precursor protein and amyloid-β protein; and higher levels of neprilysin, an enzyme that degrades amyloid proteins and is essential to prevent Alzheimer's disease in mice (i.e., mice lacking a functional gene that encodes neprilysin develop Alzheimer's disease-like symptoms).[13][42] In another study, 5xFAD mice who received β-hydroxybutyric acid subcutaneously for 28 days showed better cognitive functions, lower levels of Aβ peptide accumulation in the brain, and greater activation of microglia cells in the brain compared to placebo-treated mice. Furthermore, HCA2 messenger RNA levels were increased in the brains of these mice during the period of active plaque deposition. (The postmortem brain tissues of patients with Alzheimer's disease also contained higher HCA2 messenger RNA levels that those of individuals who did not have Alzheimer's disease.)[42] In a third study, 5XFAD control mice that had normal levels of HCA2 or had their Hca2 gene knocked out were treated with a FDA-approved formulation of niacin, Niaspan. Niaspan-treated control mice had less brain neuron losses, fewer and smaller brain plaques, and better memory (as measured on a y-maze task test) than mice not treated with Niaspan: Niaspan did not produce these changes in Hca2 gene knockout mice.[43] These results indicate that HCA2 suppresses the progression of Alzheimer's disease in a mouse model and support further studies with the ultimate goal of determining if HCA2 activators would be a useful addition to the treatment of Alzheimer's disease.[13][34][42][43]
Parkinson's disease
Individuals with Parkinson's disease develop progressively less control of their motor movements in association with progressively greater losses of dopamine neurons within the pars compacta subdivision of their brain's substantia nigra. After longer times with the disease, individuals may also develop worsening cognition symptoms and, ultimately, Parkinson's disease dementia.[44] Some studies suggest that HCA2 may act to suppress this disease's progression. In a mouse model of Parkinson's disease, control male mice and Hcar2 gene knockout male mice received lipopolysaccharide (an inflammation-inducing bacterial toxin) injections into the right substantia nigra of their brains and examined 28 days after the injections. Compared to control mice, Hcar2 gene knockout mice evidenced greater injury to their dopamine neurons, severer motor deficits, and more inflammation as judged by the levels of three pro-inflammatory cytokines (i.e., interleukin-6, interleukin-1β, and tumor necrosis factor-α) in their midbrain tissues and serum. Further studies examined mice that had their Hcar2 gene knocked out in their microglia but not in other tissues. Following the lipopolysaccharide injection protocol just described, the mice were feed a niacin solution for 28 days. This regimen alleviated dopamine neuron injuries and motor deficits in control mice but not in mice constructed to have Hcar2 gene knockout microglial cells.[45] In the model of MPTP-induced Parkinson's disease, mice received intraperitoneal injections of MPTP or a placebo (e.g., salt water) daily for 7 days followed by daily feeding (by gavage) of a salt water placebo, butyric acid, or monomethyl fumarate for 14 days. Compared to mice not treated with MPTP, mice treated with MPTP followed by salt water developed defective motor functions as defined in three different tests, lower dopamine levels in their corpus striatum, activation of the microglia in their substantia nigra, and evidence of systemic inflammation (i.e., increased serum levels of the pro-inflammatory cytokines, tumor necrosis factor-α and interleuken-6). Mice treated with MPTP followed by butyric acid or monomethyl fumarate were significantly protected from developing these changes. Further studies suggested that the activation of HCA2 on microglial cells stimulated their change from a pro-inflammatory to anti-inflammatory phenotype.[46] These results indicate that HCA2 suppresses the inflammation, neuronal damage, and neurological symptoms in mouse Parkinson's disease models and suggest that agents activating this receptor may be of use in treating and therefore should be further studied in humans with this disease.[13][45][46]
Multiple sclerosis
Multiple sclerosis is an autoimmune demyelinating disease in which an individual's immune system's causes an inflammation-based destruction of the myelin sheath surrounding neurons in the central nervous system. This disrupts the afflicted neurons' functions and causes various neurological symptoms depending on which neurons are damaged.[13] In a murine experimental autoimmune encephalomyelitis model of multiple sclerosis, mice taking oral dimethyl fumarate had less immune cell infiltration and demyelination in their spinal cords and improved motor function compared to mice not treated with dimethyl fumarate. These dimethyl fumarate-induced improvements did not occur in Hcar2 gene knockout mice.[13][47] Studies in lipopolysaccaride-treated cultured murine microglial cells found that monomethyl fumarate switched the cells from a pro-inflammatory to an anti-inflammatory phenotype. Microglial cells pretreated with an antibody that binds to and thereby blocks activation of HCA2 did not show these phenotypic changes. These studies indicate that HCA2 acts to suppress the inflammation and thereby neurological symptoms in a mouse model of multiple sclerosis. In 2013, the Federal Drug Administration approved dimethyl fumarate (trade name Tecfidera[31]) for the treatment of multiple sclerosis.[5] Although it is now regarded as one of the front-line (i.e. first used) therapies for treating this disease, dimethyl fumarate's mechanism of action, including its impact on HCA2 in human multiple sclerosis, has not yet been defined[31] and needs to be study.[13]
Pathological pain
Pathologic pain is due to the abnormal activation of neurons in pain signaling pathways)[13][48] For example, neurons in the vertebral column's posterior horn of the spinal cord are part of one pain signaling pathway. Excessive activation of these neurons caused by inflammation stimulates the production of pro-inflammatory cytokines (e.g., interleukin-2 and tumor necrosis factor-α) and persistent nociplastic pain.[48] Numerous studies in mice and rats have reported that β-hydroxybutyric acid, dimethyl fumarate, and MK-1903 have analgesic effects in models of thermal and mechanical hypersensitivity due to tibial bone fracture, intervertebral disc degeneration, complete Freund’s adjuvant-induced arthritis, systemic lupus erythematosus, and chronic constriction of the sciatic nerve.[13] In the mouse model of pain induced by chronic constriction of the sciatic nerve, the pain-relieving effects of β-hydroxybutyric acid and dimethyl fumarate did not occur in Hca2 gene knockout mice.[49] These results indicate that HCA2 suppresses various types of pathological pain in mice and support studies to learn if it does so in humans.[13]
Mastitis
Mastitis is an infection-related or sterile inflammation of breast tissue. In a murine model of mastitis, post-pregnant female mice drank niacin-containing or normal water for 26 days and then received lipopolysaccharide injections into the fourth pair of their mammary glands. The next day each mammary gland was examined. Mouse fed pure water had extensive inflammation of their lipopolysaccharide-injected mammary glands, elevated mammary gland levels of pro-inflammatory cytokines (i.e., interleukin-6, interleukin-1β, and tumor necrosis factor-α), severe structural abnormalities such as thickened walls around their breasts' milk-producing alveoli, and breakdown of the blood-milk barrier which prevents uncontrolled exchange of components between the blood and alveolar milk. The mammary glands of lipopolysaccharide-injected, niacin-fed control mice but not niacin-fed Hca2 gene knockout mice had far less of these changes. These results indicate that HCA2 functions to suppress the inflammation and tissue injuries that develop in a mouse model of mastitis.[20] HCA2 may play a similar role in bovines: dairy cows with mastitis that were fed niacin for 7 days showed decreases in their serum and milk levels of pro-inflammatory cytokines (i.e., tumor necrosis factor-α, interleukin-6, and interleukin-1β) and fewer cells in their milk compared to cows with mastitis that were not treated with niacin. It was also noted that the mammary tissue levels of HCA2 were higher in cows with than those without mastitis.[50] Thus, HCA2 may prove to be a target for treating mastitis in cows and might be useful to examine its roles in the in human mastitis.[20][50]
Alcoholic hepatitis
In a model of alcohol-induced hepatitis, β-hydroxybutyric acid-treated mice showed less evidence of liver inflammation compared to control mice as indicated by their: 1) lower plasma levels of alanine transaminase (an enzyme released into the bloodstream by damaged liver cells); 2) less liver steatosis (i.e., lower levels of liver fat); and 3) lower numbers of inflammation-promoting neutrophils, higher numbers of inflammation-suppressing M2 macrophages, and higher levels of messenger RNA encoding an inflammation-suppressing cytokine, IL-10, in their livers. The inflammation-reducing effects of β-hydroxybutyric acid did not occur in Hcar2 gene knockout mice. In human studies, the concentration of β-hydroxybutyric acid in the livers of ten patients with alcoholic hepatitis was significantly lower than that of normal individuals. These findings indicate that HCA2 acts to reduce the severity of alcohol-induced hepatitis in mice and suggest that it may also do so, and therefore should be further studied, in humans.[21]
Inflammatory bowel disease and colon cancer
Inflammatory bowel diseases, i.e., ulcerative colitis and Crohn’s disease, are chronic inflammatory diseases of the gastrointestinal tract that can progress to colon cancer.[22] Colon cancer, even if not preceded by an inflammatory bowel disease, commonly shows the presence of the inflammation response that is mounted to fight invading intestinal microorganisms. In a murine model of colitis, rats were given niacin or water for 2 weeks, given daily rectal injections of the colitis-inducing agent, iodoacetamide, and sacrificed on day 15. Compared to water-treated rats, niacin-treated rats developed milder colitis as defined by less declines in body weight, less declines in colon weights, and less rises in colon tissue levels of myeloperoxidase, an indicator of inflammatory cell (i.e. polymorphonuclear leukocytes) infiltration. In a murine model of colitis leading to colon cancer, mice were treated with dextran sulfate sodium to produce colitis and an intraperitoneal injection of azoxymethane, a colon cancer-causing carcinogen. In this ApcMin/+ murine model: 1) mice fed a diet that greatly reduced the levels of butyric acid in the colon developed colitis and numerous potentially pre-cancerous colon polyps; 2) mice fed a normal diet had less of these changes; and 3) niacin treatment of mice fed the butyric acid-reducing diet suppressed these changes but did not do so in Hcar2 gene knockout mice on the butyric acid-reducing diet.[22] Thus, HCA2 acts to inhibit colitis in rat as well as mouse models of colitis and in the mouse ulcerative colitis model reduced the formation of potentially pre-cancerous polyps.[22] In human studies, the levels of messenger RNA encoding HCA2 in 18 individuals with colon cancer were far lower in their cancers than their normal colon tissues and were also lower in 10 human colon cancer cell lines than 2 human non-cancerous colon cell lines. (HCA3 messenger RNA levels were also lower in the colon cancer than non-cancerous colon tissue of the patients.) Furthermore, individuals who have inflammatory bowel disease and consume a diet that increases their levels of β-hydroxybutyric and butyric acid have been suggested to show clinical improvements in their disease and a reduced rate of it progressing to colon cancer.[26] These findings suggest that human colon cancers not preceded by an inflammatory bowel disease are associated with reductions in the expression of HCA2 (and HCA3) due to gene silencing, that the reductions of HCA2 (and/or HCA3) may be involved in the development and/or progression of these cancers.[51][52] and that HCA2 may act to suppress human ulcerative colitis as well as its progression to colon cancer.[26]
Other diseases
Activators of HCA2 have been shown to suppress the inflammation and severity of disease in two other animal models. However, these studies did not examine Hca2 gene knockout/knockdown animals. These models are for psoriasis[23] and brain tissue inflammation, injury, and behavioral abnormalities caused by alcohol.[24]
References
- GRCh38: Ensembl release 89: ENSG00000182782 - Ensembl, May 2017
- GRCm38: Ensembl release 89: ENSMUSG00000045502 - Ensembl, May 2017
- "Human PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- "Mouse PubMed Reference:". National Center for Biotechnology Information, U.S. National Library of Medicine.
- Offermanns S, Colletti SL, Lovenberg TW, Semple G, Wise A, IJzerman AP (June 2011). "International Union of Basic and Clinical Pharmacology. LXXXII: Nomenclature and Classification of Hydroxy-carboxylic Acid Receptors (GPR81, GPR109A, and GPR109B)". Pharmacological Reviews. 63 (2): 269–90. doi:10.1124/pr.110.003301. PMID 21454438. S2CID 6766923.
- Takeda S, Kadowaki S, Haga T, Takaesu H, Mitaku S (June 2002). "Identification of G protein-coupled receptor genes from the human genome sequence". FEBS Letters. 520 (1–3): 97–101. doi:10.1016/S0014-5793(02)02775-8. PMID 12044878. S2CID 7116392.
- Wise A, Foord SM, Fraser NJ, Barnes AA, Elshourbagy N, Eilert M, Ignar DM, Murdock PR, Steplewski K, Green A, Brown AJ, Dowell SJ, Szekeres PG, Hassall DG, Marshall FH, Wilson S, Pike NB (March 2003). "Molecular identification of high and low affinity receptors for nicotinic acid". The Journal of Biological Chemistry. 278 (11): 9869–74. doi:10.1074/jbc.M210695200. PMID 12522134.
- Soga T, Kamohara M, Takasaki J, Matsumoto S, Saito T, Ohishi T, Hiyama H, Matsuo A, Matsushime H, Furuichi K (March 2003). "Molecular identification of nicotinic acid receptor". Biochemical and Biophysical Research Communications. 303 (1): 364–9. doi:10.1016/S0006-291X(03)00342-5. PMID 12646212.
- "Entrez Gene: GPR109A G protein-coupled receptor 109A".
- S Offermanns, SL Colletti, AP IJzerman, TW Lovenberg, G Semple, A Wise, MG Waters. "Hydroxycarboxylic acid receptors". IUPHAR/BPS Guide to Pharmacology. International Union of Basic and Clinical Pharmacology. Retrieved 13 July 2018.
{{cite web}}: CS1 maint: multiple names: authors list (link) - Ikeda T, Nishida A, Yamano M, Kimura I (November 2022). "Short-chain fatty acid receptors and gut microbiota as therapeutic targets in metabolic, immune, and neurological diseases". Pharmacology & Therapeutics. 239: 108273. doi:10.1016/j.pharmthera.2022.108273. PMID 36057320. S2CID 251992642.
- Miyamoto J, Ohue-Kitano R, Mukouyama H, Nishida A, Watanabe K, Igarashi M, Irie J, Tsujimoto G, Satoh-Asahara N, Itoh H, Kimura I (November 2019). "Ketone body receptor GPR43 regulates lipid metabolism under ketogenic conditions". Proceedings of the National Academy of Sciences of the United States of America. 116 (47): 23813–23821. Bibcode:2019PNAS..11623813M. doi:10.1073/pnas.1912573116. PMC 6876247. PMID 31685604.
- Taing K, Chen L, Weng HR (April 2023). "Emerging roles of GPR109A in regulation of neuroinflammation in neurological diseases and pain". Neural Regeneration Research. 18 (4): 763–768. doi:10.4103/1673-5374.354514. PMC 9700108. PMID 36204834.
- Milligan G, Barki N, Tobin AB (March 2021). "Chemogenetic Approaches to Explore the Functions of Free Fatty Acid Receptor 2" (PDF). Trends in Pharmacological Sciences. 42 (3): 191–202. doi:10.1016/j.tips.2020.12.003. PMID 33495026. S2CID 231712546.
- Bourassa MW, Alim I, Bultman SJ, Ratan RR (June 2016). "Butyrate, neuroepigenetics and the gut microbiome: Can a high fiber diet improve brain health?". Neuroscience Letters. 625: 56–63. doi:10.1016/j.neulet.2016.02.009. PMC 4903954. PMID 26868600.
- Spigoni V, Cinquegrani G, Iannozzi NT, Frigeri G, Maggiolo G, Maggi M, Parello V, Dei Cas A (2022). "Activation of G protein-coupled receptors by ketone bodies: Clinical implication of the ketogenic diet in metabolic disorders". Frontiers in Endocrinology. 13: 972890. doi:10.3389/fendo.2022.972890. PMC 9631778. PMID 36339405.
- Graff EC, Fang H, Wanders D, Judd RL (February 2016). "Anti-inflammatory effects of the hydroxycarboxylic acid receptor 2". Metabolism: Clinical and Experimental. 65 (2): 102–13. doi:10.1016/j.metabol.2015.10.001. PMID 26773933.
- Tan JK, McKenzie C, Mariño E, Macia L, Mackay CR (April 2017). "Metabolite-Sensing G Protein-Coupled Receptors-Facilitators of Diet-Related Immune Regulation". Annual Review of Immunology. 35: 371–402. doi:10.1146/annurev-immunol-051116-052235. PMID 28446062.
- Kaye DM, Shihata WA, Jama HA, Tsyganov K, Ziemann M, Kiriazis H, Horlock D, Vijay A, Giam B, Vinh A, Johnson C, Fiedler A, Donner D, Snelson M, Coughlan MT, Phillips S, Du XJ, El-Osta A, Drummond G, Lambert GW, Spector TD, Valdes AM, Mackay CR, Marques FZ (April 2020). "Deficiency of Prebiotic Fiber and Insufficient Signaling Through Gut Metabolite-Sensing Receptors Leads to Cardiovascular Disease". Circulation. 141 (17): 1393–1403. doi:10.1161/CIRCULATIONAHA.119.043081. PMID 32093510. S2CID 211476145.
- Guo W, Li W, Su Y, Liu S, Kan X, Ran X, Cao Y, Fu S, Liu J (2021). "GPR109A alleviate mastitis and enhances the blood milk barrier by activating AMPK/Nrf2 and autophagy". International Journal of Biological Sciences. 17 (15): 4271–4284. doi:10.7150/ijbs.62380. PMC 8579459. PMID 34803497.
- Chen Y, Ouyang X, Hoque R, Garcia-Martinez I, Yousaf MN, Tonack S, Offermanns S, Dubuquoy L, Louvet A, Mathurin P, Massey V, Schnabl B, Bataller RA, Mehal WZ (September 2018). "β-Hydroxybutyrate protects from alcohol-induced liver injury via a Hcar2-cAMP dependent pathway". Journal of Hepatology. 69 (3): 687–696. doi:10.1016/j.jhep.2018.04.004. PMC 6098974. PMID 29705237.
- Singh N, Gurav A, Sivaprakasam S, Brady E, Padia R, Shi H, Thangaraju M, Prasad PD, Manicassamy S, Munn DH, Lee JR, Offermanns S, Ganapathy V (January 2014). "Activation of Gpr109a, receptor for niacin and the commensal metabolite butyrate, suppresses colonic inflammation and carcinogenesis". Immunity. 40 (1): 128–39. doi:10.1016/j.immuni.2013.12.007. PMC 4305274. PMID 24412617.
- Straß S, Geiger J, Cloos N, Späth N, Geiger S, Schwamborn A, De Oliveira da Cunha L, Martorelli M, Guse JH, Sandri TL, Burnet M, Laufer S (June 2023). "Immune cell targeted fumaric esters support a role of GPR109A as a primary target of monomethyl fumarate in vivo". Inflammopharmacology. 31 (3): 1223–1239. doi:10.1007/s10787-023-01186-0. PMID 37004600. S2CID 257912134.
- Wei H, Yu C, Zhang C, Ren Y, Guo L, Wang T, Chen F, Li Y, Zhang X, Wang H, Liu J (April 2023). "Butyrate ameliorates chronic alcoholic central nervous damage by suppressing microglia-mediated neuroinflammation and modulating the microbiome-gut-brain axis". Biomedicine & Pharmacotherapy = Biomedecine & Pharmacotherapie. 160: 114308. doi:10.1016/j.biopha.2023.114308. PMID 36709599. S2CID 256383935.
- Adepu KK, Kachhap S, Bhandari D, Anishkin A, Chintapalli SV (July 2022). "Computational insights on molecular interactions of acifran with GPR109A and GPR109B". Journal of Molecular Modeling. 28 (8): 237. doi:10.1007/s00894-022-05233-5. PMID 35900600. S2CID 251108717.
- Carretta MD, Quiroga J, López R, Hidalgo MA, Burgos RA (2021). "Participation of Short-Chain Fatty Acids and Their Receptors in Gut Inflammation and Colon Cancer". Frontiers in Physiology. 12: 662739. doi:10.3389/fphys.2021.662739. PMC 8060628. PMID 33897470.
- Offermanns S (March 2017). "Hydroxy-Carboxylic Acid Receptor Actions in Metabolism". Trends in Endocrinology and Metabolism: TEM. 28 (3): 227–236. doi:10.1016/j.tem.2016.11.007. PMID 28087125. S2CID 39660018.
- Xu J, Moore BN, Pluznick JL (October 2022). "Short-Chain Fatty Acid Receptors and Blood Pressure Regulation: Council on Hypertension Mid-Career Award for Research Excellence 2021". Hypertension. 79 (10): 2127–2137. doi:10.1161/HYPERTENSIONAHA.122.18558. PMC 9458621. PMID 35912645.
- Abdelrahman AA, Powell FL, Jadeja RN, Jones MA, Thounaojam MC, Bartoli M, Al-Shabrawey M, Martin PM (August 2022). "Expression and activation of the ketone body receptor HCAR2/GPR109A promotes preservation of retinal endothelial cell barrier function". Experimental Eye Research. 221: 109129. doi:10.1016/j.exer.2022.109129. PMID 35649469. S2CID 249186172.
- Gambhir D, Ananth S, Veeranan-Karmegam R, Elangovan S, Hester S, Jennings E, Offermanns S, Nussbaum JJ, Smith SB, Thangaraju M, Ganapathy V, Martin PM (April 2012). "GPR109A as an anti-inflammatory receptor in retinal pigment epithelial cells and its relevance to diabetic retinopathy". Investigative Ophthalmology & Visual Science. 53 (4): 2208–17. doi:10.1167/iovs.11-8447. PMC 4627510. PMID 22427566.
- Majkutewicz I (July 2022). "Dimethyl fumarate: A review of preclinical efficacy in models of neurodegenerative diseases". European Journal of Pharmacology. 926: 175025. doi:10.1016/j.ejphar.2022.175025. PMID 35569547. S2CID 248784399.
- von Glehn F, Dias-Carneiro RP, Moraes AS, Farias AS, Silva VA, Oliveira FT, Silva CE, de Carvalho F, Rahal E, Baecher-Allan C, Santos LM (July 2018). "Dimethyl fumarate downregulates the immune response through the HCA2/GPR109A pathway: Implications for the treatment of multiple sclerosis". Multiple Sclerosis and Related Disorders. 23: 46–50. doi:10.1016/j.msard.2018.04.016. PMID 29763776. S2CID 21697608.
- Shen HC, Ding FX, Raghavan S, Deng Q, Luell S, Forrest MJ, Carballo-Jane E, Wilsie LC, Krsmanovic ML, Taggart AK, Wu KK, Wu TJ, Cheng K, Ren N, Cai TQ, Chen Q, Wang J, Wolff MS, Tong X, Holt TG, Waters MG, Hammond ML, Tata JR, Colletti SL (March 2010). "Discovery of a biaryl cyclohexene carboxylic acid (MK-6892): a potent and selective high affinity niacin receptor full agonist with reduced flushing profiles in animals as a preclinical candidate". Journal of Medicinal Chemistry. 53 (6): 2666–70. doi:10.1021/jm100022r. PMID 20184326.
- Boatman PD, Lauring B, Schrader TO, Kasem M, Johnson BR, Skinner P, Jung JK, Xu J, Cherrier MC, Webb PJ, Semple G, Sage CR, Knudsen J, Chen R, Luo WL, Caro L, Cote J, Lai E, Wagner J, Taggart AK, Carballo-Jane E, Hammond M, Colletti SL, Tata JR, Connolly DT, Waters MG, Richman JG (April 2012). "(1aR,5aR)1a,3,5,5a-Tetrahydro-1H-2,3-diaza-cyclopropa[a]pentalene-4-carboxylic acid (MK-1903): a potent GPR109a agonist that lowers free fatty acids in humans". Journal of Medicinal Chemistry. 55 (8): 3644–66. doi:10.1021/jm2010964. PMID 22435740.
- Dobbins RL, Shearn SP, Byerly RL, Gao FF, Mahar KM, Napolitano A, Nachbaur GJ, Le Monnier de Gouville AC (November 2013). "GSK256073, a selective agonist of G-protein coupled receptor 109A (GPR109A) reduces serum glucose in subjects with type 2 diabetes mellitus". Diabetes, Obesity & Metabolism. 15 (11): 1013–21. doi:10.1111/dom.12132. PMID 23701262. S2CID 40695967.
- Jiang Y, Jin M, Chen J, Yan J, Liu P, Yao M, Cai W, Pi R (February 2020). "Discovery of a novel niacin-lipoic acid dimer N2L attenuating atherosclerosis and dyslipidemia with non-flushing effects". European Journal of Pharmacology. 868: 172871. doi:10.1016/j.ejphar.2019.172871. PMID 31846627. S2CID 209409535.
- Plaisance EP, Lukasova M, Offermanns S, Zhang Y, Cao G, Judd RL (March 2009). "Niacin stimulates adiponectin secretion through the GPR109A receptor". American Journal of Physiology. Endocrinology and Metabolism. 296 (3): E549–58. doi:10.1152/ajpendo.91004.2008. PMID 19141678.
- Lauring B, Taggart AK, Tata JR, Dunbar R, Caro L, Cheng K, Chin J, Colletti SL, Cote J, Khalilieh S, Liu J, Luo WL, Maclean AA, Peterson LB, Polis AB, Sirah W, Wu TJ, Liu X, Jin L, Wu K, Boatman PD, Semple G, Behan DP, Connolly DT, Lai E, Wagner JA, Wright SD, Cuffie C, Mitchel YB, Rader DJ, Paolini JF, Waters MG, Plump A (August 2012). "Niacin lipid efficacy is independent of both the niacin receptor GPR109A and free fatty acid suppression". Science Translational Medicine. 4 (148): 148ra115. doi:10.1126/scitranslmed.3003877. PMID 22914621. S2CID 37941204.
- Zhang SJ, Li ZH, Zhang YD, Chen J, Li Y, Wu FQ, Wang W, Cui ZJ, Chen GQ (May 2021). "Ketone Body 3-Hydroxybutyrate Ameliorates Atherosclerosis via Receptor Gpr109a-Mediated Calcium Influx". Advanced Science (Weinheim, Baden-Wurttemberg, Germany). 8 (9): 2003410. doi:10.1002/advs.202003410. PMC 8097358. PMID 33977048.
- Rahman M, Muhammad S, Khan MA, Chen H, Ridder DA, Müller-Fielitz H, Pokorná B, Vollbrandt T, Stölting I, Nadrowitz R, Okun JG, Offermanns S, Schwaninger M (May 2014). "The β-hydroxybutyrate receptor HCA2 activates a neuroprotective subset of macrophages". Nature Communications. 5: 3944. Bibcode:2014NatCo...5.3944R. doi:10.1038/ncomms4944. PMID 24845831. S2CID 38472700.
- Kong D, Yu Y (June 2022). "Prostaglandin D2 signaling and cardiovascular homeostasis". Journal of Molecular and Cellular Cardiology. 167: 97–105. doi:10.1016/j.yjmcc.2022.03.011. PMID 35367459. S2CID 247894789.
- Wu Y, Gong Y, Luan Y, Li Y, Liu J, Yue Z, Yuan B, Sun J, Xie C, Li L, Zhen J, Jin X, Zheng Y, Wang X, Xie L, Wang W (January 2020). "BHBA treatment improves cognitive function by targeting pleiotropic mechanisms in transgenic mouse model of Alzheimer's disease". FASEB Journal. 34 (1): 1412–1429. doi:10.1096/fj.201901984R. PMID 31914599. S2CID 210120960.
- Moutinho M, Puntambekar SS, Tsai AP, Coronel I, Lin PB, Casali BT, Martinez P, Oblak AL, Lasagna-Reeves CA, Lamb BT, Landreth GE (March 2022). "The niacin receptor HCAR2 modulates microglial response and limits disease progression in a mouse model of Alzheimer's disease". Science Translational Medicine. 14 (637): eabl7634. doi:10.1126/scitranslmed.abl7634. PMC 10161396. PMID 35320002.
- Bjørklund G, Dadar M, Anderson G, Chirumbolo S, Maes M (November 2020). "Preventive treatments to slow substantia nigra damage and Parkinson's disease progression: A critical perspective review". Pharmacological Research. 161: 105065. doi:10.1016/j.phrs.2020.105065. PMID 32652199. S2CID 220487717.
- He D, Fu S, Ye B, Wang H, He Y, Li Z, Li J, Gao X, Liu D (March 2023). "Activation of HCA2 regulates microglial responses to alleviate neurodegeneration in LPS-induced in vivo and in vitro models". Journal of Neuroinflammation. 20 (1): 86. doi:10.1186/s12974-023-02762-5. PMC 10053461. PMID 36991440.
- Xu RC, Miao WT, Xu JY, Xu WX, Liu MR, Ding ST, Jian YX, Lei YH, Yan N, Liu HD (October 2022). "Neuroprotective Effects of Sodium Butyrate and Monomethyl Fumarate Treatment through GPR109A Modulation and Intestinal Barrier Restoration on PD Mice". Nutrients. 14 (19): 4163. doi:10.3390/nu14194163. PMC 9571500. PMID 36235813.
- Chen H, Assmann JC, Krenz A, Rahman M, Grimm M, Karsten CM, Köhl J, Offermanns S, Wettschureck N, Schwaninger M (May 2014). "Hydroxycarboxylic acid receptor 2 mediates dimethyl fumarate's protective effect in EAE". The Journal of Clinical Investigation. 124 (5): 2188–92. doi:10.1172/JCI72151. PMC 4001545. PMID 24691444.
- Viswanath O, Urits I, Burns J, Charipova K, Gress K, McNally A, Urman RD, Welschmeyer A, Berger AA, Kassem H, Sanchez MG, Kaye AD, Eubanks TN, Cornett EM, Ngo AL (May 2020). "Central Neuropathic Mechanisms in Pain Signaling Pathways: Current Evidence and Recommendations". Advances in Therapy. 37 (5): 1946–1959. doi:10.1007/s12325-020-01334-w. PMC 7467462. PMID 32291648.
- Boccella S, Guida F, De Logu F, De Gregorio D, Mazzitelli M, Belardo C, Iannotta M, Serra N, Nassini R, de Novellis V, Geppetti P, Maione S, Luongo L (January 2019). "Ketones and pain: unexplored role of hydroxyl carboxylic acid receptor type 2 in the pathophysiology of neuropathic pain". FASEB Journal. 33 (1): 1062–1073. doi:10.1096/fj.201801033R. PMID 30085883. S2CID 51937093.
- Guo W, Liu J, Li W, Ma H, Gong Q, Kan X, Cao Y, Wang J, Fu S (May 2020). "Niacin Alleviates Dairy Cow Mastitis by Regulating the GPR109A/AMPK/NRF2 Signaling Pathway". International Journal of Molecular Sciences. 21 (9): 3321. doi:10.3390/ijms21093321. PMC 7246865. PMID 32397071.
- Thangaraju M, Cresci GA, Liu K, Ananth S, Gnanaprakasam JP, Browning DD, Mellinger JD, Smith SB, Digby GJ, Lambert NA, Prasad PD, Ganapathy V (April 2009). "GPR109A is a G-protein-coupled receptor for the bacterial fermentation product butyrate and functions as a tumor suppressor in colon". Cancer Research. 69 (7): 2826–32. doi:10.1158/0008-5472.CAN-08-4466. PMC 3747834. PMID 19276343.
- Moniri NH, Farah Q (April 2021). "Short-chain free-fatty acid G protein-coupled receptors in colon cancer". Biochemical Pharmacology. 186: 114483. doi:10.1016/j.bcp.2021.114483. PMID 33631190. S2CID 232057114.