Fetal-maternal haemorrhage
Fetal-maternal haemorrhage is the loss of fetal blood cells into the maternal circulation. It takes place in normal pregnancies as well as when there are obstetric or trauma related complications to pregnancy.
| Fetal-maternal haemorrhage | |
|---|---|
| Specialty | Obstetrics |
Normally the maternal circulation and the fetal circulation are kept from direct contact with each other, with gas and nutrient exchange taking place across a membrane in the placenta made of two layers, the syncytiotrophoblast and the cytotrophoblast. Fetal-maternal haemorrhage occurs when this membrane ceases to function as a barrier and fetal cells may come in contact with and enter the maternal vessels in the decidua/endometrium.
Description
Normal pregnancy
It is estimated that less than 1ml of fetal blood is lost to the maternal circulation during normal labour in around 96% of normal deliveries.[1][2] The loss of this small amount of blood may however be a sensitising event and stimulate antibody production to the foetal red blood cells, an example of which is Rhesus disease of the newborn.
Abnormal pregnancy
Causes of increased foetal-maternal haemorrhage are seen as a result of trauma, placental abruption or may be spontaneous with no cause found.
Up to 30ml of foetal-maternal transfusion may take place with no significant signs or symptoms seen in either mother or foetus.[3] Loss in excess of this may result in significant morbidity and mortality to the fetus. Fetal-maternal haemorrhage is one cause of intrauterine death (IUD).
Diagnosis
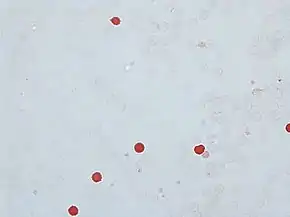
The Kleihauer–Betke test is a blood test used to measure the amount of foetal hemoglobin transferred from a foetus to its mother's bloodstream.[4] It takes advantage of the differential resistance of foetal hemoglobin to acid. A standard blood smear is prepared from the mother's blood, and exposed to an acid bath. This removes adult hemoglobin, but not foetal hemoglobin, from the red blood cells. Subsequent staining, using Shepard's method,[5] makes fetal cells (containing foetal hemoglobin) appear rose-pink in color, while adult red blood cells are only seen as "ghosts". 2000 cells are counted under the microscope and a percentage of foetal to maternal cells is calculated.
Fetal-maternal haemorrhage can also be diagnosed by flow cytometry, using anti-foetal hemoglobin antibodies (anti-HbF).[6]
Treatment
If ongoing and rapid haemorrhage is occurring then immediate delivery of the foetus may be indicated if the fetus is sufficiently developed.[7] If the haemorrhage has already occurred and now stopped, an inutero transfusion of red cells to the foetus may be recommended.[8]
References
- Sebring ES, Polesky HF. Fetomaternal Hemorrhage: Incidence, risk factors, time of occurrence, and clinical effects" Transfusion 1990; 30:344-357.
- Medearis AL, Hensleigh Pa, Parks DR, Herzenberh LA. Detection of foetal erythrocytes in maternal blood post partum with the fluorescence-activated cell sorter. American Journal of Obstetrics and Gynaecology 1984; 48:290-295.
- Polesky HF Sebring ES. Evaluation of methods of detection and quantitation of fetal cells and their effects on Rh Ig usage. American Journal of Clinical Pathology 198 1; 76(suppl):525-529.
- Katiyar R, Kriplani A, Agarwal N, Bhatla N, Kabra M (2007). "Detection of fetomaternal hemorrhage following chorionic villus sampling by Kleihauer–Betke test and rise in maternal serum alpha feto protein". Prenat. Diagn. 27 (2): 139–42. doi:10.1002/pd.1632. PMID 17191260. S2CID 36617092.
- Alcoholic haematoxylin, acidified ferric chloride, Shepard's counterstain. Shepard's Fixative/Diluent
- Kim, Yeowon A.; Makar, Robert S. (2012). "Detection of fetomaternal hemorrhage". American Journal of Hematology. 87 (4): 417–423. doi:10.1002/ajh.22255. ISSN 0361-8609. PMID 22231030.
- Massive fetomaternal hemorrhage and oxytocin contraction test: case report and review Arch Gynecol Obstet. 2004 Jan;269 (2):149-51 14648183 (P, S, G, E, B)
- Massive fetomaternal hemorrhage and oxytocin contraction test: case report and review Arch Gynecol Obstet. 2004 Jan; 269 (2):149-51 14648183 (P, S, G, E, B)