Scintillating scotoma
Scintillating scotoma is a common visual aura that was first described by 19th-century physician Hubert Airy (1838–1903). Originating from the brain, it may precede a migraine headache, but can also occur acephalgically (without headache), also known as visual migraine or migraine aura.[4] It is often confused with retinal migraine, which originates in the eyeball or socket.
| Scintillating scotoma | |
|---|---|
| Other names | Visual migraine[1] Teichopsia[2] |
 | |
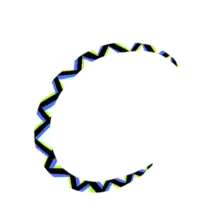
| Example of a scintillating scotoma, as may be caused by cortical spreading depression | |
| Specialty | Neurology, Neuro-ophthalmology |
| Symptoms | Aura in vision, nausea, dizziness, brain fog |
| Complications | Migraine onset |
| Duration | Less than 60 minutes[3] |
| Causes | Cortical spreading depression |
| Risk factors | Migraine sufferer |
| Differential diagnosis | Persistent aura without infarction, Retinal migraine |
| Prevention | Avoiding migraine triggers |
| Prognosis | Self-limiting |
Signs and symptoms

Many variations occur, but scintillating scotoma usually begins as a spot of flickering light near or in the center of the visual field, which prevents vision within the scotoma area. It typically affects both eyes, as it is not a problem specific to one eye. The affected area flickers but is not dark. It then gradually expands outward from the initial spot. Vision remains normal beyond the borders of the expanding scotoma(s), with objects melting into the scotoma area background similarly to the physiological blind spot, which means that objects may be seen better by not looking directly at them in the early stages when the spot is in or near the center. The scotoma area may expand to occupy one half of the visual area of one eye, or it may be bilateral. It may occur as an isolated symptom without headache in acephalgic migraine.

As the scotoma area expands, some people perceive only a bright flickering area that obstructs normal vision, while others describe seeing various patterns. Some describe seeing one or more shimmering arcs of white or colored flashing lights. An arc of light may gradually enlarge, become more obvious, and may take the form of a definite zigzag pattern, sometimes called a fortification spectrum (i.e. teichopsia, from Greek τεῖχος, town wall), because of its resemblance to the fortifications of a castle or fort seen from above.[3] It also can resemble the dazzle camouflage patterns used on ships in World War I. Others describe patterns within the arc as resembling herringbone or Widmanstätten patterns.
The visual anomaly results from abnormal functioning of portions of the occipital cortex at the back of the brain, not in the eyes nor any component thereof, such as the retinas.[5] This is a different disease from retinal migraine, which is monocular (only one eye).[6]
It may be difficult to read and dangerous to drive a vehicle while the scotoma is present. Normal central vision may return several minutes before the scotoma disappears from peripheral vision.
Sufferers can keep a diary of dates on which the episodes occur to show to their physician, plus a small sketch of the anomaly, which may vary between episodes.
Animated depictions
 Flickering animation of a scintillating scotoma, where the scintillations were of a zigzag pattern starting in the center of vision, surrounded by a somewhat larger scotoma area with distortion of shapes but otherwise melting into the background similarly to the physiological blind spot.
Flickering animation of a scintillating scotoma, where the scintillations were of a zigzag pattern starting in the center of vision, surrounded by a somewhat larger scotoma area with distortion of shapes but otherwise melting into the background similarly to the physiological blind spot. A depiction of a scintillating scotoma that was almost spiral-shaped, with distortion of shapes but otherwise melting into the background similarly to the physiological blind spot. This depiction shows the type of patterning that some have described as similar to Widmanstätten patterns.
A depiction of a scintillating scotoma that was almost spiral-shaped, with distortion of shapes but otherwise melting into the background similarly to the physiological blind spot. This depiction shows the type of patterning that some have described as similar to Widmanstätten patterns. A depiction of a scintillating scotoma that was almost spiral-shaped, with distortion of shapes but otherwise melting into the background similarly to the physiological blind spot.
A depiction of a scintillating scotoma that was almost spiral-shaped, with distortion of shapes but otherwise melting into the background similarly to the physiological blind spot.
Causes
Scintillating scotomas are most commonly caused by cortical spreading depression, a pattern of changes in the behavior of nerves in the brain during a migraine. Migraines, in turn, may be caused by genetic influences and hormones. People with migraines often self-report triggers for migraines involving stress or foods,[7] or bright lights.[8] While monosodium glutamate (MSG) is frequently reported as a dietary trigger,[9] other scientific studies do not support this claim.[10]
The Framingham Heart Study, published in 1998, surveyed 5,070 people between ages 30 and 62 and found that scintillating scotomas without other symptoms occurred in 1.23% of the group. The study did not find a link between late-life onset scintillating scotoma and stroke.[11]
Prognosis
Symptoms typically appear gradually over 5 to 20 minutes and generally last less than 60 minutes, leading to the headache in classic migraine with aura, or resolving without consequence in acephalgic migraine.[3] For many sufferers, scintillating scotoma is first experienced as a prodrome to migraine, then without migraine later in life. Typically the scotoma resolves spontaneously within the stated time frame, leaving no subsequent symptoms, though some report fatigue, nausea, and dizziness as sequelae.[12]
Names and etymology
The British physician John Fothergill described the condition in the 18th century and called it fortification spectrum.[13] The British physician Hubert Airy coined the term scintillating scotoma for it by 1870; he derived it from the Latin scintilla "spark" and the Ancient Greek skotos "darkness".[14] Other terms for the condition include flittering scotoma, fortification figure, fortification of Vauban, geometrical spectrum, herringbone, Norman arch, teichopsia,[15] and teleopsia.[13]
See also
- Anomalous experiences
- Phosphene – Visual illusion
References
- Prasad, Sashank. "Visual Migraine" (PDF). Brigham and Women's Hospital. Harvard Medical School. Archived from the original (PDF) on 18 March 2015. Retrieved 4 October 2016.
- teichopsia. 2010. doi:10.1093/acref/9780199557141.001.0001. ISBN 9780199557141. Retrieved 15 December 2020 – via oxfordreference.com.
{{cite encyclopedia}}:|work=ignored (help) - "imigraine.net". Retrieved 24 June 2015.
- Lee, Ann (11 July 2022). "'It starts as a line of light, then works its way across my vision': the disorienting mystery of migraine auras". The Guardian.
- "imigraine.net". Archived from the original on 19 July 2009. Retrieved 24 June 2015.
- Grosberg, Brian M.; Solomon, Seymour; Lipton, Richard B. (2005). "Retinal migraine". Current Pain and Headache Reports. 9 (4): 268–271. doi:10.1007/s11916-005-0035-2. PMID 16004843. S2CID 22376278.
- Scott, Paul M. "Scintillating Scotoma (Migraine Scotoma)". Retrieved 22 June 2020. Alternate version: "Scintillating Scotoma (Migraine Scotoma)". Archived from the original on 20 October 2012.
- Newman, Lawrence C. (19 July 2017). "Loud Noises, Bright Lights, and Migraines". WebMD. Retrieved 22 June 2020.
- Sun-Edelstein C, Mauskop A (June 2009). "Foods and supplements in the management of migraine headaches". The Clinical Journal of Pain. 25 (5): 446–52. CiteSeerX 10.1.1.530.1223. doi:10.1097/AJP.0b013e31819a6f65. PMID 19454881. S2CID 3042635.
- Freeman M (October 2006). "Reconsidering the effects of monosodium glutamate: a literature review". Journal of the American Academy of Nurse Practitioners. 18 (10): 482–6. doi:10.1111/j.1745-7599.2006.00160.x. PMID 16999713. S2CID 21084909.
- Christine A. C. Wijman; Philip A. Wolf; Carlos S. Kase; Margaret Kelly-Hayes; Alexa S. Beiser (August 1998). "Migrainous Visual Accompaniments Are Not Rare in Late Life: the Framingham Study". Stroke. 29 (8): 1539–1543. doi:10.1161/01.STR.29.8.1539. PMID 9707189.
- Ekbom, Karl (July 1974). "Migraine in Patients with Cluster Headache". Headache: The Journal of Head and Face Pain. 14 (2): 69–72. doi:10.1111/j.1526-4610.1974.hed1402069.x. PMID 4853218. S2CID 29918087.
- Blom 2009, p. 199.
- Blom 2009, p. 464.
- Blom 2009, pp. 463–464.
Works cited
- Gardner-Medwin AR (December 1981). "Possible roles of vertebrate neuroglia in potassium dynamics, spreading depression and migraine". J. Exp. Biol. 95: 111–27. doi:10.1242/jeb.95.1.111. PMID 7334315.
- Hadjikhani N, Sanchez Del Rio M, Wu O, et al. (10 April 2001). "Mechanisms of migraine aura revealed by functional MRI in human visual cortex". Proc. Natl. Acad. Sci. U.S.A. 98 (8): 4687–4692. Bibcode:2001PNAS...98.4687H. doi:10.1073/pnas.071582498. PMC 31895. PMID 11287655.
- Blom, Jan Dirk, ed. (2009). A Dictionary of Hallucinations. Springer Science & Business Media. ISBN 978-1-4419-1223-7.