MRI contrast agent
MRI contrast agents are contrast agents used to improve the visibility of internal body structures in magnetic resonance imaging (MRI).[1] The most commonly used compounds for contrast enhancement are gadolinium-based contrast agents (GBCAs). Such MRI contrast agents shorten the relaxation times of nuclei within body tissues following oral or intravenous administration.
Theory of operation
In MRI scanners, sections of the body are exposed to a strong magnetic field causing primarily the hydrogen nuclei ("spins") of water in tissues to be polarized in the direction of the magnetic field. An intense radiofrequency pulse is applied that tips the magnetization generated by the hydrogen nuclei in the direction of the receiver coil where the spin polarization can be detected. Random molecular rotational oscillations matching the resonance frequency of the nuclear spins provide the "relaxation" mechanisms that bring the net magnetization back to its equilibrium position in alignment with the applied magnetic field. The magnitude of the spin polarization detected by the receiver is used to form the MR image but decays with a characteristic time constant known as the T1 relaxation time. Water protons in different tissues have different T1 values, which is one of the main sources of contrast in MR images. A contrast agent usually shortens, but in some instances increases, the value of T1 of nearby water protons thereby altering the contrast in the image.
Most clinically used MRI contrast agents work by shortening the T1 relaxation time of protons inside tissues via interactions with the nearby contrast agent. Thermally driven motion of the strongly paramagnetic metal ions in the contrast agent generate the oscillating magnetic fields that provide the relaxation mechanisms that enhance the rate of decay of the induced polarization. The systematic sampling of this polarization over the spatial region of the tissue being examined forms the basis for construction of the image.
MRI contrast agents may be administered by injection into the blood stream or orally, depending on the subject of interest. Oral administration is well suited to G.I. tract scans, while intravascular administration proves more useful for most other scans.
MRI contrast agents can be classified[2] by their:
- chemical composition
- administration route
- magnetic properties
- biodistribution and applications:
- Extracellular fluid agents (intravenous contrast agents)
- Blood pool agents (intravascular contrast agents)
- Organ specific agents (gastrointestinal contrast agents and hepatobiliary contrast agents)
- Active targeting/cell labeling agents (tumor-specific agents)
- Responsive (smart or bioactivated) agents
- pH-sensitive agents
Gadolinium(III)
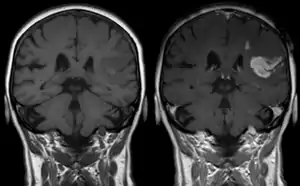
Gadolinium(III) containing MRI contrast agents (often termed simply "gado" or "gad") are the most commonly used for enhancement of vessels in MR angiography or for brain tumor enhancement associated with the degradation of the blood–brain barrier (BBB).[3][4] Over 450 million doses have been administered worldwide from 1988 to 2017.[5] For large vessels such as the aorta and its branches, the dose can be as low as 0.1 mmol / kg of body mass. Higher concentrations are often used for finer vasculature.[6] At much higher concentration, there is more T2 shortening effect of gadolinium, causing gadolinium brightness to be less than surrounding body tissues.[7] However at such concentration, it will cause greater toxicity to bodily tissues.[8]
Gd3+ chelates are hydrophilic and do not readily cross the intact blood–brain barrier. Thus, they are useful in enhancing lesions and tumors where the blood–brain barrier is compromised and the Gd(III) leaks out.[9][lower-alpha 1] In the rest of the body, the Gd3+ initially remains in the circulation but then distributes into the interstitial space or is eliminated by the kidneys.
Available Gadolinium-based contrast agents (GBCAs) (brand names, approved for human use by EMA[10] and by the FDA in 1988.[11][12] (standard dose[13])):
Extracellular fluid agents
- Macrocyclic
- ionic
- gadoterate (Dotarem, Clariscan) : EMA, FDA (SD: 0.1 mmol / kg)[14]
- non-ionic
- gadobutrol (Gadovist [EU] / Gadavist [US]) EMA, FDA (SD: 0.1 mmol / kg)[14]
- gadoteridol (ProHance) : EMA, FDA (SD: 0.1 mmol / kg)[14]
- gadopiclenol (Elucirem, Vueway) : FDA (SD: 0.05 mmol / kg)[15]
- ionic
- Linear (suspended by EMA[16])
- ionic
- gadopentetate (Magnevist, EU: Magnegita, Gado-MRT ratiopharm) FDA (SD: 0.1 mmol / kg)[14]
- gadobenate (MultiHance) : FDA, EMA (liver) (SD: 0.1 mmol / kg)[14]
- gadopentetic acid dimeglumine (Magnetol)[14]
- gadoxentate (Eovist, EU: Primovist) FDA[14]
- non-ionic
- gadoversetamide (OptiMARK) FDA (SD: 0.1 mmol / kg)[14]
- gadodiamide (Omniscan) : FDA (SD: 0.1 mmol / kg)[14]
- ionic
Blood pool agents
- Albumin-binding gadolinium complexes
- gadofosveset (Ablavar, formerly Vasovist) FDA (SD: 0.1 mmol / kg)
- gadocoletic acid
- Polymeric gadolinium complexes
- gadomelitol
- gadomer 17
Hepatobiliary (liver) agents
- gadoxetic acid (Primovist [EU] / Eovist [US]) is used as a hepatobiliary agent as 50% is taken up and excreted by the liver and 50% by the kidneys.
Safety
As a free solubilized aqueous ion, gadolinium(III) is highly toxic, but chelated compound are generally regarded as safe enough to be administered. Free Gd3+ has a median lethal dose of 0.34 mmol / kg (IV, mouse)[17] or 100–200 mg / kg, but the LD50 is increased by a factor of 31 times[18] when Gd3+ is chelated.[19]
The spectrum of adverse drug reactions is greater with gadolinium-based contrast agents than with iodinated contrast agents (Radiocontrast agents).[20]
The use of Gd3+ chelates in persons with acute or chronic kidney disease can cause nephrogenic systemic fibrosis (NSF),[21][22][23] a rare but severe systemic disease resembling scleromyxedema and to some extent scleroderma. It may occur months after contrast injection.[24] Patients with deteriorated kidney function are more at risk for NSF, with dialysis patients being more at risk than patients with chronic kidney disease.[25][26] NSF can be caused by linear and macrocyclic[27][28] (macrocyclic ionic compounds have been found the least likely to release the Gd3+),[29][21] gadolinium-containing MRI contrast agents although much more frequently by linear.
Gadolinium has been found to remain in the brain, heart muscle, kidney, liver, and other organs after one or more injections of a linear or macrocyclic gadolinium-based contrast agents, even after a prolonged period of time.[30][31] The amount differs with the presence of kidney injury at the moment of injection, the molecular geometry of the ligand, and the dose administered.
While NSF is a severe form of disease, gadolinium deposition disease (GDD) is a mild variant with pain (e.g. headache), fatique, and / or gadolinium depositions.[32]
In vitro studies have found gadolinium-based contrast agents to be neurotoxic,[33] and a study found signal intensity in the dentate nucleus of MRI (indicative of gadolinium deposition) to be correlated with lower verbal fluency.[34] Confusion is often reported as a possible clinical symptom.[33] The FDA has asked doctors to limit the use of gadolinium contrast agents to examinations where necessary information is obtained only through its use.[35] Intrathecal injections of doses higher than 1 mmol are associated with severe neurological complications and can lead to death.[36][37] The glymphatic system could be the main access of GBCA to the brain in intravenous injection.[38][39]
Continuing evidence of the retention of gadolinium in brain and other tissues following exposure to gadolinium containing contrast media, has led to a safety review by the Committee for Medicinal Products for Human Use (CHMP) which led the EMA to suspend linear gadolinium-based media, in which Gd3+ has a lower binding affinity, in 2017.[16]
In the United States, the research has led the FDA to revise its class warnings for all gadolinium-based contrast media. It is advised that the use of gadolinium-based media is based on careful consideration of the retention characteristics of the contrast. Extra care being taken in patients requiring multiple lifetime doses, pregnant, and paediatric patients, and patients with inflammatory conditions. Minimizing repeated GBCA imaging studies when possible, particularly closely spaced MRI studies. However, do not avoid or defer necessary GBCA MRI scans.[40]
In December 2017, the FDA announced in a drug safety communication it is requiring these new warnings to be included on all GBCAs. The FDA also called for increased patient education and requiring gadolinium contrast vendors to conduct additional animal and clinical studies to assess the safety of these agents.[41]
The French health authority recommends to use the lowest possible dose of a GBCA and only when essential diagnostic information cannot be obtained without it.[42]
The World Health Organization issued a restriction on use of several gadolinium contrast agents in November 2009 stating that "High-risk gadolinium-containing contrast agents (Optimark, Omniscan, Magnevist, Magnegita, and Gado-MRT ratiopharm) are contraindicated in patients with severe kidney problems, in patients who are scheduled for or have recently received a liver transplant, and in newborn babies up to four weeks of age."[43]
In magnetic resonance imaging in pregnancy, gadolinium contrast agents in the first trimester is associated with a slightly increased risk of a childhood diagnosis of several forms of rheumatism, inflammatory disorders, or infiltrative skin conditions, according to a retrospective study including 397 infants prenatally exposed to gadolinium contrast.[44] In the second and third trimester, gadolinium contrast is associated with a slightly increased risk of stillbirth or neonatal death, by the same study.[44]
Anaphylactoid reactions are rare, occurring in about 0.03–0.1%.
Iron oxide: superparamagnetic
Two types of iron oxide contrast agents exist: superparamagnetic iron oxide (SPIO) and ultrasmall superparamagnetic iron oxide (USPIO). These contrast agents consist of suspended colloids of iron oxide nanoparticles and when injected during imaging reduce the T2 signals of absorbing tissues. SPIO and USPIO contrast agents have been used successfully in some instances for liver lesion evaluation.[45][46]
- Feridex I.V. (also known as Endorem and ferumoxides). This product was discontinued by AMAG Pharma in November 2008.[47]
- Resovist (also known as Cliavist). This was approved for the European market in 2001, but production was abandoned in 2009.[48]
- Sinerem (also known as Combidex). Guerbet withdrew the marketing authorization application for this product in 2007.[49]
- Lumirem (also known as Gastromark). Gastromark was approved by the FDA in 1996[50] and was discontinued by its manufacturer in 2012.[51][52]
- Clariscan (also known as PEG-fero, Feruglose, and NC100150). This iron based contrast agent was never commercially launched and its development was discontinued in early 2000s due to safety concerns.[53] In 2017 GE Healthcare launched a macrocyclic extracellular gadolinium based contrast agent containing gadoteric acid as gadoterate meglumine under the trade name Clariscan.[54]
Iron platinum: superparamagnetic
Superparamagnetic iron–platinum particles (SIPPs) have been reported and had significantly better T2 relaxivities compared with the more common iron oxide nanoparticles. SIPPs were also encapsulated with phospholipids to create multifunctional SIPP stealth immunomicelles that specifically targeted human prostate cancer cells.[55] These are, however, investigational agents which have not yet been tried in humans. In a recent study, multifunctional SIPP micelles were synthesized and conjugated to a monoclonal antibody against prostate-specific membrane antigen.[55] The complex specifically targeted human prostate cancer cells in vitro, and these results suggest that SIPPs may have a role in the future as tumor-specific contrast agents.
Manganese
Manganese(II) chelates such as Mn-DPDP (Mangafodipir) enhance the T1 signal.[56] The chelate dissociates in vivo into manganese and DPDP; the manganese is excreted in bile, while DPDP is eliminated via kidney filtration.[57] Mangafodipir has been used in human neuroimaging clinical trials, including for neurodegenerative diseases such as multiple sclerosis.[58][59] Manganese(II) ions are often used as a contrast agent in animal studies, often called MEMRI (Manganese-Enhanced MRI).[60] Because Mn2+ ions can enter cells through calcium transport channels, it has been used for functional brain imaging.[61]
Manganese(III) chelates with porphyrins and phthalocyanines have also been studied.[56]
Unlike the other well-studied iron oxide-based nanoparticles, research on Mn-based nanoparticles is at a relatively early stage.[62]
Oral administration
A wide variety of oral contrast agents can enhance images of the gastrointestinal tract. They include gadolinium and manganese chelates, or iron salts for T1 signal enhancement. SPIO, barium sulfate, air and clay have been used to lower T2 signal. Natural products with high manganese concentration such as blueberry and green tea can also be used for T1 increasing contrast enhancement.[63]
Perflubron, a type of perfluorocarbon, has been used as a gastrointestinal MRI contrast agent for pediatric imaging.[64] This contrast agent works by reducing the number of hydrogen ions in a body cavity, thus causing it to appear dark in the images.
Protein-based MRI contrast agents
Newer research suggests the possibility of protein based contrast agents, based on the abilities of some amino acids to bind with gadolinium.[65][66][67][68]
See also
Footnotes
- "Disruption of the BBB tight junctions is thought to be an early or initiating event in new MS lesion formation. T1-w MRI in combination with low molecular weight gadolinium-based contrast agents (GBCA) is most typically used to characterize BBB compromise in MS. MRI GBCAs do not readily cross cellular membranes, are avid extracellular space markers, and are thought to enter the brain from the blood by diffusive transport between endothelial cells (ie, via intercellular pathways). Although it is widely believed that the MRI GBCAs do not cross the BBB under homeostatic conditions, there is substantial evidence that they do, albeit with very small volume transfer rate constants." — Bagnato, Gauthier, Laule, et al. (2020)[9]
References
- Rinck, Peter A. (2022). "Magnetic resonance contrast agents". Magnetic Resonance in Medicine. A critical introduction (12th ed.). TRTF – The Round Table Foundation / EMRF – European Magnetic Resonance Forum. ISBN 978-3-7460-9518-9. "Magnetic resonance contrast agents". The Round Table Foundation (trtf.eu) (offprint to download).
- Geraldes, Carlos F.G.C.; Laurent, Sophie (2009). "Classification and basic properties of contrast agents for magnetic resonance imaging". Contrast Media & Molecular Imaging. 4 (1): 1–23. doi:10.1002/cmmi.265. PMID 19156706.
- Tircsó, Gyulia; Molńar, Enricő; Csupász, Tibor; Garda, Zoltan; Botár, Richárd; Kálmán, Ferenc K.; Kovács, Zoltan; Brücher, Ernő; Tóth, Imre (2021). "Chapter 2. Gadolinium(III)-based contrast agents for magnetic resonance imaging: A re-appraisal". Metal Ions in Bio-Imaging Techniques. Springer. pp. 39–70. doi:10.1515/9783110685701-008. S2CID 233702931.
- McLeod, Shauanna M.; Mead, Thomas J. (2021). "Chapter 12. Magnetic resonance theranostics: An overview of gadolinium(II)-based strategies and magnetic particle imaging". Metal Ions in Bio-Imaging Techniques. Springer. pp. 347–370. doi:10.1515/9783110685701-018. S2CID 233710460.
- Balzer, T. (2017). "Presence of gadolinium (Gd) in the brain and body". Bayer presentation to the September 8, 2017 meeting of the Medical Imaging Drugs Advisory Committee (PDF) (Report). Silver Spring, MD: Bayer HealthCare Pharmaceuticals Inc. Retrieved 1 April 2022 – via US FDA.
- Lentschig, M.G.; Reimer, P.; Rausch-Lentschig, U.L.; Allkemper, T.; Oelerich, M.; Laub, G. (1998). "Breath-hold gadolinium-enhanced MR angiography of the major vessels at 1.0 T: Dose-response findings and angiographic correlation". Radiology. 208 (2): 353–357. doi:10.1148/radiology.208.2.9680558. PMID 9680558.
- Lee MJ, Kim MJ, Yoon CS, Song SY, Park K, Kim WS (2011). "The T2-shortening effect of gadolinium and the optimal conditions for maximizing the CNR for evaluating the biliary system: a phantom study". Korean Journal of Radiology. 12 (3): 358–364. doi:10.3348/kjr.2011.12.3.358. PMC 3088853. PMID 21603295.
- Xiao YD, Paudel R, Liu J, Ma C, Zhang ZS, Zhou SK (November 2016). "MRI contrast agents: Classification and application (Review)". International Journal of Molecular Medicine. 38 (5): 1319–1326. doi:10.3892/ijmm.2016.2744. PMID 27666161.
- Bagnato F, Gauthier SA, Laule C, Moore G, Bove R, Cai Z, et al. (May 2020). "Imaging mechanisms of disease progression in multiple sclerosis: Beyond brain atrophy". Journal of Neuroimaging. 30 (3): 251–266. doi:10.1111/jon.12700. PMID 32418324. S2CID 218677556.
- EMA recommendations on gadolinium-containing contrast agents. ema.europa.eu (Report). European Medicines Agency. Retrieved 12 July 2018.
- Kanal, Emanuel (December 2016). "Gadolinium based contrast agents (GBCA): Safety overview after 3 decades of clinical experience". Magnetic Resonance Imaging. 34 (10): 1341–1345. doi:10.1016/j.mri.2016.08.017. ISSN 1873-5894. PMID 27608608.
- Information on gadolinium-containing contrast agents (Report). Post-market Drug Safety Information for Patients and Providers. Retrieved 12 July 2018 – via fda.gov.
- "Gadolinium Based Contrast Dosing Charts" (PDF).
- McDonald, Robert J.; Levine, Deborah; Weinreb, Jeffrey; Kanal, Emanuel; Davenport, Matthew S.; Ellis, James H.; Jacobs, Paula M.; Lenkinski, Robert E.; Maravilla, Kenneth R.; Prince, Martin R.; Rowley, Howard A. (November 2018). "Gadolinium retention: A research roadmap from the 2018 NIH / ACR / RSNA workshop on gadolinium chelates". Radiology. 289 (2): 517–534. doi:10.1148/radiol.2018181151. ISSN 0033-8419. PMC 6209069. PMID 30204075.
- "Elucirem- gadopiclenol injection". DailyMed. 12 October 2022. Archived from the original on 16 October 2022. Retrieved 16 October 2022.
- "EMAs final opinion confirms restrictions on the use of linear gadolinium agents". ema.europa.eu (Press release). European Medicines Agency. 17 September 2018.
- Bousquet & etal (1988)
- Profil toxicologique des chélates de gadolinium pour l'IRM : où en est-on ? [Toxicological profile of gadolinium chelates for MRI: where do we stand?] (PDF). acadpharm.org (Report) (in French). Academie de pharmacie. 2014.
- Penfield, Jeffrey G.; Reilly, Robert F. (2007). "What nephrologists need to know about gadolinium". Nature Clinical Practice Nephrology. 3 (12): 654–668. doi:10.1038/ncpneph0660. PMID 18033225. S2CID 22435496.
- Boehm IB (2022). "Classification of gadolinium-based contrast agents (GBCAs) – adverse reactions". Magnetic Resonance Imaging. 85 (1): 1–2. doi:10.1016/j.mri.2021.10.006. PMID 34662698. S2CID 239027228.
- Grobner, T. (2005). "Gadolinium – a specific trigger for the development of nephrogenic fibrosing dermopathy and nephrogenic systemic fibrosis?". Nephrology Dialysis Transplantation. 21 (4): 1104–1108. doi:10.1093/ndt/gfk062. PMID 16431890.
- Marckmann, P.; Skov, L.; Rossen, K.; Dupont, A.; Damholt, M.B.; Heaf, J.G.; Thomsen, H.S. (2006). "Nephrogenic systemic fibrosis: Suspected causative role of gadodiamide used for contrast-enhanced magnetic resonance imaging". Journal of the American Society of Nephrology. 17 (9): 2359–2362. doi:10.1681/ASN.2006060601. PMID 16885403.
- Centers for Disease Control and Prevention (CDC) (2007). "Nephrogenic fibrosing dermopathy associated with exposure to gadolinium-containing contrast agents". Morbidity and Mortality Weekly Report (MMWR). Centers for Disease Control and Prevention (CDC). 56 (7): 137–141. PMID 17318112.
- Thomsen, H.S.; Morcos, S.K.; Dawson, P. (2006). "Is there a causal relation between the administration of gadolinium based contrast media and the development of nephrogenic systemic fibrosis (NSF)?". Clinical Radiology. 61 (11): 905–906. doi:10.1016/j.crad.2006.09.003. PMID 17018301.
- Kanal, E.; Barkovich, A.J.; Bell, C.; Borgstede, J.P.; Bradley, W.G.; Froelich, J.W.; et al. (ACR Blue Ribbon Panel on MR Safety) (2007). "ACR Guidance Document for Safe MR Practices: 2007". American Journal of Roentgenology. 188 (6): 1447–1474. doi:10.2214/AJR.06.1616. PMID 17515363.
- "Gadolinium and NSF: What is fact and what is theory?". c2i2.org. 2008. volume vi, issue 2. Retrieved 23 July 2023.
- Lim, Yu Jeong; Bang, Jisun; Ko, Youngsun; Seo, Hyun Min; Jung, Woon Yong; Yi, Joo Hark; Han, Sang Woong; Yu, Mi Yeon (7 September 2020). "Late onset nephrogenic systemic fibrosis in a patient with stage 3 chronic kidney disease: A case report". Journal of Korean Medical Science. 35 (35): e293. doi:10.3346/jkms.2020.35.e293. ISSN 1598-6357. PMC 7476800. PMID 32893521.
- Elmholdt, Tina Rask; Jørgensen, Bettina; Ramsing, Mette; Pedersen, Michael; Olesen, Anne Braae (June 2010). "Two cases of nephrogenic systemic fibrosis after exposure to the macrocyclic compound gadobutrol". NDT Plus. 3 (3): 285–287. doi:10.1093/ndtplus/sfq028. ISSN 1753-0784. PMC 5477958. PMID 28657062.
- "Questions and Answers" (PDF). International Society for Magnetic Resonance in Medicine.
- Stanescu, A. Luana; Shaw, Dennis W.; Murata, Nozomu; Murata, Kiyoko; Rutledge, Joe C.; Maloney, Ezekiel; Maravilla, Kenneth R. (March 2020). "Brain tissue gadolinium retention in pediatric patients after contrast-enhanced magnetic resonance exams: Pathological confirmation". Pediatric Radiology. 50 (3): 388–396. doi:10.1007/s00247-019-04535-w. ISSN 1432-1998. PMID 31989188. S2CID 210913930.
- Bussi, Simona; Coppo, Alessandra; Celeste, Roberto; Fanizzi, Antonello; Fringuello Mingo, Alberto; Ferraris, Andrea; et al. (4 February 2020). "Macrocyclic MR contrast agents: Evaluation of multiple-organ gadolinium retention in healthy rats". Insights into Imaging. 11 (1): 11. doi:10.1186/s13244-019-0824-5. ISSN 1869-4101. PMC 7000570. PMID 32020385.
- Boehm IB (2022). "Gadolinium deposition disease (GDD): Does the missing link exist? – A suggested pathologic model". European Journal of Internal Medicine. 105 (11): 118–120. doi:10.1016/j.ejim.2022.07.008. PMID 35864076. S2CID 250648810.
- Bower, Danielle V.; Richter, Johannes K.; von Tengg-Kobligk, Hendrik; Heverhagen, Johannes T.; Runge, Val M. (August 2019). "Gadolinium-based MRI contrast agents induce mitochondrial toxicity and cell death in human neurons, and toxicity increases with reduced kinetic stability of the agent". Investigative Radiology. 54 (8): 453–463. doi:10.1097/RLI.0000000000000567. ISSN 1536-0210. PMID 31265439. S2CID 164486744.
- Forslin, Y.; Martola, J.; Bergendal, Å.; Fredrikson, S.; Wiberg, M.K.; Granberg, T. (August 2019). "Gadolinium retention in the brain: An MRI relaxometry study of linear and macrocyclic gadolinium-based contrast agents in multiple sclerosis". American Journal of Neuroradiology. 40 (8): 1265–1273. doi:10.3174/ajnr.A6112. ISSN 0195-6108. PMC 7048491. PMID 31248867.
- FDA evaluating the risk of brain deposits with repeated use of gadolinium-based contrast agents for magnetic resonance imaging (MRI) (Report). FDA Drug Safety Communication. FDA. 18 June 2019.
- Patel, Mihilkumar; Atyani, Almohannad; Salameh, Jean-Paul; McInnes, Matthew (October 2020). "Safety of intrathecal administration of gadolinium-based contrast agents: A systematic review and meta-analysis". Radiology. 297 (1): 75–83. doi:10.1148/radiol.2020191373. ISSN 1527-1315. PMID 32720867. S2CID 220842011. Retrieved 20 August 2021.
- Provenzano, David Anthony; Pellis, Zachary; DeRiggi, Leonard (25 April 2019). "Fatal gadolinium-induced encephalopathy following accidental intrathecal administration: A case report and a comprehensive evidence-based review". Regional Anesthesia and Pain Medicine. 44 (7): 721–729. doi:10.1136/rapm-2019-100422. ISSN 1532-8651. PMID 31023932. S2CID 133608033.
- Taoka, Toshiaki; Naganawa, Shinji (10 April 2018). "Gadolinium-based Contrast Media, Cerebrospinal Fluid and the Glymphatic System: Possible Mechanisms for the Deposition of Gadolinium in the Brain". Magnetic Resonance in Medical Sciences. 17 (2): 111–119. doi:10.2463/mrms.rev.2017-0116. ISSN 1880-2206. PMC 5891336. PMID 29367513.
- Dr. Aashim Bhatia (presenter) (2019). Webinar on the role of the glymphatic system, and the growing awareness with gadolinium (Gd) deposits found in the brain (video). Archived from the original on 26 January 2023.
- "FDA warns that gadolinium-based contrast agents (GBCAs) are retained in the body; requires new class warnings" (PDF). United States Food and Drug Administration. 19 December 2017.
 This article incorporates text from this source, which is in the public domain.
This article incorporates text from this source, which is in the public domain. - "FDA warns gadolinium based contrast agents gbcas are retained body; requires new class warnings". US FDA. FDA Drug Safety Communication. 16 May 2018.
- Gadolinium pic RI reeval rapport annexe [Gadolinium peak RI re-eval report appendix]. has-sante.fr (Report) (in French). Retrieved 19 August 2021.
- Pharmaceuticals: Restrictions in use and availability (PDF) (Report). World Health Organization. 2010. p. 14 – via who.int.
- Mervak, Benjamin M.; Altun, Ersan; McGinty, Katrina A.; Hyslop, W. Brian; Semelka, Richard C.; Burke, Lauren M. (2019). "MRI in pregnancy: Indications and practical considerations". Journal of Magnetic Resonance Imaging. 49 (3): 621–631. doi:10.1002/jmri.26317. ISSN 1053-1807. PMID 30701610. S2CID 73412175.
- Nakamura, Hiroshi; Ito, Naoki; Kotake, Fumio; Mizokami, Yuji; Matsuoka, Takeshi (2000). "Tumor-detecting capacity and clinical usefulness of SPIO-MRI in patients with hepatocellular carcinoma". Journal of Gastroenterology. 35 (11): 849–855. doi:10.1007/s005350070022. PMID 11085494. S2CID 1037632.
- Shahrouki, Puja; Felker, Ely R.; Raman, Steven S.; Jeong, Woo Kyoung; Lu, David S.; Finn, J. Paul (24 October 2021). "Steady-state ferumoxytol-enhanced MRI: Early observations in benign abdominal organ masses and clinical implications". Abdominal Radiology. 47 (1): 460–470. doi:10.1007/s00261-021-03271-w. ISSN 2366-004X. PMC 8776683. PMID 34689252.
- "Feridex". Amagpharma.com. Archived from the original on 15 June 2012. Retrieved 20 June 2012.
- "Magnetic resonance TIP – MRI database : Resovist". Mr-tip.com. Softways. Retrieved 20 June 2012.
- "Update on Sinerem (TM) in Europe". AMAG Pharmaceuticals. 13 December 2007. Archived from the original on 23 March 2019. Retrieved 20 June 2012 – via Thefreelibrary.com.
- "Newly approved drug therapies (105) GastroMARK (Advanced Magnetics)". CenterWatch. Archived from the original on 29 December 2011. Retrieved 20 June 2012.
- "AMAG form 10-K for the fiscal year ended December 31, 2013". SEC / Edgar.
- "NDA 020410 for GastroMark". FDA. Retrieved 12 February 2017.
- Wang, Yi-Xiang J. (2011). "Superparamagnetic iron oxide based MRI contrast agents: Current status of clinical application". Quantitative Imaging in Medicine and Surgery. 1 (1): 35–40. doi:10.3978/j.issn.2223-4292.2011.08.03. PMC 3496483. PMID 23256052.
- "Clariscan 0.5 mmol / ml solution for injection" (PDF). Summary of product characteristics. Oslo, NO: GE Healthcare AS. 22 February 2017. Archived from the original (PDF) on 1 March 2017. Retrieved 28 February 2017.
- Taylor, Robert M.; Huber, Dale L.; Monson, Todd C.; Ali, Abdul-Mehdi S.; Bisoffi, Marco; Sillerud, Laurel O. (2011). "Multifunctional iron platinum stealth immunomicelles: Targeted detection of human prostate cancer cells using both fluorescence and magnetic resonance imaging". Journal of Nanoparticle Research. 13 (10): 4717–4729. Bibcode:2011JNR....13.4717T. doi:10.1007/s11051-011-0439-3. PMC 3223933. PMID 22121333.
- Lacerda, Sara; Ndiaye, Daouda; Tóth, Éva (2021). "Chapter 3. Manganese Complexes as Contrast Agents for Magnetic Resonance Imaging". Metal Ions in Bio-Imaging Techniques. Springer. pp. 71–99. doi:10.1515/9783110685701-009. S2CID 233682771.
- Harisinghani, Mukesh G.; Jhaveri, Kartik S.; Weissleder, Ralph; Schima, Wolfgang; Saini, Sanjay; Hahn, Peter F.; Mueller, Peter R. (2001). "MRI contrast agents for evaluating focal hepatic lesions". Clinical Radiology. 56 (9): 714–725. doi:10.1053/crad.2001.0764. PMID 11585393.
- Sudarshana, D.M.; Nair, G.; Dwyer, J.T.; Steele, S.U.; Suto, D.J.; Wu, T.; et al. (August 2019). "Manganese-enhanced MRI of the brain in healthy volunteers". American Journal of Neuroradiology. 40 (8): 1309–1316. doi:10.3174/ajnr.A6152. PMC 6754109. PMID 31371354.
- Suto, D.J.; Nair, G.; Sudarshana, D.M.; Steel, S.U.; Dwyer, J.; Beck, E.S; et al. (August 2020). "Manganese-enhanced MRI in patients with multiple sclerosis". American Journal of Neuroradiology. 41 (9): 1569–1576. doi:10.3174/ajnr.A6665. PMC 7583091. PMID 32763897.
- Koretsky, Alan P.; Silva, Afonso C. (2004). "Manganese-enhanced magnetic resonance imaging (MEMRI)". NMR in Biomedicine. 17 (8): 527–531. doi:10.1002/nbm.940. PMID 15617051.
- Lin, Yi-Jen; Koretsky, Alan P. (1997). "Manganese ion enhances T1-weighted MRI during brain activation: An approach to direct imaging of brain function". Magnetic Resonance in Medicine. 38 (3): 378–388. doi:10.1002/mrm.1910380305. PMID 9339438. S2CID 25703430.
- Zhen, Zipeng; Xie, J. (2012). "Development of Manganese-Based Nanoparticles as Contrast Probes for Magnetic Resonance Imaging". Theranostics. 2 (1): 45–54. doi:10.7150/thno.3448. PMC 3263515. PMID 22272218.
- Lee, Joseph K.T. (2006). Computed Body Tomography with MRI Correlation. Lippincott Williams & Wilkins. p. 87. ISBN 978-0-7817-4526-0 – via Internet Archive. (Lee, Joseph K. T. (23 August 2023). equivalent link. Lippincott Williams & Wilkins. ISBN 9780781745260 – via Google Books.
- Bisset, G.S.; Emery, K.H.; Meza, M.P.; Rollins, N.K.; Don, S.; Shorr, J.S. (1996). "Perflubron as a gastrointestinal MR imaging contrast agent in the pediatric population". Pediatric Radiology. 26 (6): 409–415. doi:10.1007/BF01387316. PMID 8657479. S2CID 10032242.
- Xue, Shenghui; Qiao, Jingjuan; Pu, Fan; Cameron, Mathew; Yang, Jenny J. (2013). "Design of a novel class of protein-based magnetic resonance imaging contrast agents for the molecular imaging of cancer biomarkers". Wiley Interdisciplinary Reviews: Nanomedicine and Nanobiotechnology. 5 (2): 163–179. doi:10.1002/wnan.1205. PMC 4011496. PMID 23335551.
- Li, Shunyi; Jiang, Jie; Zou, Jin; Qiao, Jingjuan; Xue, Shenghui; Wei, Lixia; et al. (2012). "PEGylation of protein-based MRI contrast agents improves relaxivities and biocompatibilities". Journal of Inorganic Biochemistry. 107 (1): 111–118. doi:10.1016/j.jinorgbio.2011.11.004. PMC 3273044. PMID 22178673.
- Xue, Shenghui; Qiao, Jingjuan; Hubbard, Kendra; White, Natalie; Wei, Lixia; Li, Shunyi; et al. (2014). "Design of ProCAs (protein-based Gd3+ MRI contrast agents) with high dose efficiency and capability for molecular imaging of cancer biomarkers". Medicinal Research Reviews. 34 (5): 1070–1099. doi:10.1002/med.21313. PMID 24615853. S2CID 42641594.
- Qiao, Jingjuan; Xue, Shenghui; Pu, Fan; White, Natalie; Liu, Zhi-Ren; Yang, Jenny J. (2014). "Molecular imaging of EGFR/HER2 cancer biomarkers by protein MRI contrast agents". Journal of Biological Inorganic Chemistry. 19 (2): 259–270. doi:10.1007/s00775-013-1076-3. PMC 3931309. PMID 24366655.
External links
- "MRI contrast agents". magnetic-resonance.org.