Mpox
Mpox (formerly known as monkeypox)[6] is an infectious viral disease that can occur in humans and some other animals.[1] Symptoms include a rash that forms blisters and then crusts over, fever, and swollen lymph nodes.[1] The illness is usually mild and most of those infected will recover within a few weeks without treatment.[5] The time from exposure to onset of symptoms ranges from five to twenty-one days and symptoms typically last from two to four weeks.[2] Cases may be severe, especially in children, pregnant women or people with suppressed immune systems.[7]
| Mpox | |
|---|---|
 | |
| Mpox rash on arm and leg of a four-year-old girl in 1971 | |
| Pronunciation |
|
| Specialty | Infectious disease[1] |
| Symptoms | Rash, fever, exhaustion, swollen lymph nodes, muscle aches, sore throat[2] |
| Complications | secondary infections, pneumonia, sepsis, encephalitis, and loss of vision with severe eye infection[1] |
| Usual onset | 5–21 days post exposure[2] |
| Duration | 2 to 4 weeks[2] |
| Types | Clade I, Clade II[1] |
| Causes | Monkeypox virus[3] |
| Diagnostic method | Testing for viral DNA[1] |
| Differential diagnosis | Chickenpox, smallpox[4] |
| Prevention | Smallpox & mpox vaccine, hand washing, covering rash, PPE, social distancing[1] |
| Treatment | Supportive[1] |
| Medication | Tecovirimat, antivirals[1] |
| Prognosis | Most recover[5] |
The disease is caused by the monkeypox virus,[lower-alpha 1] a zoonotic virus in the genus Orthopoxvirus. The variola virus, the causative agent of the disease smallpox, is also in this genus.[1] Human-to-human transmission can occur through direct contact with infected skin or body fluids, including sexual contact.[1] People remain infectious from the onset of symptoms until all the lesions have scabbed and healed.[7] It may spread from infected animals by handling infected meat or via bites or scratches.[7] Diagnosis can be confirmed by PCR testing a lesion for the virus' DNA.[1]
Vaccination is recommended for those at high risk of infection.[1] Evidence shows that the MVA-BN[lower-alpha 2] vaccine is 86% effective at reducing the risk of mpox illness.[8][9][10] The aim of treatment is to manage the symptoms and prevent complications[1] as there is no specific treatment for the disease.[11] Antiviral drugs such as tecovirimat can be used to treat mpox,[1] although their effectiveness has not been proved.[12]
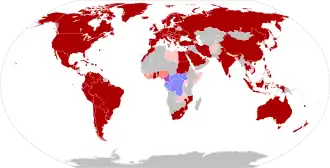
Mpox is endemic in central and western Africa, where several species of mammals are suspected to act as a natural reservoir of the virus.[1] The first human cases were diagnosed in 1970 in Basankusu, Democratic Republic of the Congo.[13] Since then the frequency and severity of outbreaks has significantly increased, possibly as a result of waning immunity since the cessation of routine smallpox vaccination.[13] The 2022–2023 mpox outbreak represents the first incidence of widespread community transmission outside of Africa. This was initially identified in the United Kingdom in May 2022, with subsequent cases confirmed in 111 countries as of May 2023.[14] The World Health Organization (WHO) declared the outbreak a Public Health Emergency of International Concern (PHEIC) between 23 July 2022 and 10 May 2023.[15]
Nomenclature
The name monkeypox was originally coined because the disease was first identified in laboratory monkeys.[3] This was subsequently criticised for being a misnomer for a number of reasons:
- Monkeys are not the main host or reservoir.
- The name reinforces stigma about African countries as a source of disease.
- It could encourage racist and homophobic stereotypes that compare people with non-human primates.
After requests by a number of public health organisations and scientists, who argued that these issues were harming the fight to contain the disease outbreak,[16] the subtypes of monkeypox virus were renamed Clade I and Clade II in August 2022. The World Health Organization announced in November 2022 that it "will adopt the term mpox in its communications, and encourages others to follow these recommendations".[6]
Signs and symptoms




Initial symptoms of mpox infection are fever, muscle pains, and sore throat, followed by an itchy or painful rash, headache, swollen lymph nodes, and fatigue. Not everyone will exhibit the complete range of symptoms.[1][2]
Most mpox patients become symptomatic 4–11 days after infection. However, the incubation period can be as short as 1 day. The 2022–2023 outbreak revealed that incubation periods of up to 4 weeks are possible, with 5% of cases having incubation periods longer than the previously assumed 21 days.[1][18]
The rash comprises many small lesions which may appear on the palms and soles, face, mouth and throat, genitals or anus.[1] They begin as small flat spots, before becoming small bumps which then fill with fluid and subsequently burst and scab over, persisting for around ten days.[2]
Some patients may manifest only a single sore from the disease while others may have hundreds.[1] It is possible for a person to be infected with monkeypox virus without showing any symptoms.[1] Symptoms typically last for two to four weeks, but may last longer if the patient has a weakened immune system.[2][1]
Complications
Complications include secondary infections, pneumonia, sepsis, encephalitis, and loss of vision following corneal infection.[1] Persons with weakened immune systems, whether due to medication, medical conditions, or HIV, are more likely to develop severe disease.[1] If infection occurs during pregnancy, this may lead to stillbirth or other complications.[7]
Outcome
Provided there are no complications, sequelae are rare; after healing, the scabs may leave pale marks before becoming darker scars.[19]
Prior to the 2022 outbreak, the risk of death in those infected was estimated from 0% to 11%.[13] With other historic case fatality rates being reported as 6% in Nigeria and 10-15% in the Democratic Republic of Congo and the Central African Republic, with a higher death rate in the more virulent Clade 1 variant that is endemic to central Africa.[20] However in the 2022 global outbreak 112 deaths were reported in 87,000 cases, with other sources reporting a risk of death as high as 0.025%.[1][20] Most reported deaths in this outbreak were among those who were immunocompromised either due to medication or poorly controlled HIV infection.[1]
In other animals
It is thought that small mammals provide a reservoir for the virus in endemic areas.[21] Spread among animals occurs via the fecal–oral route and through the nose, through wounds and eating infected meat.[22] The disease has also been reported in a wide range of other animals including monkeys, anteaters, hedgehogs, prairie dogs, squirrels, and shrews. Signs and symptoms in animals are not well researched and further studies are in progress.[23]
There have been instances of animal infection outside of endemic Africa; during the 2003 US outbreak, prairie dogs (Cynomys ludovicianus) became infected and presented with fever, cough, sore eyes, poor feeding and rash.[24] There has also been an instance of a domestic dog (Canis familiaris) which became infected displaying lesions and ulceration.[25]
Cause
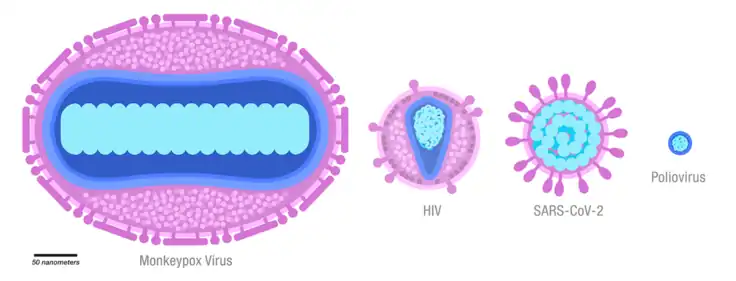
Mpox in both humans and animals is caused by infection with the monkeypox virus – a double-stranded DNA virus in the genus Orthopoxvirus, family Poxviridae, making it closely related to the smallpox, cowpox, and vaccinia viruses. The two subtypes of virus are Clade I and Clade II.[1] Clade II is further divided into subclades: Clade IIa and Clade IIb. Cases identified as part of the 2022-2023 global outbreak are caused by Clade IIb.[1] Clade I is largely limited to the DRC and is estimated to cause more severe disease and higher mortality than Clades IIa and IIb.[26]
The virus is considered to be endemic in tropical rainforest regions of Central and West Africa.[27] In addition to monkeys, the virus has been identified in Gambian pouched rats (Cricetomys gambianus), dormice (Graphiurus spp.) and African squirrels (Heliosciurus, and Funisciurus). The use of these animals as food may be an important source of transmission to humans.[1]
Transmission
Mpox can be transmitted from one person to another through contact with infectious lesion material or fluid on the skin, in the mouth or on the genitals; this includes touching, close contact and during sex. It may also spread by means of respiratory droplets from talking, coughing or sneezing.[1][28] During the 2022–2023 outbreak, transmission between people was almost exclusively via sexual contact.[29] There is a lower risk of infection from fomites (objects which can become infectious after being touched by an infected person) such as clothing or bedding, but precautions should be taken.[28]
The virus then enters the body through broken skin, or mucosal surfaces such as the mouth, respiratory tract, or genitals.[1]
The natural reservoir of monkeypox virus is thought to be small mammals in tropical Africa.[27] The virus can be transmitted from animal to human from bites or scratches, or during activities such as hunting, skinning, or cooking infected animals.[1]
Diagnosis
Clinical differential diagnosis must consider other rash illnesses, such as chickenpox, measles, bacterial skin infections, scabies, syphilis and medication-associated allergies. Diagnosis can be verified by testing for the virus. Polymerase chain reaction (PCR) testing of samples from skin lesions is the preferred laboratory test.[1]
Prevention
The MVA-BN vaccine, originally developed for smallpox, has been approved for use by persons who are either considered at high risk of exposure to mpox, or who may have recently been exposed to it.[8][9][10] The United States Centers for Disease Control and Prevention (CDC) recommends that persons investigating mpox outbreaks, those caring for infected individuals or animals, and those exposed by close or intimate contact with infected individuals or animals should receive a vaccination.[3]
Historically, smallpox vaccine had been reported to reduce the risk of mpox among previously vaccinated persons in Africa. The decrease in immunity to poxviruses in exposed populations is a factor in the increasing prevalence of human mpox. It is attributed to waning cross-protective immunity among those vaccinated before 1980, when mass smallpox vaccinations were discontinued, and to the gradually increasing proportion of unvaccinated individuals.[30]
The CDC has made detailed recommendations in addition to the standard precautions for infection control. These include that healthcare providers don a gown, mask, goggles, and a disposable filtering respirator (such as an N95), and that an infected person should be isolated a private room to keep others from possible contact.[31]
Those living in countries where mpox is endemic should avoid contact with sick mammals such as rodents, marsupials, non-human primates (dead or alive) that could harbour monkeypox virus and should refrain from eating or handling wild game (bush meat).[32][7]
During the 2022–2023 outbreak, several public health authorities launched public awareness campaigns in order to reduce spread of the disease.[33][34][35]
Treatment
Most cases of mpox present with mild symptoms and there is complete recovery within 2 to 4 weeks.[7] There is no specific treatment for the disease, although antivirals such as tecovirimat have been approved for the treatment of severe mpox.[12][36][11] Pain is common and may be severe; supportive care such as pain or fever control may be administered.[7][37] Patients with mild disease should isolate at home, stay hydrated, eat well, and take steps to maintain their mental health.[1]
Patients who are at high risk from the disease include children, pregnant women, the elderly and those who are immunocompromised.[38] For these patients, or those who have severe disease, hospital admission and careful monitoring of symptoms is recommended,[37] Symptomatic treatment is recommended for complications such as proctitis, and pruritis.[37]
Epidemiology
History
Mpox was first identified as a distinct illness in 1958 among laboratory monkeys in Copenhagen, Denmark.[39] The first documented cases in humans was in 1970, in six unvaccinated children during the smallpox eradication efforts; the first being a 9-month-old boy in the Democratic Republic of the Congo (DRC).[13][40] From 1981 to 1986, over 300 cases of human mpox were reported in the DRC, the majority being due to contact with animals.[41] The virus has been detected In Gambian pouched rats, dormice and African squirrels, which are often used as food.[42][1]
Many more mpox cases have been reported in Central and West Africa, and in the Democratic Republic of Congo in particular: 2000 cases per year are known between 2011 and 2014. The collected data is often incomplete and unconfirmed, which hinders realistic estimations of the number of cases of mpox over time.[43] Originally thought to be uncommon in humans, cases increased since the 1980s,[44][13] possibly as a result of waning immunity since the stopping of routine smallpox vaccination.[4]
Deaths
Historically, the case fatality rate (CFR) of past outbreaks was estimated at between 1% and 10%, with Clade I considered to be more severe than Clade II.[45] However the CFR of the 2022-2023 global outbreak (caused by Clade IIb) has been very low - estimated at 0.16%, with the majority of deaths in individuals who were already immunocompromised.[46] The huge difference between these estimates is attributed to: -
Future threat
The natural reservoir of monkeypox virus has not been conclusively determined, although small rodents are the most likely candidate. Without a major vaccination campaign, mpox outbreaks in humans will continue indefinitely in the endemic areas, with an ongoing risk that disease outbreaks will spread to non-endemic areas. Other evidence - that the virus is evolving to be more transmissible among humans, that it can infect a wide range of host species, and that human to animal transmission can occur - lead to concerns that mpox may either become established in new natural reservoirs outside of Africa, or cause future global epidemics.[48][49][50][51]
Following the 2022-2023 outbreak, mpox remains present in the human population at very low levels.[52]
Outbreaks
This section is an incomplete list of disease outbreaks which have been reported outside the endemic countries in tropical Africa (Benin, Cameroon, the Central African Republic, the Democratic Republic of the Congo, Gabon, Ghana, Ivory Coast, Liberia, Nigeria, the Republic of the Congo, Sierra Leone, and South Sudan).[53] Outbreaks of mpox are frequent in areas where the disease is endemic - these areas often have poor healthcare infrastructure and outbreaks are rarely documented.[54][55][56]
United States
In May 2003, a young child became ill with fever and rash after being bitten by a prairie dog purchased at a local swap meet near Milwaukee, Wisconsin.[57] In total, 71 cases of mpox were reported through 20 June 2003. All cases were traced to Gambian pouched rats imported from Accra, Ghana, in April 2003 by a Texas exotic animal distributor. No deaths resulted.[58] Electron microscopy and serologic studies were used to confirm that the disease was human mpox.[59] Everyone affected reported direct or close contact with prairie dogs, later found to be infected with the monkeypox virus.[60]
In July 2021, in the US, an American returning from a trip in Nigeria was diagnosed with mpox. Subsequent testing identified the virus as belonging to clade II. The patient was hospitalized and treated with tecovirimat and was discharged after 32 days.[61]
Sudan
During 2022, an outbreak of Clade I mpox was reported in refugee camps in Sudan.[1]
Nigeria
In September 2017, monkeypox virus was reported in Nigeria. The subsequent outbreak was, at that time, the largest ever outbreak of clade II of the virus, with 118 confirmed cases. Unlike previous outbreaks of this clade, infection was predominantly among young male adults and human-to-human transmission appears to have readily occurred. Seven deaths (5 male, 2 female, case fatality rate of 6%) were reported, including a baby and four HIV/AIDS patients. Additionally, a pregnant woman in her second trimester had a spontaneous miscarriage attributed to monkeypox virus infection.[62]
In May 2022, the Nigerian government released a report stating that between 2017 and 2022, 558 cases were confirmed across 32 states and the Federal Capital Territory. There were 8 deaths reported, making for a 3.5% Case Fatality Ratio. In 2022, NCDC implemented a National Technical Working Group for reporting and monitoring infections, strengthening response capacity.[63]
United Kingdom
In September 2018, the United Kingdom's first case of mpox was recorded. The person, a Nigerian national, is believed to have contracted mpox in Nigeria before travelling to the United Kingdom.[64] A second case was confirmed in the town of Blackpool, with a further case that of a medical worker who cared for the case from Blackpool.[65]
In December 2019, mpox was diagnosed in a person in South West England who had travelled to the UK from Nigeria.[66]
In May 2021, in the UK, three cases of mpox from a single household were identified by Public Health Wales. The index case had travelled from Nigeria.
Singapore
In May 2019, a 38-year-old man who travelled from Nigeria was hospitalised in an isolation ward at the National Centre for Infectious Diseases in Singapore, after being confirmed as the country's first case of mpox. As a result, 22 people were quarantined.[67] The case may have been linked to a simultaneous outbreak in Nigeria.[68]
2022–2023 Global outbreak
An outbreak of mpox was confirmed in May 2022.[69] The initial cluster of cases was found in the United Kingdom,[70] where the first case was detected in London on 6 May 2022[71] in a patient with a recent travel history from Nigeria (where the disease is endemic).[72] On 16 May, the UK Health Security Agency (UKHSA) confirmed four new cases with no link to travel to a country where mpox is endemic. All four cases appeared to have been infected in London.[71] From 18 May onwards, cases were reported from an increasing number of countries and regions, predominantly in Europe and in the Americas but also in Asia, in Africa, and in Oceania.[79] In May 2023, the World Health Organization declared an end to the global health emergency declared in response to the worldwide outbreak of mpox virus.[80]
See also
Notes
- The World Health Organization (the authority on disease names) announced the new name "mpox" in November 2022. But virus naming is the responsibility of the International Committee on the Taxonomy of Viruses (ICTV), which is currently reviewing all orthopoxvirus species. As of March 2023, the official name of the virus remains "monkeypox virus".[6]
- Branded as Jynneos (US), Imvamune (Canada ), Imvanex (European Union and UK)
References
- "WHO Factsheet – Mpox (Monkeypox)". World Health Organization (WHO). 18 April 2023. Archived from the original on 21 April 2022. Retrieved 21 May 2023.
- "Mpox Symptoms". U.S. Centers for Disease Control and Prevention (CDC). 2 February 2023. Archived from the original on 21 May 2023. Retrieved 21 May 2023.
- "About Mpox". U.S. Centers for Disease Control and Prevention (CDC). Archived from the original on 11 March 2023. Retrieved 13 March 2023.
- McCollum AM, Damon IK (January 2014). "Human monkeypox". Clinical Infectious Diseases. 58 (2): 260–267. doi:10.1093/cid/cit703. PMID 24158414.
- "Monkeypox". GOV.UK. 24 May 2022. Archived from the original on 18 May 2022. Retrieved 28 May 2022.
- "WHO recommends new name for monkeypox disease" (Press release). World Health Organization (WHO). 28 November 2022. Retrieved 29 November 2022.
- "Mpox (monkeypox)". World Health Organisation. 12 May 2023. Archived from the original on 23 May 2023. Retrieved 24 May 2023.
- "Jynneos Vaccine Effectiveness". Centers for Disease Control and Prevention. 19 May 2023. Archived from the original on 24 May 2023. Retrieved 24 May 2023.
- "Considerations on posology for the use of the vaccine Jynneos/ Imvanex (MVA-BN) against monkeypox" (PDF). European Medicines Agency. 19 August 2022. Archived (PDF) from the original on 28 May 2023. Retrieved 28 May 2023.
- "Protecting you from mpox (monkeypox): information on the smallpox vaccination". GOV.UK. Archived from the original on 28 May 2023. Retrieved 28 May 2023.
- "Mpox (formerly Monkeypox)". NIH: National Institute of Allergy and Infectious Diseases. 6 December 2022. Archived from the original on 23 May 2023. Retrieved 24 May 2023.
- "Patient's Guide to Mpox Treatment with Tecovirimat (TPOXX)". Centers for Disease Control and Prevention. 28 November 2022. Archived from the original on 24 May 2023. Retrieved 24 May 2023.
- Bunge, Eveline M.; Hoet, Bernard; Chen, Liddy; Lienert, Florian; Weidenthaler, Heinz; Baer, Lorraine R.; Steffen, Robert (11 February 2022). "The changing epidemiology of human monkeypox – A potential threat? A systematic review". PLOS Neglected Tropical Diseases. 16 (2): e0010141. doi:10.1371/journal.pntd.0010141. PMC 8870502. PMID 35148313.
- "Mpox is no longer officially a public health emergency; here's why we shouldn't let down our guard | Gavi, the Vaccine Alliance". www.gavi.org. Archived from the original on 13 May 2023. Retrieved 13 May 2023.
- "Mpox (monkeypox) Outbreak". www.who.int. Archived from the original on 31 July 2022. Retrieved 13 May 2023.
- "Urgent need for a non-discriminatory and non-stigmatizing nomenclature for monkeypox virus". Virological. 16 August 2022. Archived from the original on 25 May 2023. Retrieved 25 May 2023.
- Caldas, JP; Valdoleiros, SR; Rebelo, S; Tavares, M (17 October 2022). "Monkeypox after Occupational Needlestick Injury from Pustule". Emerging Infectious Diseases. 28 (12): 2516–2519. doi:10.3201/eid2812.221374. PMC 9707600. PMID 36252152. S2CID 252969061.
- McFarland, Sarah E; Marcus, Ulrich; Hemmers, Lukas; Miura, Fuminari; Iñigo Martínez, Jesús; Martínez, Fernando Martín; Montalbán, Elisa Gil; Chazelle, Emilie; Mailles, Alexandra; Silue, Yassoungo; Hammami, Naïma; Lecompte, Amaryl; Ledent, Nicolas; Vanden Berghe, Wim; Liesenborghs, Laurens; Van den Bossche, Dorien; Cleary, Paul R.; Wallinga, Jacco; Robinson, Eve P.; Johansen, Tone B.; Bormane, Tanya; Seidl, Cornelia; Coyer, Lisa; Boberg, Ronja; Jurke, Anette; Werber, Dirk; Bartel, Alexander (6 July 2023). "Estimated incubation period distributions of mpox using cases from two international European festivals and outbreaks in a club in Berlin, May to June 2022". Eurosurveillance. 28 (27). doi:10.2807/1560-7917.ES.2023.28.27.2200806. ISSN 1560-7917. PMC 10370040. PMID 37410383.
- Petersen, Brett W.; Damon, Inger K. (2020). "348. Smallpox, monkeypox and other poxvirus infections". In Goldman, Lee; Schafer, Andrew I. (eds.). Goldman-Cecil Medicine. Vol. 2 (26th ed.). Philadelphia: Elsevier. pp. 2180–2183. ISBN 978-0-323-53266-2. Archived from the original on 19 January 2023. Retrieved 28 May 2022.
- Gessain, Antoine; Nakoune, Emmanuel; Yazdanpanah, Yazdan (10 November 2022). "Monkeypox". New England Journal of Medicine. 387 (19): 1783–1793. doi:10.1056/NEJMra2208860.
- "Mpox in Animals". Centers for Disease Control and Prevention. 4 January 2023. Retrieved 25 May 2023.
- Nash, Sherrie L.; Palmer, Sally B.; Wingfield, Wayne E. (2009). "1.11. Zoonoses and zoonotic diseases". In Wingfield, Wayne E.; Palmer, Sally B. (eds.). Veterinary Disaster Response. Iowa: John Wiley & Sons. pp. 167–168. ISBN 978-0-8138-1014-0.
- "Mpox in Animals". Centers for Disease Control and Prevention. 4 January 2023. Retrieved 25 May 2023.
- "Examining Animals With Suspected Monkeypox | Monkeypox | Poxvirus". U.S. Centers for Disease Control and Prevention (CDC). 19 November 2019. Archived from the original on 19 May 2022. Retrieved 24 May 2022.
- Seang, Sophie; et al. (10 August 2022). "Evidence of human-to-dog transmission of monkeypox virus". The Lancet. 400 (10353): 658–659. doi:10.1016/S0140-6736(22)01487-8. PMC 9536767. PMID 35963267.
- "Mpox (formerly Monkeypox) | NIH: National Institute of Allergy and Infectious Diseases". www.niaid.nih.gov. 6 December 2022. Archived from the original on 23 May 2023. Retrieved 26 May 2023.
- Moore, Marlyn J.; Rathish, Balram; Zahra, Farah (30 November 2022), "Mpox (Monkeypox)", StatPearls, StatPearls Publishing, PMID 34662033, archived from the original on 16 March 2023, retrieved 26 May 2023
- "Mpox – How It Spreads". Centers for Disease Control and Prevention. 2 February 2023. Archived from the original on 21 May 2023. Retrieved 23 May 2023.
- "Safer Sex, Social Gatherings, and Mpox". Centers for Disease Control and Prevention. 28 April 2023. Archived from the original on 29 May 2023. Retrieved 26 May 2023.
- Kantele A, Chickering K, Vapalahti O, Rimoin AW (August 2016). "Emerging diseases-the monkeypox epidemic in the Democratic Republic of the Congo". Clinical Microbiology and Infection. 22 (8): 658–659. doi:10.1016/j.cmi.2016.07.004. PMC 9533887. PMID 27404372.
- "Infection Prevention and Control of Mpox in Healthcare Settings". U.S. Centers for Disease Control and Prevention (CDC). 31 October 2022. Archived from the original on 18 May 2022. Retrieved 21 May 2022.
- "Multi-country monkeypox outbreak in non-endemic countries: Update". www.who.int. Archived from the original on 30 May 2022. Retrieved 28 May 2023.
- "CDC's Mpox Toolkit for Event Organizers | Mpox | Poxvirus | CDC". Centers for Disease Control and Prevention. 23 May 2023. Archived from the original on 28 May 2023. Retrieved 28 May 2023.
- "Monkeypox – Campaign details". Department of Health and Social Care – Campaign Resource Centre. Archived from the original on 28 May 2023. Retrieved 28 May 2023.
- "Mpox (Monkeypox) awareness campaign: Communications toolkit for stakeholders". Western Australia Department of Health. 10 June 2022. Archived from the original on 28 May 2023. Retrieved 28 May 2023.
- "Tecovirimat SIGA". European Medicines Agency. 28 January 2022. Archived from the original on 16 May 2022. Retrieved 19 May 2022.
- "Mpox (monkeypox) – Treatment algorithm". BMJ Best Practice. Archived from the original on 4 December 2022. Retrieved 14 March 2023.
- "Factsheet for health professionals on mpox (monkeypox)". European Centre for Disease Prevention and Control. 25 October 2022. Archived from the original on 20 June 2022. Retrieved 29 May 2023.
- Parker, Scott; Buller, R. Mark (1 February 2013). "A review of experimental and natural infections of animals with monkeypox virus between 1958 and 2012". Future Virology. 8 (2): 129–157. doi:10.2217/fvl.12.130. ISSN 1746-0794. PMC 3635111. PMID 23626656.
- Cho, C. T.; Wenner, H. A. (March 1973). "Monkeypox virus". Bacteriological Reviews. 37 (1): 1–18. doi:10.1128/br.37.1.1-18.1973. PMC 413801. PMID 4349404.
- Meyer H, Perrichot M, Stemmler M, Emmerich P, Schmitz H, Varaine F, et al. (August 2002). "Outbreaks of disease suspected of being due to human monkeypox virus infection in the Democratic Republic of Congo in 2001". Journal of Clinical Microbiology. 40 (8): 2919–2921. doi:10.1128/JCM.40.8.2919-2921.2002. PMC 120683. PMID 12149352.
- Falendysz, Elizabeth A.; Lopera, Juan G.; Lorenzsonn, Faye; Salzer, Johanna S.; Hutson, Christina L.; Doty, Jeffrey; Gallardo-Romero, Nadia; Carroll, Darin S.; Osorio, Jorge E.; Rocke, Tonie E. (30 October 2015). "Further Assessment of Monkeypox Virus Infection in Gambian Pouched Rats (Cricetomys gambianus) Using In Vivo Bioluminescent Imaging". PLOS Neglected Tropical Diseases. 9 (10): e0004130. doi:10.1371/journal.pntd.0004130. PMC 4627722. PMID 26517839.
- Sklenovská N, Van Ranst M (September 2018). "Emergence of Monkeypox as the Most Important Orthopoxvirus Infection in Humans". Frontiers in Public Health. 6: 241. doi:10.3389/fpubh.2018.00241. PMC 6131633. PMID 30234087.
- James, William D.; Elston, Dirk; Treat, James R.; Rosenbach, Misha A.; Neuhaus, Isaac (2020). "19. Viral diseases". Andrews' Diseases of the Skin: Clinical Dermatology (13th ed.). Edinburgh: Elsevier. p. 389. ISBN 978-0-323-54753-6. Archived from the original on 19 January 2023. Retrieved 9 June 2022.
- Vogel, Lauren (15 August 2022). "Making sense of monkeypox death rates". CMAJ. 194 (31): E1097. doi:10.1503/cmaj.1096012. ISSN 0820-3946. PMC 9377567. PMID 35970550. Archived from the original on 31 May 2023. Retrieved 31 May 2023.
- "Mpox (monkeypox) - Prognosis". BMJ Best Practice. Archived from the original on 31 May 2023. Retrieved 31 May 2023.
- Dumonteil, Eric (February 2023). "Monkeypox Virus Evolution before 2022 Outbreak". Emerging Infectious Diseases. 29 (2): 451–453. doi:10.3201/eid2902.220962. PMC 9881786. PMID 36692511.
- Johnson, Philip; et al. (21 September 2022). "Evolutionary consequences of delaying intervention for monkeypox". The Lancet. 400 (10359): 1191–1193. doi:10.1016/S0140-6736(22)01789-5. PMC 9534010. PMID 36152668.
- "Monkeypox cases waning, but global threat remains". Gavi, the Vaccine Alliance. Archived from the original on 1 June 2023. Retrieved 1 June 2023.
- Adetifa, Ifedayo; et al. (2 May 2023). "Mpox neglect and the smallpox niche: a problem for Africa, a problem for the world". The Lancet. 401 (10390): 1822–1824. doi:10.1016/S0140-6736(23)00588-3. PMC 10154003. PMID 37146622. S2CID 258441920.
- "Mpox (monkeypox) and animals". Public Health Agency of Canada. 30 December 2022. Archived from the original on 1 June 2023. Retrieved 1 June 2023.
- Mathieu, Edouard; Spooner, Fiona; Dattani, Saloni; Ritchie, Hannah; Roser, Max (24 May 2022). "Mpox (monkeypox)". Our World in Data.
- "Multi-country monkeypox outbreak in non-endemic countries". World Health Organisation. Archived from the original on 22 May 2022. Retrieved 31 May 2023.
- Besombes, Camille; Mbrenga, Festus; Schaeffer, Laura; Malaka, Christian; Gonofio, Ella; Landier, Jordi; Vickos, Ulrich; Konamna, Xavier; Selekon, Benjamin; Dankpea, Joella Namsenei; Von Platen, Cassandre; Houndjahoue, Franck Gislain; Ouaïmon, Daniel Sylver; Hassanin, Alexandre; Berthet, Nicolas (December 2022). "National Monkeypox Surveillance, Central African Republic, 2001-2021". Emerging Infectious Diseases. 28 (12): 2435–2445. doi:10.3201/eid2812.220897. ISSN 1080-6059. PMC 9707566. PMID 36328951.
- Kozlov, Max (10 February 2023). "WHO may soon end mpox emergency – but outbreaks rage in Africa". Nature. 614 (7949): 600–601. doi:10.1038/d41586-023-00391-9. PMID 36765257. S2CID 256764657. Archived from the original on 16 May 2023. Retrieved 30 May 2023.
- "In Central Africa, a deadly monkeypox variant is surging". National Geographic. 20 October 2022. Archived from the original on 30 May 2023. Retrieved 30 May 2023.
- Anderson, Michael G.; Frenkel, Lawrence D.; Homann, Scott; Guffey, Jennifer (December 2003). "A case of severe monkeypox virus disease in an American child: emerging infections and changing professional values". The Pediatric Infectious Disease Journal. 22 (12): 1093–1096. doi:10.1097/01.inf.0000101821.61387.a5. PMID 14688573.
- "Medscape Monkeypox Review". Bcbsma.medscape.com. Archived from the original on 2 December 2012. Retrieved 22 March 2013.
- "Monkeypox in the United States | Monkeypox | Poxvirus". U.S. Centers for Disease Control and Prevention (CDC). 19 November 2021. Archived from the original on 27 April 2022. Retrieved 27 April 2022.
- Centers for Disease Control Prevention (July 2003). "Update: multistate outbreak of monkeypox – Illinois, Indiana, Kansas, Missouri, Ohio, and Wisconsin, 2003" (PDF). Morbidity and Mortality Weekly Report. 52 (27): 642–646. PMID 12855947. Archived (PDF) from the original on 8 December 2022. Retrieved 4 December 2022.
- "A Case of Monkeypox in a Returned Traveler". ProQuest. Archived from the original on 31 May 2022. Retrieved 23 May 2022.
- Yinka-Ogunleye, Adesola; Aruna, Olusola; Dalhat, Mahmood; Ogoina, Dimie; McCollum, Andrea; Disu, Yahyah; Mamadu, Ibrahim; Akinpelu, Afolabi; Ahmad, Adama; Burga, Joel; Ndoreraho, Adolphe (1 August 2019). "Outbreak of human monkeypox in Nigeria in 2017–18: a clinical and epidemiological report". The Lancet Infectious Diseases. 19 (8): 872–879. doi:10.1016/S1473-3099(19)30294-4. PMC 9628943. PMID 31285143. S2CID 195842553.
- Ileyemi, Mariam (10 May 2022). "Monkeypox: Nigeria records 558 cases, eight deaths in five years". Premium Times. Archived from the original on 10 May 2022. Retrieved 25 May 2022.
- "First ever case of monkeypox recorded in the UK". The Guardian. 8 September 2018. Archived from the original on 8 September 2018. Retrieved 8 September 2018.
- Gayle D (26 September 2018). "Medic becomes third person infected with monkeypox in England". The Guardian. Archived from the original on 26 September 2018. Retrieved 26 September 2018.
- "Monkeypox case confirmed in England". GOV.UK. Public Health England. 4 December 2019. Archived from the original on 12 December 2019. Retrieved 12 December 2019.
- "News Scan for May 09, 2019, Singapore sees first monkeypox case – in Nigerian national". CIDRAP. University of Minnesota. 9 May 2019. Archived from the original on 10 May 2019. Retrieved 10 May 2019.
- "Monkeypox – Singapore". World Health Organization (WHO). 16 May 2019. Archived from the original on 1 July 2019. Retrieved 17 May 2019.
- "Multi-country monkeypox outbreak in non-endemic countries". World Health Organization. 21 May 2022. Archived from the original on 22 May 2022. Retrieved 25 May 2022.
- "So, Have You Heard About Monkeypox?". The Atlantic. 19 May 2022. Archived from the original on 23 June 2022. Retrieved 2 June 2022.
- "Monkeypox cases confirmed in England – latest updates". GOV.UK. 6 September 2022. Archived from the original on 16 May 2022. Retrieved 25 September 2022.
- "Monkeypox – United Kingdom of Great Britain and Northern Ireland". World Health Organization. 16 May 2022. Archived from the original on 17 May 2022. Retrieved 17 May 2022.
- "Viruela del mono: confirmaron el primer caso del virus en el país" (in Spanish). 26 May 2022. Archived from the original on 24 June 2022. Retrieved 26 May 2022.
- "UAE reports first case of monkeypox in the country". Al Arabiya. 24 May 2022. Archived from the original on 24 May 2022. Retrieved 24 May 2022.
- Efrati, Ido. "Israel Confirms First Case of Monkeypox Virus". Haaretz. Archived from the original on 20 May 2022. Retrieved 21 May 2022.
- "Monkeypox confirmed in Melbourne and Sydney". Australian Broadcasting Corporation. 20 May 2022. Archived from the original on 20 May 2022. Retrieved 20 May 2022.
- "Morocco Reports First Monkeypox Case". Morocco World News. Archived from the original on 21 June 2022. Retrieved 2 June 2022.
- Yalley, Christian. "5 cases of monkeypox confirmed in Ghana". MyJoyOnline.com. Archived from the original on 21 June 2022. Retrieved 8 June 2022.
- [73][74][75][76][77][78]
- Kimball, Spencer (11 May 2023). "WHO says mpox outbreak, the largest in history, no longer global health emergency". CNBC. Archived from the original on 11 May 2023. Retrieved 11 May 2023.
External links
- CDC – Mpox
- WHO – Monkeypox Fact Sheet
- "Could Monkeypox Take Over Where Smallpox Left Off?". Scientific American, 4 March 2013.
- MonkeypoxTracker – Monkeypox statistics visualization site
- PoxApp – the mpox app – Assesses skin lesions and symptoms with artificial intelligence developed by Stanford University