Implantable cardioverter-defibrillator
An implantable cardioverter-defibrillator (ICD) or automated implantable cardioverter defibrillator (AICD) is a device implantable inside the body, able to perform defibrillation, and depending on the type, cardioversion and pacing of the heart. The ICD is the first-line treatment and prophylactic therapy for patients at risk for sudden cardiac death due to ventricular fibrillation and ventricular tachycardia.[1]
| Implantable cardioverter-defibrillator | |
|---|---|
 A Guidant Corporation ICD device | |
| ICD-9 | 37.94-37.97 |
| MeSH | D017147 |
| MedlinePlus | 007370 |
| eMedicine | 1971119 |
"AICD" was trademarked by the Boston Scientific corporation, so the more generic "ICD" is preferred terminology.

Current device batteries last about six to ten years. Advances in technology, such as batteries with more capacity or rechargeable batteries,[2][3] may allow batteries to last over ten years. The lead (the electrical cable connecting the device to the heart) has a much longer average longevity, but can malfunction in various ways, specifically insulation failure or fracture of the conductor, and require replacement.[4][5]
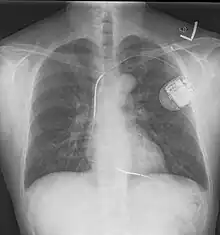
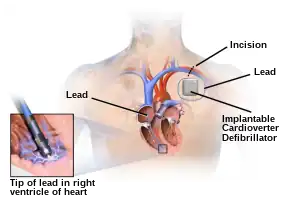
The process of implantation of an ICD system is similar to implantation of a pacemaker. In fact, ICDs are composed of an ICD generator and of wires. The first component or generator contains a computer chip or circuitry with RAM (memory), programmable software, a capacitor and a battery; this is implanted typically under the skin in the left upper chest. The second part of the system is an electrode wire or wires that, similar to pacemakers, are connected to the generator and passed through a vein to the right chambers of the heart. The lead usually lodges in the apex or septum of the right ventricle.
Just like pacemakers, ICDs can have a single wire or lead in the heart (in the right ventricle, single chamber ICD), two leads (in the right atrium and right ventricle, dual chamber ICD) or three leads (biventricular ICD, one in the right atrium, one in the right ventricle and one on the outer wall of the left ventricle). The difference between pacemakers and ICDs is that pacemakers are also available as temporary units and are generally designed to correct slow heart rates, i.e. bradycardia, while ICDs are often permanent safeguards against sudden life-threatening arrhythmias.

Recent developments include the subcutaneous ICD (S-ICD) which is placed entirely under the skin, leaving the vessels and heart untouched. [6]
Indications
Implantation of ICD is meant to prevent sudden cardiac death and is indicated under various conditions. Two broad but distinct categories are primary and secondary prevention. Primary prevention refers to patients who have not suffered a life-threatening arrhythmia episode. Secondary prevention has the strongest evidence for benefit and it refers to survivors of cardiac arrest secondary to ventricular fibrillation or hemodynamically unstable sustained ventricular tachycardia after reversible causes are excluded.[7]
Similarly, ICD use in primary prevention is to prevent cardiac death in patients who are at risk for sustained ventricular tachycardia or ventricular fibrillation. This population accounts for the bulk of all ICD implants. There are a multitude of guideline indications for ICD use in primary preventions with varying degree of supporting evidence. Periodically, both the American College of Cardiology (ACC)/American Heart Association (AHA) and European Society of Cardiology provide an update to this guideline. Some of the Class I indications are as follows:[7]
- With LVEF ≤ 35% due to prior Myocardial Infarction (MI) who are at least 40 days post-MI and are in NYHA Functional Class II or III
- With LV dysfunction due to prior MI who are at least 40 days post-MI, have an LVEF ≤ 30%, and are in NYHA Functional Class I
- With nonischemic DCM who have an LVEF ≤ 35% and who are in NYHA Functional Class II or III
- With nonsustained VT due to prior MI, LVEF < 40%, and inducible VF or sustained VT at electrophysiological study
- With structural heart disease and spontaneous sustained VT, whether hemodynamically stable or unstable
- With syncope of undetermined origin with clinically relevant, hemodynamically significant sustained VT or VF induced at electrophysiological study
Clinical trials
A number of clinical trials have demonstrated the superiority of the ICD over AAD (antiarrhythmic drugs) in the prevention of death from malignant arrhythmias. The SCD-HeFT trial (published in 2005)[8] showed a significant all-cause mortality benefit for patients with ICD. Congestive heart failure patients that were implanted with an ICD had an all-cause death risk 23% lower than placebo and an absolute decrease in mortality of 7.2 percentage points after five years in the overall population.1 Reporting in 1999, the Antiarrhythmics Versus Implantable Defibrillators (AVID) trial consisted of 1,016 patients, and deaths in those treated with AAD were more frequent (n = 122) compared with deaths in the ICD groups (n = 80, p < 0.001).[9] In 2002 the MADITII trial showed benefit of ICD treatment in patients after myocardial infarction with reduced left ventricular function (EF<30).
Initially ICDs were implanted via thoracotomy with defibrillator patches applied to the epicardium or pericardium. The device was attached via subcutaneous and transvenous leads to the device contained in a subcutaneous abdominal wall pocket. The device itself acts as an electrode. Most ICDs nowadays are implanted transvenously with the devices placed in the left pectoral region similar to pacemakers. Intravascular spring or coil electrodes are used to defibrillate. The devices have become smaller and less invasive as the technology advances. Current ICDs weigh only 70 grams and are about 12.9 mm thick.
A recent study by Birnie and colleagues at the University of Ottawa Heart Institute has demonstrated that ICDs are underused in both the United States and Canada.[10] An accompanying editorial by Dr. Chris Simpson of Queen's University explores some of the economic, geographic, social and political reasons for this.[11]
History
The development of the ICD was pioneered at Sinai Hospital in Baltimore by a team including Michel Mirowski, Morton Mower, Alois Langer, William Staewen, and Joseph "Jack" Lattuca. Mirowski teamed up with Mower and Staewen and together they commenced their research in 1969 but it was 11 years before they treated their first patient.[12][13]
The work was commenced against much skepticism even by leading experts in the field of arrhythmias and sudden death. There was doubt that their ideas would ever become a clinical reality. In 1972 Bernard Lown, the inventor of the external defibrillator, and Paul Axelrod stated in the journal Circulation – "The very rare patient who has frequent bouts of ventricular fibrillation is best treated in a coronary care unit and is better served by an effective anti-arrhythmic program or surgical correction of inadequate coronary blood flow or ventricular malfunction. In fact, the implanted defibrillator system represents an imperfect solution in search of a plausible and practical application."[12][14]
The problems to be overcome were the design of a system which would allow detection of ventricular fibrillation or ventricular tachycardia. Despite the lack of financial backing and grants, they persisted and the first device was implanted in February 1980 at Johns Hopkins Hospital by Dr. Levi Watkins Jr.[12][15]
The first devices required the chest to be cut open and a mesh electrode sewn onto the heart; the pulse generator was placed in the abdomen.[12]
Working mechanism
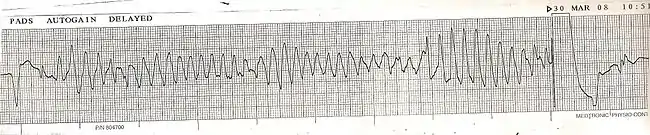
ICDs constantly monitor the rate and rhythm of the heart and can deliver therapies, by way of an electrical shock, when the heart rate exceeds a preset number. More modern devices have software designed to attempt a discrimination between ventricular fibrillation and ventricular tachycardia (VT), and may try to pace the heart faster than its intrinsic rate in the case of VT, to try to break the tachycardia before it progresses to ventricular fibrillation. This is known as overdrive pacing, or anti-tachycardia pacing (ATP). ATP is only effective if the underlying rhythm is ventricular tachycardia, and is never effective if the rhythm is ventricular fibrillation.
Many modern ICDs use a combination of various methods to determine if a fast rhythm is normal, supraventricular tachycardia, ventricular tachycardia, or ventricular fibrillation.
Rate discrimination evaluates the rate of the lower chambers of the heart (the ventricles) and compares it to the rate in the upper chambers of the heart (the atria). If the rate in the atria is faster than or equal to the rate in the ventricles, then the rhythm is most likely not ventricular in origin, and is usually more benign. If this is the case, the ICD does not provide any therapy, or withholds it for a programmable length of time.
Rhythm discrimination will see how regular a ventricular tachycardia is. Generally, ventricular tachycardia is regular. If the rhythm is irregular, it is usually due to conduction of an irregular rhythm that originates in the atria, such as atrial fibrillation. In the picture, an example of torsades de pointes can be seen; this represents a form of irregular ventricular tachycardia. In this case, the ICD will rely on rate, not regularity, to make the correct diagnosis.
Morphology discrimination checks the morphology of every ventricular beat and compares it to what the ICD knows is the morphology of normally conducted ventricular impulse for the patient. This normal ventricular impulse is often an average of a multiple of normal beats of the patient acquired in the recent past and known as a template.
The integration of these various parameters is very complex, and clinically, the occurrence of inappropriate therapy is still occasionally seen and a challenge for future software advancements.
Living with an ICD
People who have an implanted cardioverter-defibrillator can live full lives. Usually the ICD does not improve the quality of life of the patient, although it may provide a strong degree of reassurance. As with a pacemaker, however, living with an ICD does impose some restrictions on the person's lifestyle.
A patient who had an ICD fitted in 2016 following cardiac arrest described the ICD as being "half the size of your mobile phone and a little bit thicker, in my chest and has two wires attached to it ... screwed into the bottom of your heart. ... I opted to have it fitted under my pectoral muscle, so you can't see it but you can see the wires in my chest - if you wanted to. Some have them on top of the pectoral muscle, so you can see it."[16]
Physical activities
Almost all forms of physical activities can be performed by patients with an ICD. All forms of sports that do not pose a risk of damaging the ICD or because of the underlying cardiomyopathy can be undertaken by the patient. Special care should be taken not to put excessive strain on the shoulder, arm and torso area where the ICD is implanted. Doing so may damage the ICD or the leads going from the ICD generator to the patient's heart. Particularly to be avoided are exercises that cause the clavicle to be pulled down towards the ribs, such as lifting weights with the arm, on the ICD site, while standing.
Driving
ICD patients are prohibited from professional or commercial driving. A driving abstinence for private drivers is recommended following ICD implantation, but the timeframe is variable depending on the country (between 3 and 6 months for secondary prevention and 1–4 weeks for primary prevention). Following an appropriate ICD-therapy, a driving ban is recommended for 3–6 months depending on the country. After inappropriate ICD-therapy delivered for non-ventricular arrhythmias or due to the device malfunction, driving restrictions usually apply until the cause of the inappropriate therapy has been eliminated.[17]
Electro-magnetic equipment
Equipment using large magnets or generating magnetic fields, or any similar environment, must be avoided by patients with an ICD. As with other metallic objects, an ICD is normally a contraindication to the use of magnetic resonance imaging (MRI). However, several ICD manufacturers have recently introduced MR-Conditional ICDs, which allow the use of MRI under specified safe operating conditions.
Quality of life
Implantable cardioverter defibrillators have demonstrated clear life-saving benefits, while concerns about patient acceptance and psychological adjustment to the ICD have been the focus of much research.[18] Researchers, including those from the field of cardiac psychology, have concluded that the quality of life (QoL) of ICD patients is at least equal to, or better than, that of those taking anti-arrhythmic medications.[19] The largest study of examined 2,521 patients with stable heart failure in the SCD-HeFT trial.[20] Results indicated that there were no differences between ICD-treated and medication-treated groups at 30 months in patient-reported QoL.[21] Psychological adjustment following ICD implantation has also been well studied. In rare cases, the ICD can become infected and is usually bacterial in origin but other organisms such as certain fungi have occasionally been implicated.[22] This is more likely to occur in people with diabetes, heart failure, kidney failure, or a suppressed immune system.[22]
Anxiety is a common psychological side effect, with approximately 13–38% of ICD patients reporting clinically significant anxiety.[23][24] The primary etiological factors contributing to anxiety in ICD patients have not been determined, however. Depressive symptoms are also common, but the incidence of these problems has been shown to be similar to those observed in other cardiac patient groups, with approximately 24–41% of patients with ICDs experiencing depressive symptoms.[24] Problems in psychosocial adjustment to ICDs, including the experience of anxiety, among spouses or other romantic partners are also prevalent.[25] This phenomenon may be related, at least in part, to shared shock anxiety and avoidance of physical and sexual contact.[26]
See also
Notes
- Mirowski, M; Reid, PR; Mower, MM; Watkins, L; Gott, VL; Schauble, JF; Langer, A; Heilman, MS; Kolenik, SA; Fischell, RE; Weisfeldt, ML (7 August 1980). "Termination of malignant ventricular arrhythmias with an implanted automatic defibrillator in human beings". The New England Journal of Medicine. 303 (6): 322–4. doi:10.1056/nejm198008073030607. PMID 6991948.
- WiTriCity being looked at for use in pacemakers
- Wireless Qi developed for use in pacemakers
- Replacing of ICD and leads needs to be done every 5 to 10 years
- Kleemann T1 Becker T, Doenges K, Vater M, Senges J, Schneider S, Saggau W, Weisse U, Seidl K (May 2007). "Annual rate of transvenous defibrillation lead defects in implantable cardioverter-defibrillators over a period of >10 years". Circulation. 115 (19): 2474–80. doi:10.1161/CIRCULATIONAHA.106.663807. PMID 17470696.
{{cite journal}}: CS1 maint: multiple names: authors list (link) - "How ICDs and S-ICDs Work". www.bostonscientific.com. Retrieved 2022-01-30.
- Tracy, Cynthia M.; Epstein, Andrew E.; Darbar, Dawood; DiMarco, John P.; Dunbar, Sandra B.; Estes, N.A. Mark; Ferguson, T. Bruce; Hammill, Stephen C.; Karasik, Pamela E.; Link, Mark S.; Marine, Joseph E.; Schoenfeld, Mark H.; Shanker, Amit J.; Silka, Michael J.; Stevenson, Lynne Warner; Stevenson, William G.; Varosy, Paul D. (January 2013). "2012 ACCF/AHA/HRS Focused Update Incorporated Into the ACCF/AHA/HRS 2008 Guidelines for Device-Based Therapy of Cardiac Rhythm Abnormalities". Journal of the American College of Cardiology. 61 (3): e6–e75. doi:10.1016/j.jacc.2012.11.007. PMID 23265327.
- Bardy GH, Lee KL, Mark DB, Poole JE, Packer DL, Boineau R, Domanski M, Troutman C, Anderson J, Johnson G, McNulty SE, Clapp-Channing N, Davidson-Ray LD, Fraulo ES, Fishbein DP, Luceri RM, Ip JH; Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med. 2005 Jan 20; 352(3):225–37.
- "Causes of death in the Antiarrhythmics Versus Implantable Defibrillators (AVID) Trial". Journal of the American College of Cardiology. 34 (5): 1552–59. November 1999. doi:10.1016/s0735-1097(99)00376-9. PMID 10551706.

- Birnie, David H; Sambell, Christie; Johansen, Helen; Williams, Katherine; Lemery, Robert; Green, Martin S; Gollob, Michael H; Lee, Douglas S; Tang, Anthony SL (July 2007). "Use of implantable cardioverter defibrillators in Canadian and US survivors of out-of-hospital cardiac arrest". Canadian Medical Association Journal. 177 (1): 41–46. doi:10.1503/cmaj.060730. PMC 1896034. PMID 17606938. Retrieved 2007-07-29.
- Simpson, Christopher S (July 2007). "Implantable cardioverter defibrillators work – so why aren't we using them?". Canadian Medical Association Journal. 177 (1): 49–51. doi:10.1503/cmaj.070470. PMC 1896028. PMID 17606939. Retrieved 2007-07-29.
- Matchett, M; Sears, SF; Hazelton, G; Kirian, K; Wilson, E; Nekkanti, R (January 2009). "The implantable cardioverter defibrillator: its history, current psychological impact and future". Expert Review of Medical Devices. 6 (1): 43–50. doi:10.1586/17434440.6.1.43. PMID 19105779. S2CID 23062309.
- Mirowski M, Mower MM, Staewen WS, et al. (1970). "Standby automatic defibrillator: An approach to prevention of sudden coronary death". Arch Intern Med. 126 (1): 158–61. doi:10.1001/archinte.1970.00310070160014. PMID 5425512.
- Lown, B; Axelrod, P (October 1972). "Implanted standby defibrillators". Circulation. 46 (4): 637–9. doi:10.1161/01.cir.46.4.637. PMID 5072764.
- Roberts, Sam (April 16, 2015). "Levi Watkins, 70, Dies; Pioneering Heart Surgeon Pushed Civil Rights". New York Times. Retrieved April 24, 2015.
- "Eriksen to have heart-starting device". BBC Sport. 17 June 2021.
- Cooper, Mona; Berent, Theresa; Auer, Johann; Berent, Robert (December 2020). "Recommendations for driving after implantable cardioverter defibrillator implantation and the use of a wearable cardioverter defibrillator: Different viewpoints around the world". Wiener klinische Wochenschrift. 132 (23–24): 770–781. doi:10.1007/s00508-020-01675-0. ISSN 0043-5325. PMID 32435868. S2CID 218693504.
- Burns, J. L.; Serber, E. R.; Keim, S; Sears, S. F. (April 2005). "Measuring patient acceptance of implantable cardiac device therapy: Initial psychometric investigation of the Florida Patient Acceptance Survey". Journal of Cardiovascular Electrophysiology. 16 (4): 384–90. doi:10.1046/j.1540-8167.2005.40134.x. PMID 15828880. S2CID 36667780.

- Sears S, Matchett M, Conti J (2009). "Effective management of ICD patient psychosocial issues and patient critical events". J Cardiovasc Electrophysiol. 20 (11): 1297–304. doi:10.1111/j.1540-8167.2009.01526.x. PMID 19563356. S2CID 7314151.
- Bardy, Lee, Mark et al., 2005
- Mark DB, Anstrom KJ, Sun JL, Clapp-Channing NE, Tsiatis AA, Davidson-Ray L, Lee KL, Bardy GH. Quality of life with defibrillator therapy or amiodarone in heart failure. N Engl J Med 2008; 359(10):999–1008
- Rivera NT, Bray N, Wang H, Zelnick K, Osman A, Vicuña R (October 2014). "Rare infection of implantable cardioverter-defibrillator lead with Candida albicans: case report and literature review". Ther Adv Cardiovasc Dis. 8 (5): 193–201. doi:10.1177/1753944714539406. PMID 24951637.
- Bilge AK, Ozben B, Demircan S, et al. (Jun 2006). "Depression and anxiety status of patients with implantable cardioverter defibrillator and precipitating factors". Pacing Clin Electrophysiol. 29 (6): 619–26. doi:10.1111/j.1540-8159.2006.00409.x. PMID 16784428. S2CID 11982210.
- Sears SF Jr.; Todaro JF; Lewis TS; Sotile W; Conti JB. (1999). "Examining the psychosocial impact of implantable cardioverter defibrillators: a literature review". Clin Cardiol. 22 (7): 481–89. doi:10.1002/clc.4960220709. PMC 6656039. PMID 10410293.
- Vasquez-Sowell L, Sears SF, Walker RL, Kuhl EA, Conti JB (2007). "Anxiety and marital adjustment in patients with implantable cardioverter defibrillator and their spouses". Journal of Cardiopulmonary Rehabilitation and Prevention. 27 (1): 46–49. doi:10.1097/01.hcr.0000265027.79649.6a. PMID 17474644. S2CID 37445387.
- Vasquez LD, Sears SF, Shea JB, Vasquez PM (2010). "Sexual health for patients with an Implantable Cardioverter Defibrillator". Circulation. 122 (13): 465–67. doi:10.1161/circulationaha.110.949628. PMID 20876441.
References
- Bardy GH, Lee KL, Mark DB, et al. for the Sudden Cardiac Death in Heart Failure Trial (SCD-HeFT) Investigators. Amiodarone or an implantable cardioverter-defibrillator for congestive heart failure. N Engl J Med 2005; 352:225–237
- Stevenson W, Chaitman B, Ellenbogen K, Epstein A, Gross W, Hayes D, Strickberger S, Sweeney M (2004). "Clinical assessment and management of patients with implanted cardioverter-defibrillators presenting to nonelectrophysiologists". Circulation. 110 (25): 3866–69. doi:10.1161/01.CIR.0000149716.03295.7C. PMID 15611390.Full text
- Kumar and Clarke. Internal Medicine. 2009.
- Sears S, Matchett M, Conti J. "Effective management of ICD patient psychosocial issues and patient critical events. J Cardiovasc Electrophysiol 2009; 20(11):1297–304.
- Sears SF Jr.; Todaro JF; Lewis TS; Sotile W; Conti JB. (1999). "Examining the psychosocial impact of implantable cardioverter defibrillators: a literature review". Clin Cardiol. 22 (7): 481–89. doi:10.1002/clc.4960220709. PMC 6656039. PMID 10410293.
- Burns JL, Serber ER, Keim S, Sears SF (2005). "Measuring patient acceptance of implantable cardiac device therapy: initial psychometric investigation of the Florida Patient Acceptance Survey". J Cardiovasc Electrophysiol. 16 (4): 384–90. doi:10.1046/j.1540-8167.2005.40134.x. PMID 15828880. S2CID 36667780.
- Mark DB, Anstrom KJ, Sun JL, Clapp-Channing NE, Tsiatis AA, Davidson-Ray L, Lee KL, Bardy GH (2008). "Quality of life with defibrillator therapy or amiodarone in heart failure". N Engl J Med. 359 (10): 999–1008. doi:10.1056/nejmoa0706719. PMC 2823628. PMID 18768943.
- Bilge AK, Ozben B, Demircan S, et al. (Jun 2006). "Depression and anxiety status of patients with implantable cardioverter defibrillator and precipitating factors". Pacing Clin Electrophysiol. 29 (6): 619–26. doi:10.1111/j.1540-8159.2006.00409.x. PMID 16784428. S2CID 11982210.
External links
- A Defibrillator in Action Archived 2016-04-03 at the Wayback Machine
- Information on ICDs/S-ICDs from the charity Arrhythmia Alliance
- East Carolina Heart Institute at ECU, Cardiac Psychology Lab, Focus on ICD
- Samuel F. Sears, Jr., Ph.D., East Carolina University, Cardiac Psychology, ICD QoL Specialist
- Video, Coping with an ICD