Enteroendocrine cell
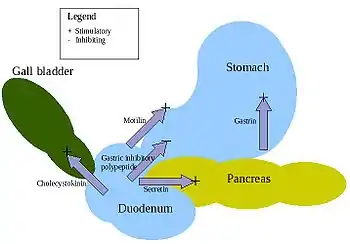
Enteroendocrine cells are specialized cells of the gastrointestinal tract and pancreas with endocrine function. They produce gastrointestinal hormones or peptides in response to various stimuli and release them into the bloodstream for systemic effect, diffuse them as local messengers, or transmit them to the enteric nervous system to activate nervous responses.[1][2] Enteroendocrine cells of the intestine are the most numerous endocrine cells of the body.[3][4][5] They constitute an enteric endocrine system as a subset of the endocrine system just as the enteric nervous system is a subset of the nervous system.[6] In a sense they are known to act as chemoreceptors, initiating digestive actions and detecting harmful substances and initiating protective responses.[7][8] Enteroendocrine cells are located in the stomach, in the intestine and in the pancreas. Microbiota play key roles in the intestinal immune and metabolic responses in these enteroendocrine cells via their fermentation product (short chain fatty acid), acetate.[9]
| Enteroendocrine cell | |
|---|---|
 Actions of the major digestive hormones secreted by enteroendocrine cells | |
| Details | |
| System | Endocrine system |
| Location | Gastrointestinal tract |
| Identifiers | |
| Latin | endocrinocyti gastroenteropancreatici |
| MeSH | D019858 |
| TH | H3.04.02.0.00024, H3.08.01.0.00003 |
| FMA | 62930 |
| Anatomical terms of microanatomy | |
Intestinal enteroendocrine cells
Intestinal enteroendocrine cells are not clustered together but spread as single cells throughout the intestinal tract.[7]
Hormones secreted include somatostatin, motilin, cholecystokinin, neurotensin, vasoactive intestinal peptide, and enteroglucagon.[10] The enteroendocrine cells sense the metabolites from intestinal commensal microbiota and, in turn, coordinate antibacterial, mechanical, and metabolic branches of the host intestinal innate immune response to the commensal microbiota.[11]
K cell
K cells secrete gastric inhibitory peptide, an incretin, which also promotes triglyceride storage.[12] K cells are mostly found in the duodenum.[13]
L cell
L cells secrete glucagon-like peptide-1, an incretin, peptide YY3-36, oxyntomodulin and glucagon-like peptide-2. L cells are primarily found in the ileum and large intestine (colon), but some are also found in the duodenum and jejunum.[14]
I cell
I cells secrete cholecystokinin (CCK), and have the highest mucosal density in the duodenum with a decreasing amount throughout the small intestine.[15] They modulate bile secretion, exocrine pancreas secretion, and satiety.[16]
G cell
Stomach enteroendocrine cells, which release gastrin, and stimulate gastric acid secretion.[17]
Enterochromaffin cell
Enterochromaffin cells are enteroendocrine and neuroendocrine cells with a close similarity to adrenomedullary chromaffin cells secreting serotonin.[18]
Enterochromaffin-like cell
Enterochromaffin-like cells or ECL cells are a type of neuroendocrine cell secreting histamine.
N cell
Located in a increasing manner throughout the small intestine, with the highest levels found in the in ileum,[19] N cells release neurotensin, and control smooth muscle contraction.[20]
S cell
S cells secrete secretin mostly from the duodenum, but also in decreasing amounts throughout the rest of the small intestine,[21] and stimulate exocrine pancreatic secretion.[16]
D cell
Also called Delta cells, D cells secrete somatostatin.
Mo cell (or M cell)
- found in crypts of the small intestine, especially in the duodenum and jejunum.
- Different from the Microfold cells (M cells) that are in Peyer's patches.
- Secrete motilin[22][23]
Gastric enteroendocrine cells
Gastric enteroendocrine cells are found in the gastric glands, mostly at their base. The G cells secrete gastrin, post-ganglionic fibers of the vagus nerve can release gastrin-releasing peptide during parasympathetic stimulation to stimulate secretion. Enterochromaffin-like cells are enteroendocrine and neuroendocrine cells also known for their similarity to chromaffin cells secreting histamine, which stimulates G cells to secrete gastrin.
Other hormones produced include cholecystokinin, somatostatin, vasoactive intestinal peptide, substance P, alpha and gamma-endorphin.[10][24]
Pancreatic enteroendocrine cells
Pancreatic enteroendocrine cells are located in the islets of Langerhans and produce most importantly the hormones insulin and glucagon. The autonomous nervous system strongly regulates their secretion, with parasympathetic stimulation stimulating insulin secretion and inhibiting glucagon secretion and sympathetic stimulation having opposite effect.[25]
Other hormones produced include somatostatin, pancreatic polypeptide, amylin and ghrelin.
Clinical significance
Rare and slow growing carcinoid and non-carcinoid tumors develop from these cells. When a tumor arises it has the capacity to secrete large volumes of hormones.[2][26]
History
The very discovery of hormones occurred during studies of how the digestive system regulates its activities, as explained at Secretin § Discovery.
Other organisms
In rats (Rattus rattus) the short-chain fatty acid receptor GPR43 is expressed both by this cell type and by mast cells of the mucosa.[27]
References
- Rehfeld JF (October 1998). "The new biology of gastrointestinal hormones". Physiological Reviews. 78 (4): 1087–108. doi:10.1152/physrev.1998.78.4.1087. PMID 9790570.
- Solcia E, Capella C, Buffa R, Usellini L, Fiocca R, Frigerio B, Tenti P, Sessa F (1981). "The diffuse endocrine-paracrine system of the gut in health and disease: ultrastructural features". Scandinavian Journal of Gastroenterology. Supplement. 70: 25–36. PMID 6118945.
- Ahlman H (2001). "The gut as the largest endocrine organ in the body". Annals of Oncology. 12 Suppl 2 (suppl 2): S63–8. doi:10.1093/annonc/12.suppl_2.s63. PMID 11762354.
- Schonhoff SE, Giel-Moloney M, Leiter AB (June 2004). "Minireview: Development and differentiation of gut endocrine cells". Endocrinology. 145 (6): 2639–44. doi:10.1210/en.2004-0051. PMID 15044355.
- Moran GW, Leslie FC, Levison SE, Worthington J, McLaughlin JT (July 2008). "Enteroendocrine cells: neglected players in gastrointestinal disorders?". Therapeutic Advances in Gastroenterology. 1 (1): 51–60. doi:10.1177/1756283X08093943. PMC 3002486. PMID 21180514.
- Wallace Hayes A (2007). Principles and Methods of Toxicology (5th, revised ed.). CRC Press. p. 1547. ISBN 9781420005424.
- Sternini C, Anselmi L, Rozengurt E (February 2008). "Enteroendocrine cells: a site of 'taste' in gastrointestinal chemosensing". Current Opinion in Endocrinology, Diabetes and Obesity. 15 (1): 73–8. doi:10.1097/MED.0b013e3282f43a73. PMC 2943060. PMID 18185066.
- Sternini C (February 2007). "Taste receptors in the gastrointestinal tract. IV. Functional implications of bitter taste receptors in gastrointestinal chemosensing". American Journal of Physiology. Gastrointestinal and Liver Physiology. 292 (2): G457–61. doi:10.1152/ajpgi.00411.2006. PMID 17095755.
- Jugder BE, Kamareddine L, Watnick PI (August 2021). "Microbiota-derived acetate activates intestinal innate immunity via the Tip60 histone acetyltransferase complex". Immunity. 54 (8): 1683–1697.e3. doi:10.1016/j.immuni.2021.05.017. ISSN 1074-7613. PMC 8363570. PMID 34107298.
- Krause WJ, Yamada J, Cutts JH (June 1985). "Quantitative distribution of enteroendocrine cells in the gastrointestinal tract of the adult opossum, Didelphis virginiana". Journal of Anatomy. 140 (4): 591–605. PMC 1165084. PMID 4077699.
- Watnick PI, Jugder BE (February 2020). "Microbial Control of Intestinal Homeostasis via Enteroendocrine Cell Innate Immune Signaling". Trends Microbiol. 28 (2): 141–149. doi:10.1016/j.tim.2019.09.005. ISSN 0966-842X. PMC 6980660. PMID 31699645.
- Parker HE, Habib AM, Rogers GJ, Gribble FM, Reimann F (February 2009). "Nutrient-dependent secretion of glucose-dependent insulinotropic polypeptide from primary murine K cells". Diabetologia. 52 (2): 289–298. doi:10.1007/s00125-008-1202-x. PMC 4308617. PMID 19082577.
- Gutierrez-Aguilar, Ruth; Woods, Stephen C (February 2011). "Nutrition and L and K-enteroendocrine cells". Current Opinion in Endocrinology, Diabetes & Obesity. 18 (1): 35–41. doi:10.1097/MED.0b013e32834190b5. PMC 3884637. PMID 21124210.
- Drucker DJ, Nauck MA (November 2006). "The incretin system: glucagon-like peptide-1 receptor agonists and dipeptidyl peptidase-4 inhibitors in type 2 diabetes" (PDF). Lancet. 368 (9548): 1696–705. doi:10.1016/s0140-6736(06)69705-5. PMID 17098089. S2CID 25748028. Archived from the original (PDF) on 2014-12-31. Retrieved 2014-12-31.
- Gilliam-Vigh, Hannah; Jorsal, Tina; Rehfeld, Jens F.; Pedersen, Jens; Poulsen, Steen S.; Vilsbøll, Tina; Knop, Filip K. (2021). "Expression of Cholecystokinin and its Receptors in the Intestinal Tract of Type 2 Diabetes Patients and Healthy Controls". The Journal of Clinical Endocrinology & Metabolism. 106 (8): 2164–2170. doi:10.1210/clinem/dgab367. PMID 34036343. S2CID 235203208. Retrieved 2023-09-20.
- Brubaker PL (July 2012). "A beautiful cell (or two or three?)". Endocrinology. 153 (7): 2945–8. doi:10.1210/en.2012-1549. PMID 22730282.
- Friis-Hansen L, Sundler F, Li Y, Gillespie PJ, Saunders TL, Greenson JK, Owyang C, Rehfeld JF, Samuelson LC (March 1998). "Impaired gastric acid secretion in gastrin-deficient mice". The American Journal of Physiology. 274 (3 Pt 1): G561–8. doi:10.1152/ajpgi.1998.274.3.G561. PMID 9530158.
- Ormsbee HS, Fondacaro JD (March 1985). "Action of serotonin on the gastrointestinal tract". Proceedings of the Society for Experimental Biology and Medicine. 178 (3): 333–8. doi:10.3181/00379727-178-42016. PMID 3919396. S2CID 34829257.
- Gilliam-Vigh, Hannah; Jorsal, Tina; Nielsen, Sophie W.; Forman, Julie L.; Pedersen, Jens; Poulsen, Steen S.; Vilsbøll, Tina; Knop, Filip K. (2023). "Expression of Neurotensin and Its Receptors Along the Intestinal Tract in Type 2 Diabetes Patients and Healthy Controls". The Journal of Clinical Endocrinology & Metabolism. 108 (9): 2211–2216. doi:10.1210/clinem/dgad146. PMID 36916883. S2CID 257506286. Retrieved 2023-09-20.
- Kitabgi P, Freychet P (August 1978). "Effects of neurotensin on isolated intestinal smooth muscles". European Journal of Pharmacology. 50 (4): 349–57. doi:10.1016/0014-2999(78)90140-1. PMID 699961.
- Gilliam-Vigh, Hannah; Jorsal, Tina; Nielsen, Sophie W.; Forman, Julie L.; Pedersen, Jens; Poulsen, Steen S.; Vilsbøll, Tina; Knop, Filip K. (2023). "Expression of Secretin and its Receptor Along the Intestinal Tract in Type 2 Diabetes Patients and Healthy Controls". The Journal of Clinical Endocrinology & Metabolism. doi:10.1210/clinem/dgad372. PMID 37335970. S2CID 259202375. Retrieved 2023-09-20.
- Daniel EE (1990-12-11). Neuropeptide Function in the Gastrointestinal Tract. CRC Press. ISBN 9780849361586.
- Goswami C, Shimada Y, Yoshimura M, Mondal A, Oda S, Tanaka T, Sakai T, Sakata I (2015-06-26). "Motilin Stimulates Gastric Acid Secretion in Coordination with Ghrelin in Suncus murinus". PLOS ONE. 10 (6): e0131554. Bibcode:2015PLoSO..1031554G. doi:10.1371/journal.pone.0131554. PMC 4482737. PMID 26115342.
- Zverkov IV, Vinogradov VA, Smagin VG (October 1983). "[Endorphin-containing cells in the gastric antral mucosa in duodenal ulcer]". Biulleten' Eksperimental'noi Biologii I Meditsiny. 96 (10): 32–4. PMID 6194833.
- Kiba T (August 2004). "Relationships between the autonomic nervous system and the pancreas including regulation of regeneration and apoptosis: recent developments". Pancreas. 29 (2): e51–8. doi:10.1097/00006676-200408000-00019. PMID 15257115. S2CID 15849806.
- Warner RR (May 2005). "Enteroendocrine tumors other than carcinoid: a review of clinically significant advances". Gastroenterology. 128 (6): 1668–84. doi:10.1053/j.gastro.2005.03.078. PMID 15887158.
- Camilleri M (October 2012). "Peripheral mechanisms in irritable bowel syndrome". N Engl J Med. 367 (17): 1626–35. doi:10.1056/NEJMra1207068. ISSN 0028-4793. PMID 23094724.
External links
- Histology image: 11604loa – Histology Learning System at Boston University - "Endocrine System: duodenum, enteroendocrine cells"