Nitrous oxide (medication)
Nitrous oxide is an inhaled gas used as a pain medication and together with other medications for anesthesia.[2] Common uses include during childbirth, following trauma, and as part of end-of-life care.[2] Onset of effect is typically within half a minute, and the effect lasts for about a minute.[1]
 Entonox CD cylinder and giving set | |
| Clinical data | |
|---|---|
| Trade names | Entonox, Nitronox, others |
| ATC code | |
| Pharmacokinetic data | |
| Onset of action | 30 seconds[1] |
| Duration of action | 1 minute[1] |
| Identifiers | |
| |
| CAS Number | |
| PubChem CID | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| ChEBI | |
| ChEMBL | |
| Chemical and physical data | |
| Formula | N2O |
| Molar mass | 44.013 g·mol−1 |
| 3D model (JSmol) | |
| |
| |
There are few side effects, other than vomiting, with short-term use.[1][2] With long-term use anemia or numbness may occur.[2] It should always be given with at least 21% oxygen.[2] It is not recommended in people with a bowel obstruction or pneumothorax.[2] Use in the early part of pregnancy is not recommended.[1] It is possible to continue breastfeeding following use.[3]
Nitrous oxide was discovered between 1772 and 1793 and used for anesthesia in 1844.[4] It is on the World Health Organization's List of Essential Medicines.[5] It often comes as a 50/50 mixture with oxygen.[1] Devices with a demand valve are available for self-administration.[6] The setup and maintenance is relatively expensive for developing countries.[7][8]
Medical uses
Nitrous oxide (N2O) is itself active (does not require any changes in the body to become active), and so has an onset in roughly the lung–brain circulation time. This gives it a peak action 30 seconds after the start of administration;[1] Entonox should thus be used accordingly, i.e. inhalation should start 30 seconds before a contraction becomes painful in labour. It is removed from the body unchanged via the lungs, and does not accumulate under normal conditions, explaining the rapid offset of around 60 seconds.[1] It is effective in managing pain during labor and delivery.[9]
Nitrous oxide is more soluble than oxygen and nitrogen, so will tend to diffuse into any air spaces within the body. This makes it dangerous to use in patients with pneumothorax or those who have recently been scuba diving, and there are cautions over its use with any bowel obstruction.
Its analgesic effect is strong (equivalent to 15 mg of subcutaneous route morphine[1])[10][11] and characterised by rapid onset and offset, i.e. it is very fast-acting and wears off very quickly.
When used in combination with other anesthetics gases, nitrous oxide causes a dose dependent increased respiratory rate and decreased tidal volumes, the net effect is a lower minute ventilation. Like volatile anesthetics, it increases cerebral blood flow and intracranial pressure. However, contrary to volatile anesthetics, it leads to an increase in cerebral metabolic rate of oxygen.[12][13]
Contraindications
N2O should not be used in patients with bowel obstruction, pneumothorax, or middle ear or sinus disease,[1] and should also not be used on any patient who has been scuba diving within the preceding 24 hours[14] or in violently disturbed psychiatric patients.[15] There are also clinical cautions in place for the first two trimesters of pregnancy and in patients with decreased levels of consciousness.[1]
Composition
The gas is a mixture of half nitrous oxide (N2O) and half oxygen (O2).[1][15] The ability to combine N2O and oxygen at high pressure while remaining in the gaseous form is caused by the Poynting effect (after John Henry Poynting, an English physicist).[1]
The Poynting effect involves the dissolution of gaseous O2 when bubbled through liquid N2O, with vaporisation of the liquid to form a gaseous O2/N2O mixture.[1]
Inhalation of pure N2O over a continued period would deprive the patient of oxygen,[16] but the 50% oxygen content prevents this from occurring. The two gases will separate at low temperatures (<4 °C), which would permit administration of hypoxic mixtures. Therefore, it is not given from a cold cylinder without being shaken (usually by cylinder inversion) to remix the gases.
 Distinct blue and white cap of an Entonox cylinder
Distinct blue and white cap of an Entonox cylinder Typical Schrader valve attachment, making the gas usable only with demand based giving sets
Typical Schrader valve attachment, making the gas usable only with demand based giving sets
Administration
The gas is self-administered through a demand valve, using a mouthpiece, bite block or face mask.[15] Self-administration of Entonox is safe because if enough is inhaled to start to induce anaesthesia, the patient becomes unable to hold the valve, and so will drop it and soon exhale the residual gas. This means that unlike other anaesthetic gases, it does not require the presence of an anaesthetist for administration. The 50% oxygen in Entonox ensures the person will have sufficient oxygen in their alveoli and conducting airways for a short period of apnea to be safe.
Mechanism of action
The pharmacological mechanism of action of N
2O in medicine is not fully known. However, it has been shown to directly modulate a broad range of ligand-gated ion channels, and this likely plays a major role in many of its effects. It moderately blocks NMDAR and β2-subunit-containing nACh channels, weakly inhibits AMPA, kainate, GABAC and 5-HT3 receptors, and slightly potentiates GABAA and glycine receptors.[17][18] It also has been shown to activate two-pore-domain K+
channels.[19] While N
2O affects quite a few ion channels, its anesthetic, hallucinogenic and euphoriant effects are likely caused predominantly, or fully, via inhibition of NMDA receptor-mediated currents.[17][20] In addition to its effects on ion channels, N
2O may act to imitate nitric oxide (NO) in the central nervous system, and this may be related to its analgesic and anxiolytic properties.[20] Nitrous oxide is 30 to 40 times more soluble than nitrogen.
History
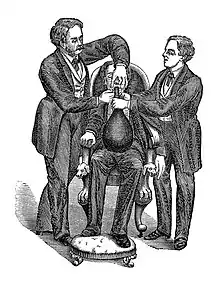
Pure N2O was first used as a medical analgesic in December 1844, when Horace Wells made the first 12–15 dental operations with the gas in Hartford.[22][23]
Its debut as a generally accepted method, however, came in 1863, when Gardner Quincy Colton introduced it more broadly at all the Colton Dental Association clinics, that he founded in New Haven and New York City.[24]
The first devices used in dentistry to administer the gas consisted of a simple breathing bag made of rubber cloth.[25]
Breathing the pure gas often caused hypoxia (oxygen insufficiency) and sometimes death by asphyxiation. Eventually practitioners became aware of the need to provide at least 21% oxygen content in the gas (the same percentage as in air).[23] In 1911, the anaesthetist Arthur Ernest Guedel first described the use of self-administration of a nitrous oxide and oxygen mix. It was not until 1961 that the first paper was published by Michael Tunstall and others, describing the administration of a pre-mixed 50:50 nitrous oxide and oxygen mix, which led to the commercialisation of the product.[23]
In 1970, Peter Baskett recognised that pre-mixed nitrous oxide and oxygen mix could have an important part to play in the provision of pre-hospital pain relief management, provided by ambulance personnel. Baskett contacted the Chief Ambulance Officer for the Gloucestershire Ambulance Brigade, Alan Withnell, to suggest this idea. This gained traction when Baskett negotiated with the British Oxygen Company, the availability of pre-mixed nitrous oxide and oxygen mix apparatus for training. Regular training sessions began at Frenchay Hospital (Bristol) and a pilot study was run in Gloucestershire (in which ambulances were crewed by a driver and one of the new highly trained ambulance men), the results of this trial were published in 1970.[26]
Today the nitrous oxide is administered in hospitals by a relative analgesia machine, which includes several improvements such as flowmeters and constant-flow regulators, an anaesthetic vaporiser, a medical ventilator, and a scavenger system, and delivers a precisely dosed and breath-actuated flow of nitrous oxide mixed with oxygen.
The machine used in dentistry is much simpler, and is meant to be used by the patient in a fully conscious state. The gas is delivered through a demand-valve inhaler over the nose, which will only release gas when the patient inhales through it.
Society and culture
Nitronox was a registered trademark of the BOC Group between 1966 and 1999,[27] and was reregistered by Hs Tm Inc since 2005 It is also colloquially known as "gas and air" in the United Kingdom.[28]
Research
Investigational trials show potential for antidepressant applications of N2O, especially for treatment-resistant forms of depression, and it is rapid-acting.[29][30][31][32]
References
- "Anaesthesia UK : Entonox". www.frca.co.uk. 26 January 2009. Archived from the original on 31 October 2007. Retrieved 15 December 2016.
- World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. p. 20. hdl:10665/44053. ISBN 9789241547659.
- "Nitrous Oxide use while Breastfeeding". Drugs.com. Archived from the original on 21 December 2016. Retrieved 15 December 2016.
- Myers RL (2007). 100 Most Important Chemical Compounds, The: A Reference Guide: A Reference Guide. ABC-CLIO. p. 198. ISBN 9780313080579. Archived from the original on 2016-12-20.
- World Health Organization (2021). World Health Organization model list of essential medicines: 22nd list (2021). Geneva: World Health Organization. hdl:10665/345533. WHO/MHP/HPS/EML/2021.02.
- British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. p. 878. ISBN 9780857111562.
- Gregory GA, Andropoulos DB (2012). Gregory's Pediatric Anesthesia, With Wiley Desktop Edition. John Wiley & Sons. p. 1148. ISBN 9781444333466. Archived from the original on 2016-12-20.
- WHO model prescribing information : drugs used in anaesthesia. World Health Organization. 1989. hdl:10665/41014. ISBN 92-4-140101-X.
- Jones L, Othman M, Dowswell T, Alfirevic Z, Gates S, Newburn M, et al. (March 2012). "Pain management for women in labour: an overview of systematic reviews". The Cochrane Database of Systematic Reviews. 2012 (3): CD009234. doi:10.1002/14651858.CD009234.pub2. PMC 7132546. PMID 22419342.
- Gao HX, Zhang JJ, Liu N, Wang Y, Ma CX, Gao LL, et al. (January 2021). "A fixed nitrous oxide/oxygen mixture as an analgesic for patients with postherpetic neuralgia: study protocol for a randomized controlled trial". Trials. 22 (1): 29. doi:10.1186/s13063-020-04960-5. PMC 7787626. PMID 33407845.
- Parbrook GD (December 1967). "The levels of nitrous oxide analgesia". British Journal of Anaesthesia. 39 (12): 974–982. doi:10.1093/bja/39.12.974. PMID 4865545.
- Clar DT, Patel S, Richards JR (2022). "Anesthetic Gases". StatPearls. PMID 30725698. NBK537013.
- Knuf K, Maani CV (2022). "Nitrous Oxide". StatPearls. PMID 30422517. NBK532922.
- Komesaroff D (1998). "Oxygen administration in diving accidents". South Pacific Underwater Medicine Society Journal. 28 (3 Supplement).
- Fisher, J; Brown, S; Cooke, M (2006). UK Ambulance Service Clinical Practice Guidelines (PDF). Joint Royal Colleges Ambulance Liaison Committee. ISBN 978-1-84690-060-0. Archived (PDF) from the original on 2011-06-05.
- "Breathing Nitrous Oxide". Nitrous Oxide Supplies. Archived from the original on 2009-02-16.
- Yamakura T, Harris RA (October 2000). "Effects of gaseous anesthetics nitrous oxide and xenon on ligand-gated ion channels. Comparison with isoflurane and ethanol". Anesthesiology. 93 (4): 1095–1101. doi:10.1097/00000542-200010000-00034. PMID 11020766. S2CID 4684919.
- Mennerick S, Jevtovic-Todorovic V, Todorovic SM, Shen W, Olney JW, Zorumski CF (December 1998). "Effect of nitrous oxide on excitatory and inhibitory synaptic transmission in hippocampal cultures". The Journal of Neuroscience. 18 (23): 9716–9726. doi:10.1523/JNEUROSCI.18-23-09716.1998. PMC 6793274. PMID 9822732.
- Gruss M, Bushell TJ, Bright DP, Lieb WR, Mathie A, Franks NP (February 2004). "Two-pore-domain K+ channels are a novel target for the anesthetic gases xenon, nitrous oxide, and cyclopropane". Molecular Pharmacology. 65 (2): 443–452. doi:10.1124/mol.65.2.443. PMID 14742687. S2CID 7762447.
- Emmanouil DE, Quock RM (2007). "Advances in understanding the actions of nitrous oxide". Anesthesia Progress. 54 (1): 9–18. doi:10.2344/0003-3006(2007)54[9:AIUTAO]2.0.CO;2. PMC 1821130. PMID 17352529.
- Thomas FR (1870). "Manual of the discovery, manufacture, and administration of nitrous oxide, or laughing gas in its relations to dental or minor surgical operations, and particularly for the painless extraction of teeth". Philadelphia : S.S. White. Retrieved 17 December 2018.
- Erving HW (May 1933). "The Discoverer of Anæsthesia: Dr. Horace Wells of Hartford". The Yale Journal of Biology and Medicine. 5 (5): 421–430. PMC 2606479. PMID 21433572. Archived from the original on 2012-12-23.
- "History of Entonox". BOC Gases. Archived from the original on 2009-07-05. Retrieved 2009-04-11.
- Sneader W (2005). "Part 1: Legacy of the past, chapter 8: systematic medicine". Drug Discovery –A History. John Wiley and Sons. pp. 74–87. ISBN 978-0-471-89980-8. Retrieved 21 April 2010.
- Miller AH (1941). "Technical Development of Gas Anesthesia". Anesthesiology. 2 (4): 398–409. doi:10.1097/00000542-194107000-00004. S2CID 71117361.
- Baskett PJ (April 1970). "Use of Entonox in the ambulance service". British Medical Journal. 2 (5700): 41–43. doi:10.1136/bmj.2.5700.41. PMC 1699783. PMID 5440577.
- "NITRONOX Trademark Information". trademarkia. Archived from the original on 2017-09-10. Retrieved 2017-07-11.
- "Entonox (gas and air)". Baby Centre. Archived from the original on 2006-11-11.
- Nagele P, Duma A, Kopec M, Gebara MA, Parsoei A, Walker M, et al. (July 2015). "Nitrous Oxide for Treatment-Resistant Major Depression: A Proof-of-Concept Trial". Biological Psychiatry. 78 (1): 10–18. doi:10.1016/j.biopsych.2014.11.016. PMID 25577164.
- Newport DJ, Carpenter LL, McDonald WM, Potash JB, Tohen M, Nemeroff CB (October 2015). "Ketamine and Other NMDA Antagonists: Early Clinical Trials and Possible Mechanisms in Depression". The American Journal of Psychiatry. 172 (10): 950–966. doi:10.1176/appi.ajp.2015.15040465. PMID 26423481.
- Nagele P, Palanca BJ, Gott B, Brown F, Barnes L, Nguyen T, et al. (June 2021). "A phase 2 trial of inhaled nitrous oxide for treatment-resistant major depression". Science Translational Medicine. 13 (597): eabe1376. doi:10.1126/scitranslmed.abe1376. PMID 34108247. S2CID 235381316.
- Mozes A (2021-06-10). "'Laughing Gas' May Help Tough-to-Treat Depression". WebMD. Retrieved 2021-06-15.
Further reading
- Clark MS, Brunick A (2014). Handbook of Nitrous Oxide and Oxygen Sedation. Elsevier Health Sciences. ISBN 9780323101301.