Pelvic floor
The pelvic floor or pelvic diaphragm is an anatomical location in the human body,[1] which has an important role in urinary and anal continence, sexual function and support of the pelvic organs.[2] The pelvic floor includes muscles, both skeletal and smooth, ligaments and fascia.[3] and separates between the pelvic cavity from above, and the perineum from below. It is formed by the levator ani muscle and coccygeus muscle, and associated connective tissue.[4]
.png.webp)
.png.webp)
The pelvic floor has two hiatuses (gaps): (anteriorly) the urogenital hiatus through which urethra and vagina pass, and (posteriorly) the rectal hiatus through which the anal canal passes.[5]
Structure
Definition
Some sources do not consider "pelvic floor" and "pelvic diaphragm" to be identical, with the "diaphragm" consisting of only the levator ani and coccygeus, while the "floor" also includes the perineal membrane and deep perineal pouch.[6] However, other sources include the fascia as part of the diaphragm.[7] In practice, the two terms are often used interchangeably.
Relations
The pelvic cavity of the true pelvis has the pelvic floor as its inferior boundary (and the pelvic brim as its superior boundary). The perineum has the pelvic floor as its superior boundary.
Posteriorly, the pelvic floor extends into the anal triangle.
Function
It is important in providing support for pelvic viscera (organs), e.g. the bladder, intestines, the uterus (in females), and in maintenance of continence as part of the urinary and anal sphincters. It facilitates birth by resisting the descent of the presenting part, causing the fetus to rotate forwards to navigate through the pelvic girdle. It helps maintain optimal intra-abdominal pressure.[5]
Clinical significance
The pelvic floor is subject to clinically relevant changes that can result in:
- Anterior vaginal wall prolapse
- Cystocele (bladder into vagina)[8]
- Urethrocele (urethra into vagina)
- Cystourethrocele (both bladder and urethra)
- Posterior vaginal wall prolapse
- Enterocele (small intestine into vagina)
- Rectocele (rectum into vagina)
- Apical vaginal prolapse
- Uterine prolapse (uterus into vagina)
- Vaginal vault prolapse (roof of vagina) - after hysterectomy
Pelvic floor dysfunction can result after treatment for gynecological cancers.[9]
Damage to the pelvic floor not only contributes to urinary incontinence but can lead to pelvic organ prolapse. Pelvic organ prolapse occurs in women when pelvic organs (e.g. the vagina, bladder, rectum, or uterus) protrude into or outside of the vagina. The causes of pelvic organ prolapse are not unlike those that also contribute to urinary incontinence. These include inappropriate (asymmetrical, excessive, insufficient) muscle tone and asymmetries caused by trauma to the pelvis. Age, pregnancy, family history, and hormonal status all contribute to the development of pelvic organ prolapse. The vagina is suspended by attachments to the perineum, pelvic side wall and sacrum via attachments that include collagen, elastin, and smooth muscle. Surgery can be performed to repair pelvic floor muscles. The pelvic floor muscles can be strengthened with Kegel exercises.[10]
Disorders of the posterior pelvic floor include rectal prolapse, rectocele, perineal hernia, and a number of functional disorders including anismus. Constipation due to any of these disorders is called "functional constipation" and is identifiable by clinical diagnostic criteria.[11]

Pelvic floor exercise (PFE), also known as Kegel exercises, may improve the tone and function of the pelvic floor muscles, which is of particular benefit for women (and less commonly men) who experience stress urinary incontinence.[12][10] However, compliance with PFE programs often is poor,[12] PFE generally is ineffective for urinary incontinence unless performed with biofeedback and trained supervision,[10] and in severe cases it may have no benefit. Pelvic floor muscle tone may be estimated using a perineometer, which measures the pressure within the vagina.[13] Medication may also be used to improve continence.[14] In severe cases, surgery may be used to repair or even to reconstruct the pelvic floor.[14]
Perineology or pelviperineology is a speciality dealing with the functional troubles of the three axes (urological, gynaecological and coloproctological) of the pelvic floor.[15]
Additional images
.png.webp)
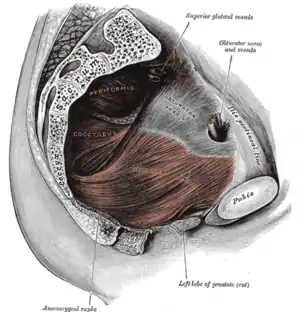 The pelvic floor muscles span the bottom of the pelvis. This image shows the left levator ani from within.
The pelvic floor muscles span the bottom of the pelvis. This image shows the left levator ani from within.

See also
References
![]() This article incorporates text in the public domain from page 420 of the 20th edition of Gray's Anatomy (1918)
This article incorporates text in the public domain from page 420 of the 20th edition of Gray's Anatomy (1918)
- Bordoni, Bruno; Sugumar, Kavin; Leslie, Stephen W. (2023), "Anatomy, Abdomen and Pelvis, Pelvic Floor", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 29489277, retrieved 2023-10-13
- Fernandes, Ana Carolina Nociti Lopes; Palacios-Ceña, Domingo; Hay-Smith, Jean; Pena, Caroline Caetano; Sidou, Mayra Feltrin; de Alencar, Amanda Lima; Ferreira, Cristine Homsi Jorge (2021-07-01). "Women report sustained benefits from attending group-based education about pelvic floor muscles: a longitudinal qualitative study". Journal of Physiotherapy. 67 (3): 210–216. doi:10.1016/j.jphys.2021.06.010. ISSN 1836-9553.
- Roch, Mélanie; Gaudreault, Nathaly; Cyr, Marie-Pierre; Venne, Gabriel; Bureau, Nathalie J.; Morin, Mélanie (September 2021). "The Female Pelvic Floor Fascia Anatomy: A Systematic Search and Review". Life. 11 (9): 900. doi:10.3390/life11090900. ISSN 2075-1729.
- "Pelvic Floor Muscles: Anatomy, Function & Conditions". Cleveland Clinic. Retrieved 2023-03-16.
- Daftary, Shirish; Chakravarti, Sudip (2011). Manual of Obstetrics (3rd ed.). Elsevier. pp. 1–16. ISBN 978-81-312-2556-1.
- Drake, Richard L.; Vogl, Wayne; Mitchell, Adam W. M. (2005). Gray's Anatomy For Students. Elsevier Health Sciences TW. p. 391. ISBN 978-0-443-06612-2.
- Herschorn, Sender (2004). "Female Pelvic Floor Anatomy: The Pelvic Floor, Supporting Structures, and Pelvic Organs". Reviews in Urology. 6 (Suppl 5): S2–S10. ISSN 1523-6161. PMC 1472875. PMID 16985905.
- "Cystocele (Prolapsed Bladder) | NIDDK". National Institute of Diabetes and Digestive and Kidney Diseases. Retrieved 2017-12-02.
- Ramaseshan, Aparna S.; Felton, Jessica; Roque, Dana; Rao, Gautam; Shipper, Andrea G.; Sanses, Tatiana V. D. (2017-09-19). "Pelvic floor disorders in women with gynecologic malignancies: a systematic review". International Urogynecology Journal. 29 (4): 459–476. doi:10.1007/s00192-017-3467-4. ISSN 0937-3462. PMC 7329191. PMID 28929201.
- Harvey, M. A. (2003). "Pelvic floor exercises during and after pregnancy: A systematic review of their role in preventing pelvic floor dysfunction". Journal of Obstetrics and Gynaecology Canada. 25 (6): 487–98. doi:10.1016/s1701-2163(16)30310-3. PMID 12806450.
- Berman, L; Aversa, J; Abir, F; Longo, W. E. (2005). "Management of disorders of the posterior pelvic floor". The Yale Journal of Biology and Medicine. 78 (4): 211–21. PMC 2259151. PMID 16720016.
- Kielb, S. J. (2005). "Stress incontinence: Alternatives to surgery". International Journal of Fertility and Women's Medicine. 50 (1): 24–9. PMID 15971718.
- Barbosa, Patrícia Brentegani; Franco, Maíra Menezes; Souza, Flaviane de Oliveira; Antônio, Flávia Ignácio; Montezuma, Thaís; Ferreira, Cristine Homsi Jorge (June 2009). "Comparison between measurements obtained with three different perineometers". Clinics. 64 (6): 527–533. doi:10.1590/s1807-59322009000600007. ISSN 1807-5932. PMC 2705146. PMID 19578656.
- "Pelvic Floor Dysfunction: Symptoms, Causes & Treatment". Cleveland Clinic. Retrieved 2023-03-16.
- Beco, J.; Mouchel, J. (2002-10-01). "Understanding the Concept of Perineology". International Urogynecology Journal. 13 (5): 275–277. doi:10.1007/s001920200060. ISSN 0937-3462. PMID 12355284. S2CID 12964013.