Phyllodes tumor
Phyllodes tumors (from Greek: phullon), are a rare type of biphasic fibroepithelial mass that form from the periductal stromal and epithelial cells of the breast.[1] They account for less than 1% of all breast neoplasms.[2] They were previously termed cystosarcoma phyllodes, coined by Johannes Muller in 1838, before being renamed to phyllodes tumor by the World Health Organization in 2003.[3] Phullon, which means 'leaf' in Greek, describes the unique papillary projections characteristic of phyllodes tumors on histology.[1] Diagnosis is made via a core-needle biopsy and treatment is typically surgical resection with wide margins (>1 cm), due to their propensity to recur.[4]
| Phyllodes tumor | |
|---|---|
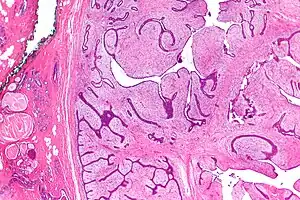 | |
| Micrograph of a phyllodes tumor (right of image) with the characteristic long clefts and myxoid cellular stroma. Normal breast and fibrocystic change are also seen (left of image). H&E stain. |

Signs and symptoms
Phyllodes tumors typically present as a firm, mobile, and palpable mass that is painless in nature.[5] On physical examination, the mass can demonstrate a smooth or nodular texture depending on its size.[3] In addition, larger masses can stretch the overlying breast tissue leading to nipple retraction, chest wall fixation, and in advanced cases, ulceration from pressure necrosis.[6]
Phyllodes tumors can grow to a variety of sizes, ranging from 0.8 to 40 cm, with the average tumor growing to between 4 and 8 cm.[7] Their growth can be slow, rapid, or demonstrate alternating growth patterns.[5] A notable feature, however, is that their growth rarely regresses, a distinguishing feature from fibroadenomas which tend to change in size based on a female's menstrual cycle.[8]
Causes
Experts are unsure of the exact etiology of phyllodes tumors.[5] Genetically, phyllodes tumors have shown to have a higher incidence with conditions such as Li-Fraumeni syndrome and BRCA1/BRCA2 mutations.[5] In addition, males with a history of gynecomastia have shown an increased incidence of developing a phyllodes tumor.[5]
Mechanism
The pathogenesis behind the development of a phyllodes tumor is not well-defined.[9] Some theories suggest a genetic cause while other literature supports the involvement of hormone and growth factor receptors, cell signal transduction pathways, and cell cycle markers.[8][9][10] Certain receptors include estrogen/progesterone, glucocorticoid, and HER2.[9] The most well-studied cell signal transduction pathway includes the Wnt pathway, which is a highly conserved genetic pathway between species.[9] In the Wnt pathway, gene transcription via B-catenin is a highly regulated process by proteins including, but not limited to, c-myc, c-jun, Fra, and cyclin D1.[9] Mutation of any these proteins can lead to the un-regulated, rapid growth characteristic of phyllodes tumors.[9]
In addition, vascular factors promoting angiogenesis have been shown to further promote growth of these breast masses.[9] These proteins include vascular endothelial growth factor (VEGF), Hypoxia-inducible factor-1a, Platelet-derived growth factor, endothelin-1, and nitrogen oxide synthase.[9] The increased expression of these angiogenic factors reflects the increased angiogenesis seen in higher grade phyllodes tumors.[9]
Genes that have been associated with a higher incidence of phyllodes tumors include Mediator Complex Subunit 12 (MED12) exon 2, Telomerase Reverse Transcriptase (TERT) promoter, and Retinoic Acid Receptor Alpha (RARA); important genes for regulating DNA synthesis.[10]
The current theory behind the development of phyllodes tumors involves the interaction between each of these pathways to some degree and how they alter the normal interaction of the breast epithelial-stromal tissue.[9]
Diagnosis
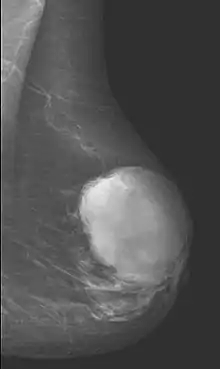
Diagnostic techniques
Radiographical imaging is the first-line test for identifying a phyllodes tumor.[11] Despite their propensity to grow rapidly and deform the overlying breast tissue, approximately 20% of phyllodes tumors can present as a nonpalpable mass on screening mammography.[12] Other imaging tools used to assess the size and spread of a phyllodes tumor include ultrasound and magnetic resonance imaging (MRI).[11] None of these imaging tools are definitive tests for differentiating a phyllodes tumor from a benign fibroadenoma.[13] Phyllodes tumors can only be diagnosed histologically, as they tend to have many overlapping features with other breast masses on physical examination and radiological imaging.[11]
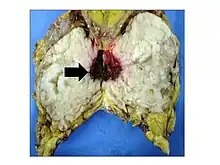
A core needle biopsy is the primary tool used to provide a definitive diagnose for a phyllodes tumors.[11] Other biopsy techniques include fine-needle aspiration and excisional biopsy. Following biopsy, histological and gross examination is performed which helps clinicians better grade and classify the phyllodes tumor.[11]
Classification
Phyllodes tumors are part of a group of breast diseases called cellular fibroepithelial lesions.[8] This term incorporates a spectrum of diseases ranging from a benign fibroadenoma to a malignant phyllodes tumor, with numerous variants in between.[14] They are classified by ICD-O, not by MeSH.[14]
Phyllodes tumors may be considered benign, borderline, or malignant depending upon their histological features, including stromal cellularity, infiltration of the epithelial-stromal interface, and mitotic activity.[15] Due to their propensity to metastasize and grow quickly, almost all phyllodes tumors are regarded as having malignant potential and treated accordingly.[15] A large case series from the M.D. Anderson Cancer Centre reported the incidence of each type of phyllodes tumor as benign (58%), borderline (12%), and malignant (30%).[16]
.jpg.webp)
Malignant phyllodes tumors can behave similarly to sarcomas leading to development of blood-borne metastases.[16] Approximately 10% of phyllodes tumor develop distant metastases and this occurrence is higher (20%) in patients with histological-identified malignant tumors.[16] The most common site for distant metastases include the lung, bone, and abdominal viscera.[17] In more insidious cases, the parotid region has also been described in literature.[18]
| Benign | Borderline | Malignant | |
|---|---|---|---|
| Margin | Pushing | Infiltrating | |
| Stromal atypia | Minimal | Moderate | Severe |
| Mitoses per 10 HPF | <5 | 5 to 9 | ≥10 |
| Stromal overgrowth | Absent | Present | |
Prevention and screening
There is no evidence-based recommendations for screening or preventative measures for early detection of phyllodes tumors.[20][21]
In patients with a prior history of a phyllodes tumor, the follow-up recommendations are employed on a case-by-case basis depending upon the grade and stage of the treated tumor.[20]
Patients who have not had a mastectomy should continue regular breast cancer screening based on the recommendations by the United States Preventative Services Task Force.[22]
Treatment
The most common, curative treatment for a phyllodes tumor is wide surgical excision with greater than 1 cm margins.[15] Other than surgery, there is no definite cure for a phyllodes tumor as chemotherapy and radiation therapy have not proven effectiveness.[15] The risk of developing local recurrence or metastases is related the histologic grade and mitotic activity of the tumor.[15] Despite proper surgical excision, a high percentage of surgeries performed to treat a phyllodes tumor demonstrate incomplete excision margins that require additional revision surgery.[23] Radiation treatment, after breast-conserving surgery with negative margins, may significantly reduce the local recurrence rate for borderline and malignant tumors.[24] A study performed in 2012 derived a risk calculator for relapse risk of phyllodes tumors after surgery.[25]
Prognosis
The prognosis of phyllodes tumor is good with an overall 87% 10-year survival rate.[5] After wide-margin surgical excision, 98.7% of benign phyllodes tumors and 80% of borderline were cured.[25] In rare cases where the tumor has metastasized, the prognosis is poor.[5] This most commonly occurs in cases of malignant grade phyllodes tumor.[5]
Epidemiology
Phyllodes tumors account for approximately 1% of all breast neoplasms.[2] They primarily occur in adult women, with very few examples reported in adolescents. Incidence is most common between the ages of 40 and 50, prior to the onset of menopause.[26] For comparison, this is about 15 years older than the typical age of patients with a fibroadenoma, a common differential diagnosis in patients with a suspected phyllodes tumors.[26] Younger women have a higher chance of having a benign phyllodes tumor, while older women are more likely to have higher-grade tumors.[23]
References
- Hasdemir S, Tolunay Ş, Özşen M, Gökgöz MŞ (January 2020). "Phyllodes Tumor of the Breast: A Clinicopathological Evaluation of 55 Cases". European Journal of Breast Health. 16 (1): 32–38. doi:10.5152/ejbh.2019.4709. PMC 6939715. PMID 31912011.
- Konstantakos AK, Graham DJ (September 2003). "Cystosarcoma phyllodes tumors in men". The American Surgeon. 69 (9): 808–811. doi:10.1177/000313480306900916. PMID 14509333. S2CID 26206134.
- Zhou ZR, Wang CC, Yang ZZ, Yu XL, Guo XM (November 2016). "Phyllodes tumors of the breast: diagnosis, treatment and prognostic factors related to recurrence". Journal of Thoracic Disease. 8 (11): 3361–3368. doi:10.21037/jtd.2016.11.03. PMC 5179374. PMID 28066617.
- Komenaka IK, El-Tamer M, Pile-Spellman E, Hibshoosh H (September 2003). "Core needle biopsy as a diagnostic tool to differentiate phyllodes tumor from fibroadenoma". Archives of Surgery. 138 (9): 987–990. doi:10.1001/archsurg.138.9.987. PMID 12963656.
- Limaiem F, Kashyap S (2022). Phyllodes Tumor Of The Breast. PMID 31082182. Retrieved 2023-01-18.
{{cite book}}:|work=ignored (help) - Khan SA, Badve S (April 2001). "Phyllodes tumors of the breast". Current Treatment Options in Oncology. 2 (2): 139–147. doi:10.1007/s11864-001-0056-y. PMID 12057132. S2CID 34616186.
- Belkacémi Y, Bousquet G, Marsiglia H, Ray-Coquard I, Magné N, Malard Y, et al. (February 2008). "Phyllodes tumor of the breast". International Journal of Radiation Oncology, Biology, Physics. 70 (2): 492–500. doi:10.1016/j.ijrobp.2007.06.059. PMID 17931796.
- Hartmann TC, Hanna MW (October 2022). "Delayed Conversion of a Fibroadenoma Into a Large Phyllodes Tumor: A Case Report". Cureus. 14 (10): e30795. doi:10.7759/cureus.30795. PMC 9701494. PMID 36447717.
- Karim, Rooshdiya Z.; Scolyer, Richard A.; Tse, Gary M.; Tan, Puay-Hoon; Putti, Thomas C.; Lee, C. Soon (February 2009). "Pathogenic mechanisms in the initiation and progression of mammary phyllodes tumours". Pathology. 41 (2): 105–117. doi:10.1080/00313020802579342. ISSN 0031-3025. PMID 19152185. S2CID 34470088.
- Sim, Yirong; Ng, Gwendolene Xin Pei; Ng, Cedric Chuan Young; Rajasegaran, Vikneswari; Wong, Suet Far; Liu, Wei; Guan, Peiyong; Nagarajan, Sanjanaa; Ng, Wai Yee; Thike, Aye Aye; Lim, Jeffrey Chun Tatt; Nasir, Nur Diyana Binte Md; Tan, Veronique Kiak Mien; Madhukumar, Preetha; Yong, Wei Sean (2019-10-23). "A novel genomic panel as an adjunctive diagnostic tool for the characterization and profiling of breast Fibroepithelial lesions". BMC Medical Genomics. 12 (1): 142. doi:10.1186/s12920-019-0588-2. ISSN 1755-8794. PMC 6813086. PMID 31647027.
- Boutas, Ioannis; Kontogeorgi, Adamandia; Dimas, Dionysios; Koufopoulos, Nektarios; Genitsaridi, Sofia-Maria; Sitara, Kyparissia; Kalantaridou, Sophia; Dimitrakakis, Constantine (October 2022). "Local recurrence for phyllodes tumours of the breast: Systematic review and meta-analysis". Oncology Letters. 24 (4): 353. doi:10.3892/ol.2022.13473. ISSN 1792-1082. PMC 9478605. PMID 36168312.
- Macdonald, O. Kenneth; Lee, Christopher M.; Tward, Jonathan D.; Chappel, Craig D.; Gaffney, David K. (2006-11-01). "Malignant phyllodes tumor of the female breast: association of primary therapy with cause-specific survival from the Surveillance, Epidemiology, and End Results (SEER) program". Cancer. 107 (9): 2127–2133. doi:10.1002/cncr.22228. ISSN 0008-543X. PMID 16998937. S2CID 35411155.
- "UpToDate". www.uptodate.com. Retrieved 2023-01-26.
- Deen SA, McKee GT, Kissin MW (February 1999). "Differential cytologic features of fibroepithelial lesions of the breast". Diagnostic Cytopathology. 20 (2): 53–56. doi:10.1002/(SICI)1097-0339(199902)20:2<53::AID-DC1>3.0.CO;2-T. PMID 9951596. S2CID 21831164.
- Tan BY, Acs G, Apple SK, Badve S, Bleiweiss IJ, Brogi E, et al. (January 2016). "Phyllodes tumours of the breast: a consensus review". Histopathology. 68 (1): 5–21. doi:10.1111/his.12876. PMC 5027876. PMID 26768026.
- Majeski, James; Stroud, Jason (2012). "Malignant phyllodes tumors of the breast: a study in clinical practice". International Surgery. 97 (2): 95–98. doi:10.9738/CC79.1. ISSN 2520-2456. PMC 3723204. PMID 23102073.
- Khanal, Suman; Singh, Yogendra P.; Bhandari, Anuja; Sharma, Rashmi (December 2018). "Malignant phyllodes tumor with metastases to lung, adrenal and brain: A rare case report". Annals of Medicine and Surgery (2012). 36: 113–117. doi:10.1016/j.amsu.2018.10.030. ISSN 2049-0801. PMC 6230968. PMID 30455875.
- Zhang, John Z.; Gu, Mai (2003). "Malignant phyllodes tumor of the breast metastatic to the parotid gland diagnosed by fine needle aspiration biopsy. A case report". Acta Cytologica. 47 (2): 253–258. doi:10.1159/000326512. ISSN 0001-5547. PMID 12685197. S2CID 3364081.
- Makhija D, Shah H, Bothra J, Jayaswal S (December 2016). "An adolescent with a phyllodes tumor: A case report and review". International Journal of Pediatrics & Adolescent Medicine. 3 (4): 180–183. doi:10.1016/j.ijpam.2016.03.005. PMC 6372421. PMID 30805490.
- Patel, Shreyaskumar R.; Zagars, Gunar K.; Pisters, Peter W. T. (June 2003). "The follow-up of adult soft-tissue sarcomas". Seminars in Oncology. 30 (3): 413–416. doi:10.1016/s0093-7754(03)00101-5. ISSN 0093-7754. PMID 12870143.
- Grabowski, Julia; Salzstein, Sidney L.; Sadler, Georgia R.; Blair, Sarah L. (October 2007). "Malignant phyllodes tumors: a review of 752 cases". The American Surgeon. 73 (10): 967–969. doi:10.1177/000313480707301007. ISSN 0003-1348. PMID 17983058. S2CID 20319387.
- "Recommendation: Breast Cancer: Screening | United States Preventive Services Taskforce". www.uspreventiveservicestaskforce.org. Retrieved 2023-01-23.
- Guillot E, Couturaud B, Reyal F, Curnier A, Ravinet J, Laé M, et al. (2011). "Management of phyllodes breast tumors". The Breast Journal. 17 (2): 129–137. doi:10.1111/j.1524-4741.2010.01045.x. PMID 21251125. S2CID 7074922.
- Barth RJ, Wells WA, Mitchell SE, Cole BF (August 2009). "A prospective, multi-institutional study of adjuvant radiotherapy after resection of malignant phyllodes tumors". Annals of Surgical Oncology. 16 (8): 2288–2294. doi:10.1245/s10434-009-0489-2. PMC 5053421. PMID 19424757.
- Reinfuss, M.; Mituś, J.; Duda, K.; Stelmach, A.; Ryś, J.; Smolak, K. (1996-03-01). "The treatment and prognosis of patients with phyllodes tumor of the breast: an analysis of 170 cases". Cancer. 77 (5): 910–916. doi:10.1002/(sici)1097-0142(19960301)77:5<910::aid-cncr16>3.0.co;2-6. ISSN 0008-543X. PMID 8608483. S2CID 46154369.
- Bernstein, L.; Deapen, D.; Ross, R. K. (1993-05-15). "The descriptive epidemiology of malignant cystosarcoma phyllodes tumors of the breast". Cancer. 71 (10): 3020–3024. doi:10.1002/1097-0142(19930515)71:10<3020::aid-cncr2820711022>3.0.co;2-g. ISSN 0008-543X. PMID 8387873. S2CID 21014296.