Recurrent miscarriage
Recurrent miscarriage or recurrent pregnancy loss is three or more consecutive pregnancy losses.[1][2] In contrast, infertility is the inability to conceive. In many cases the cause of RPL is unknown. After three or more losses, a thorough evaluation is recommended by American Society of Reproductive Medicine.[3] While accurate figures are not available, it has been estimated that anywhere between 1% and 5% of couples trying to have children are affected by recurrent miscarriage.[4][5][6]
| Recurrent miscarriage | |
|---|---|
| Other names | Habitual abortion, recurrent pregnancy loss (RPL) |
| Specialty | Obstetrics |
Causes
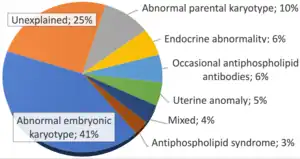
There are various causes for recurrent miscarriage, and some can be treated. Some couples never have a cause identified, often after extensive investigations.[8] About 50–75% of cases of recurrent miscarriage are unexplained.[3]
Chromosomal disorders
A balanced translocation or Robertsonian translocation in one of the partners leads to unviable fetuses that are miscarried. This explains why a karyogram is often performed in both partners if a woman has experienced repeated miscarriages.[9]
Aneuploidy may be a cause of a random spontaneous as well as recurrent pregnancy loss.[10] Aneuploidy is more common with advanced reproductive age reflecting decreased germ cell quality.[11][12]
Larger chromosomal disorders are generally detected on karyotype. In couples where a miscarried embryo has an abnormal karyotype, 76% of subsequent miscarried embryos have shown abnormal karyotypes as well. On the other hand, this group of couples have a better long-term live birth rate than those where miscarried embryos have normal karyotype.[7]
Lifestyle factors
While lifestyle factors have been associated with increased risk for miscarriage in general, and are usually not listed as specific causes for RPL, every effort should be made to address these issues in patients with RPL. Of specific concern are chronic exposures to toxins including smoking, alcohol, and drugs.[10]
Research on Caffeine before Pregnancy
Some research on the maternal use of caffeine before conception found appreciable evidence that caffeine usage in excess of 300 mg/d increases the risk of miscarriage. The same study found that use of caffeine smaller usage than this amount is correlated with an increase in the risk of miscarriage, though with odds ratios that included 1 at the 95% CI.[13]
Research on Alcohol and Caffeine During Pregnancy
Research found that 5 or more units of alcohol per week during pregnancy and 375 mg or more caffeine per day during pregnancy may increase the risk of spontaneous abortion.[14]
Research on stress, psychological support, and pregnancy loss
Research found that there is "increased relative risk of spontaneous abortion (odds ratio 1.28, 95% confidence interval 1.05-1.57)...for women experiencing high job stress."[15] Another research review found that the risk of miscarriage is higher for women with a "history of exposure to psychological stress (OR 1.42, 95% CI 1.19–1.70)"[16] However, the authors of these studies[15][16] also point out that measuring stress is difficult, and that the results must therefore be interpreted with some caution. In addition, one of the studies[16] notes that, while there are no randomized trials to study stress as it relates to pregnancy loss, one study found that a program of structured psychological support increased live birth rate among women with recurrent miscarriage.[17]
Anatomical conditions
Fifteen percent of women who have experienced three or more recurring miscarriages have some anatomical reason for the inability to complete the pregnancy.[18] The structure of the uterus has an effect on the ability to carry a child to term. Anatomical differences are common and can be congenital.
| Type of Uterine structure |
Miscarriage rate associated with defect |
References |
|---|---|---|
| Bicornate uterus | 40–79% | [19][20] |
| Septate or unicornate | 34–88% | [19][21] |
| Arcuate | unknown | [19][21] |
| Didelphhys | 40% | [19][21] |
| Fibroids | unknown | [21] |
Cervical conditions
In the second trimester a weak cervix can become a recurrent problem. Such cervical incompetence leads to premature pregnancy loss resulting in miscarriages or preterm deliveries. It has been estimated that cervical insufficiency is a cause in about 8% of women with second trimester recurrent miscarriages.[22]
Endocrine disorders
Women with hypothyroidism are at increased risk for pregnancy losses. Unrecognized or poorly treated diabetes mellitus leads to increased miscarriages. Women with polycystic ovary syndrome also have higher loss rates possibly related to hyperinsulinemia or excess androgens. Inadequate production of progesterone in the luteal phase may set the stage for RPL (see below).
Thrombophilia
An important example is the possible increased risk of miscarriage in women with thrombophilia (propensity for blood clots). The most common problem is the factor V Leiden and prothrombin G20210A mutation.[10] Some preliminary studies suggest that anticoagulant medication may improve the chances of carrying pregnancy to term but these studies need to be confirmed before they are adopted in clinical practice.[23] Note that many women with thrombophilia go through one or more pregnancies with no difficulties, while others may have pregnancy complications. Thrombophilia may explain up to 49–65% of recurrent miscarriages.[24]
Immune factors
A common feature of immune factors in causing recurrent pregnancy loss appears to be a decreased maternal immune tolerance towards the fetus.[25]
Antiphospholipid syndrome
The antiphospholipid syndrome is an autoimmune disease that is a common cause of recurrent pregnancy loss.[5][10] Around 15% of the women who have recurrent miscarriages have high levels of antiphospholipid antibodies.[5] Women who have had more than one miscarriage in the first trimester, or a miscarriage in the second trimester, may have their blood tested for antibodies, to determine if they have antiphospholipid syndrome.[5] Women diagnosed with antiphospholipid syndrome generally take aspirin or heparin in subsequent pregnancies, but questions remain due to the lack of high quality trials.[26][27]
Thyroid antibodies
Anti-thyroid autoantibodies are associated with an increased risk of recurrent miscarriage with an odds ratio of 2.3 with a 95% confidence interval of 1.5–3.5.[28]
Increased uterine NK cells
Natural killer cells, a type of white blood cell, are present in uterine tissue. High levels of these cells may be linked to RPL but high numbers or the presence of these cells is not a predictor of pregnancy loss in women who have not have had a miscarriage.[29]
Parental HLA sharing
Earlier studies that perhaps paternal sharing of HLA genes would be associated with increased pregnancy loss have not been confirmed.
Male-specific minor histocompatibility
Immunization of mothers against male-specific minor histocompatibility (H-Y) antigens has a pathogenic role in many cases of secondary recurrent miscarriage, that is, recurrent miscarriage in pregnancies succeeding a previous live birth. An example of this effect is that the male:female ratio of children born prior and subsequent to secondary recurrent miscarriage is 1.49 and 0.76 respectively.[30]
Ovarian factors
Luteal phase defect
The issue of a luteal phase defect is complex. The theory behind the concept suggests that an inadequate amount of progesterone is produced by the corpus luteum to maintain the early pregnancy. Assessment of this situation was traditionally carried out by an endometrial biopsy, however recent studies have not confirmed that such assessment is valid.[10] Studies about the value of progesterone supplementation remain deficient, however, such supplementation is commonly carried out on an empirical basis.
Infection
Infections are estimated to be responsible for between 0.5 and 5% of cases with recurrent miscarriage.[31] The main suspected pathogens are mycoplasma, ureaplasma, Chlamydia trachomatis, Listeria monocytogenes, and herpes simplex virus.[31] An infectious evaluation may be warranted in people with immunodeficiency, or with signs of chronic endometritis/cervicitis on examination.[31] Otherwise, there is no evidence that routine infectious evaluation is appropriate or productive.[31]
Chronic endometritis (CE) due to common bacteria has been found to be prevalent in some women with a history of recurrent miscarriage. One study found that 71 percent of women who tested positive for this condition were successfully treated by an antibiogram-based antibiotic treatment. 78.4 percent of these women subsequently became pregnant in the year following treatment. The study concludes that "CE is frequent in women with recurrent miscarriages," and that "antibiotic treatment seems to be associated with an improved reproductive outcome." The authors also conclude, "that hysteroscopy should be a part of the diagnostic workup of infertile women complaining of unexplained recurrent miscarriage."[32] Despite challenges in diagnosing chronic endometritis, often done by identifying plasma cells within the lining of the womb, a recent study identified women with chronic endometritis were more likely to have a miscarriage than women without.[33]
Assessment
Transvaginal ultrasonography has become the primary method of assessment of the health of an early pregnancy.
In non-pregnant patients who are evaluated for recurrent pregnancy loss the following tests are usually performed. Parental chromosome testing (karyogram) is generally recommended after 2 or 3 pregnancy losses. Blood tests for thrombophilia, ovarian function, thyroid function and diabetes are performed.
Treatment
If the likely cause of recurrent pregnancy loss can be determined treatment is to be directed accordingly. In pregnant women with a history of recurrent miscarriage, anticoagulants seem to increase the live birth rate among those with antiphospholipid syndrome and perhaps those with congenital thrombophilia but not in those with unexplained recurrent miscarriage.[34] One study found that in many women with chronic endometritis, "fertility was restored after appropriate antibiotic treatment."[32]
For women with unexplained recurrent pregnancy loss, research suggests that specific antenatal counseling and psychological support may result in a higher chance of pregnancy success.[35] Some research finds that for these patients psychological support and ultrasound in early pregnancy "gives 'success rates' of between 70% and 80%".[36]
However, each additional loss worsens the prognostic for a successful pregnancy and increases the psychological and physical risks to the mother. Aspirin has no effect in preventing recurrent miscarriage in women with unexplained recurrent pregnancy loss.[37] Immunotherapy has not been found to help.[38]
In certain chromosomal situations, while treatment may not be available, in vitro fertilization with preimplantation genetic diagnosis may be able to identify embryos with a reduced risk of another pregnancy loss which then would be transferred. However, in vitro fertilization does not improve maternal-fetal tolerance imbalances.
Psychological effects of miscarriages
There is significant, and often unrecognized, psychological and psychiatric trauma for the mother – for many, miscarriage represents the loss of a future child, of motherhood, and engenders doubts regarding her ability to procreate.[39]
"There is tremendous psychological impact of recurrent miscarriage. Psychological support in the form of frequent discussions and sympathetic counseling are crucial to the successful evaluation and treatment of the anxious couple. When no etiologic factor is identified, no treatment started at 60% to 80% fetal salvage rate still may be expected. Therefore, couples with unexplained recurrent miscarriage should be offered appropriate emotional support and reassurance."[40]
Association with later disease
Recurrent miscarriage in itself is associated with later development of coronary artery disease with an odds ratio of approximately 2,[41] increased risk of ovarian cancer,[42] increased risk of cardiovascular complications,[43] and an increased risk of all-cause mortality of 44%, 86%, and 150% for women with a history of 1, 2, or 3 miscarriages, respectively.[44]
Women with a history of recurrent miscarriage are at risk of developing preeclampsia in later pregnancies.[45]
References
- Ford, Holly B; Schust, Danny J (2009). "Recurrent Pregnancy Loss: Etiology, Diagnosis, and Therapy". Reviews in Obstetrics and Gynecology. 2 (2): 76–83. ISSN 1941-2797. PMC 2709325. PMID 19609401.
- Jeve YB, Davies W (July 2014). "Evidence-based management of recurrent miscarriages". Journal of Human Reproductive Sciences. 7 (3): 159–69. doi:10.4103/0974-1208.142475. PMC 4229790. PMID 25395740.
- "ASRM Patient Fact Sheet: Recurrent Pregnancy Loss". Archived from the original on April 3, 2015. Retrieved April 2, 2015.
- American College of Obstetricians and Gynecologists (ACOG) Repeated Miscarriage FAQ 100 http://www.acog.org/-/media/For-Patients/faq100.pdf?dmc=1&ts=20150820T1255284207 Archived 2018-07-29 at the Wayback Machine
- Royal College of Obstetricians and Gynaecologists (RCOG) (April 2011). "The investigation and treatment of couples with recurrent first-trimester and second-trimester miscarriage" (PDF). Green-top Guideline No. 17. Royal College of Obstetricians and Gynaecologists (RCOG). Archived from the original (PDF) on 5 July 2013. Retrieved 2 July 2013.
- Christiansen, Ole B.; Nybo Andersen, Anne-Marie; Bosch, Ernesto; Daya, Salim; Delves, Peter J.; Hviid, Thomas V.; Kutteh, William H.; Laird, Susan M.; Li, Tin-Chiu; van der Ven, Katrin (2005-04-01). "Evidence-based investigations and treatments of recurrent pregnancy loss". Fertility and Sterility. 83 (4): 821–839. doi:10.1016/j.fertnstert.2004.12.018. ISSN 0015-0282. PMID 15820784.
- Sugiura-Ogasawara, M.; Ozaki, Y.; Katano, K.; Suzumori, N.; Kitaori, T.; Mizutani, E. (2012). "Abnormal embryonic karyotype is the most frequent cause of recurrent miscarriage". Human Reproduction. 27 (8): 2297–2303. doi:10.1093/humrep/des179. ISSN 0268-1161. PMID 22661547.
- "The Investigation and Treatment of Couples with Recurrent Miscarriage: Guideline No 17" (PDF). Royal College of Obstetricians and Gynaecologists. Archived from the original (PDF) on 2013-07-05.
- Branch DW, Gibson M, Silver RM (October 2010). "Clinical practice. Recurrent miscarriage". The New England Journal of Medicine. 363 (18): 1740–7. doi:10.1056/NEJMcp1005330. PMID 20979474.
- "Management of Early Pregnancy Loss". ACOG Practice Bulletin. American College of Obstetricians and Gynecologists. 24 (February). 2001.
- Angell RR (July 1994). "Aneuploidy in older women. Higher rates of aneuploidy in oocytes from older women". Human Reproduction. 9 (7): 1199–200. doi:10.1093/oxfordjournals.humrep.a138675. PMID 7962415.
- MacLennan M, Crichton JH, Playfoot CJ, Adams IR (September 2015). "Oocyte development, meiosis and aneuploidy". Seminars in Cell & Developmental Biology. 45: 68–76. doi:10.1016/j.semcdb.2015.10.005. PMC 4828587. PMID 26454098.
- Infante-Rivard, Claire; Fernández, Alberto; Gauthier, Robert; David, Michèle; Rivard, Georges-Etienne (1993-12-22). "Fetal Loss Associated With Caffeine Intake Before and During Pregnancy". JAMA. 270 (24): 2940–2943. doi:10.1001/jama.1993.03510240052031. ISSN 0098-7484. PMID 8254854.
- Windham, G. C.; Von Behren, J.; Waller, K.; Fenster, L. (1999-02-01). "Exposure to Environmental and Mainstream Tobacco Smoke and Risk of Spontaneous Abortion". American Journal of Epidemiology. 149 (3): 243–247. doi:10.1093/oxfordjournals.aje.a009798. ISSN 0002-9262. PMID 9927219.
- Brandt, Lars P. A.; Nielsen, Claus V. (1992-02-01). "Job Stress and Adverse Outcome of Pregnancy: A Causal Link or Recall Bias?". American Journal of Epidemiology. 135 (3): 302–311. doi:10.1093/oxfordjournals.aje.a116284. ISSN 1476-6256. PMID 1546706.
- Qu, Fan; Wu, Yan; Zhu, Yu-Hang; Barry, John; Ding, Tao; Baio, Gianluca; Muscat, Ruth; Todd, Brenda K.; Wang, Fang-Fang; Hardiman, Paul J. (2017-05-11). "The association between psychological stress and miscarriage: A systematic review and meta-analysis". Scientific Reports. 7 (1): 1731. Bibcode:2017NatSR...7.1731Q. doi:10.1038/s41598-017-01792-3. ISSN 2045-2322. PMC 5431920. PMID 28496110.
- Liddell, H. S.; Pattison, N. S.; Zanderigo, A. (November 1991). "Recurrent Miscarriage - Outcome After Supportive Care in Early Pregnancy". The Australian and New Zealand Journal of Obstetrics and Gynaecology. 31 (4): 320–322. doi:10.1111/j.1479-828x.1991.tb02811.x. ISSN 0004-8666. PMID 1799343. S2CID 9800035.
- Hoffman, p. 181.
- Hoffman, p. 181–182.
- Ali O, Hakimi I, Chanana A, Habib MA, Guelzim K, Kouach J, et al. (2015). "[Term pegnancy on septate uterus: report of a case and review of the literature]". The Pan African Medical Journal. 22: 219. doi:10.11604/pamj.2015.22.219.7790. PMC 4760728. PMID 26955410.
- Choices, NHS (7 December 2017). "Miscarriage - Causes - NHS Choices". www.nhs.uk.
- Alfirevic, Zarko; Stampalija, Tamara; Medley, Nancy (2017). "Cervical stitch (cerclage) for preventing preterm birth in singleton pregnancy". Cochrane Database of Systematic Reviews. 2017 (6): CD008991. doi:10.1002/14651858.CD008991.pub3. ISSN 1465-1858. PMC 6481522. PMID 28586127.
- Rodger MA, Paidas M, McLintock C, Claire M, Middeldorp S, Kahn S, et al. (August 2008). "Inherited thrombophilia and pregnancy complications revisited". Obstetrics and Gynecology. 112 (2 Pt 1): 320–4. doi:10.1097/AOG.0b013e31817e8acc. PMID 18669729.
- Nahas R, Saliba W, Elias A, Elias M (January 2018). "The Prevalence of Thrombophilia in Women With Recurrent Fetal Loss and Outcome of Anticoagulation Therapy for the Prevention of Miscarriages". Clinical and Applied Thrombosis/Hemostasis. 24 (1): 122–128. doi:10.1177/1076029616675967. PMC 6714626. PMID 27799457.
- Williams Z (September 2012). "Inducing tolerance to pregnancy". The New England Journal of Medicine. 367 (12): 1159–61. doi:10.1056/NEJMcibr1207279. PMC 3644969. PMID 22992082.
- Empson M, Lassere M, Craig J, Scott J (April 2005). "Prevention of recurrent miscarriage for women with antiphospholipid antibody or lupus anticoagulant". The Cochrane Database of Systematic Reviews. 2012 (2): CD002859. doi:10.1002/14651858.CD002859.pub2. PMC 6768987. PMID 15846641.
- Patient’s Fact Sheet: Recurrent Pregnancy Lost. American Society for Reproductive Medicine, 8/2008
- van den Boogaard E, Vissenberg R, Land JA, van Wely M, van der Post JA, Goddijn M, et al. (2011). "Significance of (sub)clinical thyroid dysfunction and thyroid autoimmunity before conception and in early pregnancy: a systematic review". Human Reproduction Update. 17 (5): 605–19. doi:10.1093/humupd/dmr024. PMID 21622978.
- Christiansen O (2014). Recurrent pregnancy loss. Chichester, West Sussex, UK: John Wiley & Sons. pp. 29–37. ISBN 9781118749180.
- Nielsen HS (2011). "Secondary recurrent miscarriage and H-Y immunity". Human Reproduction Update. 17 (4): 558–74. doi:10.1093/humupd/dmr005. PMID 21482560.
- Ford HB, Schust DJ (2009). "Recurrent pregnancy loss: etiology, diagnosis, and therapy". Rev Obstet Gynecol. 2 (2): 76–83. PMC 2709325. PMID 19609401.
- Cicinelli E, Matteo M, Tinelli R, Pinto V, Marinaccio M, Indraccolo U, et al. (May 2014). "Chronic endometritis due to common bacteria is prevalent in women with recurrent miscarriage as confirmed by improved pregnancy outcome after antibiotic treatment". Reproductive Sciences. 21 (5): 640–7. doi:10.1177/1933719113508817. PMC 3984485. PMID 24177713.
- Rimmer MP, Fishwick K, Henderson I, Chinn D, Al Wattar BH and Quenby S. Quantifying CD138+ cells in the endometrium to assess chronic endometritis in women at risk of recurrent pregnancy loss: A prospective cohort study and rapid review. J Obstet Gynaecol Res. 2020.
- de Jong PG, Goddijn M, Middeldorp S (2013). "Antithrombotic therapy for pregnancy loss". Human Reproduction Update. 19 (6): 656–73. doi:10.1093/humupd/dmt019. PMID 23766357.
- Stray-Pedersen, Babill; Stray-Pedersen, Sverre (1984-01-15). "Etiologic factors and subsequent reproductive performance in 195 couples with a prior history of habitual abortion". American Journal of Obstetrics and Gynecology. 148 (2): 140–146. doi:10.1016/S0002-9378(84)80164-7. ISSN 0002-9378. PMID 6691389.
- Brigham, S.A.; Conlon, C.; Farquharson, R.G. (November 1999). "A longitudinal study of pregnancy outcome following idiopathic recurrent miscarriage". Human Reproduction. 14 (11): 2868–2871. doi:10.1093/humrep/14.11.2868. ISSN 1460-2350. PMID 10548638.
- Kaandorp SP, Goddijn M, van der Post JA, Hutten BA, Verhoeve HR, Hamulyák K, et al. (April 2010). "Aspirin plus heparin or aspirin alone in women with recurrent miscarriage". The New England Journal of Medicine. 362 (17): 1586–96. doi:10.1056/NEJMoa1000641. PMID 20335572.
- Wong LF, Porter TF, Scott JR (October 2014). "Immunotherapy for recurrent miscarriage". The Cochrane Database of Systematic Reviews. 10 (10): CD000112. doi:10.1002/14651858.CD000112.pub3. PMC 7051032. PMID 25331518.
- Lok, I. H., & Neugebauer, R. (2007). Psychological morbidity following miscarriage. Best Practice & Research Clinical Obstetrics & Gynaecology, 21(2), 229–247.
- Jeve YB, Davies W (July 2014). "Evidence-based management of recurrent miscarriages". Journal of Human Reproductive Sciences. 7 (3): 159–69. doi:10.4103/0974-1208.142475. PMC 4229790. PMID 25395740.
- Oliver-Williams CT, Heydon EE, Smith GC, Wood AM (November 2013). "Miscarriage and future maternal cardiovascular disease: a systematic review and meta-analysis". Heart. 99 (22): 1636–44. doi:10.1136/heartjnl-2012-303237. PMC 3812894. PMID 23539554.
- Braem MG, Onland-Moret NC, Schouten LJ, Kruitwagen RF, Lukanova A, Allen NE, et al. (2012). "Multiple miscarriages are associated with the risk of ovarian cancer: results from the European Prospective Investigation into Cancer and Nutrition". PLOS ONE. 7 (5): e37141. Bibcode:2012PLoSO...737141B. doi:10.1371/journal.pone.0037141. PMC 3356371. PMID 22623987.
- Kessous R, Shoham-Vardi I, Pariente G, Sergienko R, Holcberg G, Sheiner E (October 2014). "Recurrent pregnancy loss: a risk factor for long-term maternal atherosclerotic morbidity?". American Journal of Obstetrics and Gynecology. 211 (4): 414.e1–11. doi:10.1016/j.ajog.2014.05.050. PMID 24905415.
- Coleman PK, Reardon DC, Calhoun BC (August 2013). "Reproductive history patterns and long-term mortality rates: a Danish, population-based record linkage study". European Journal of Public Health. 23 (4): 569–74. doi:10.1093/eurpub/cks107. PMID 22954474.
- Trogstad L, Magnus P, Moffett A, Stoltenberg C (January 2009). "The effect of recurrent miscarriage and infertility on the risk of pre-eclampsia". BJOG. 116 (1): 108–13. doi:10.1111/j.1471-0528.2008.01978.x. PMID 19087081. S2CID 1195813.
Bibliography
- Hoffman, Barbara (2012). Williams gynecology. New York: McGraw-Hill Medical. ISBN 9780071716727.