Retinal vasculitis
Retinal vasculitis is inflammation of the vascular branches of the retinal artery, caused either by primary ocular disease processes, or as a specific presentation of any systemic form of vasculitis such as Behçet's disease, sarcoidosis, multiple sclerosis, or any form of systemic necrotizing vasculitis such as temporal arteritis, polyarteritis nodosa, and granulomatosis with polyangiitis, or due to lupus erythematosus, or rheumatoid arthritis.[1][2] Eales disease, pars planitis, birdshot retinochoroidopathy (autoimmune bilateral posterior uveitis), and Fuchs heterochromic iridocyclitis (FHI) can also cause retinal vasculitis.[1] Infectious pathogens such as Mycobacterium tuberculosis, visceral larva migrans (Toxocara canis & Toxocara cati) can also cause retinal vasculitis.[1] Drug-induced vasculitis may involve retina as well, as seen in methamphetamine induced vasculitis.[3]
| Retinal vasculitis | |
|---|---|
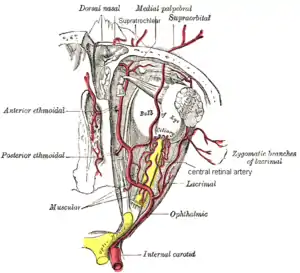 | |
| Retinal artery (at center) | |
| Specialty | Neurology |
Symptoms
Retinal vasculitis presents as painless, decrease of visual acuity (blurry vision), visual floaters, scotomas (dark spot in vision), decreased ability to distinguish colors, and metamorphopsia (distortion of images such as linear images).[1]
Diseases associated with retinal vasculitis
- Behçet's disease
- Common Variable Immune Deficiency[4]
- Eales disease
- Granulomatosis with polyangiitis
- Idiopathic Retinal Vasculitis Aneurysms and Neuroretinitis
- Lupus erythematosus
- Multiple sclerosis
- Polyarteritis nodosa
- Q fever
- Rheumatoid arthritis
- Sarcoidosis
- Temporal arteritis
Diagnosis
Retinal vasculitis is very rare as the only presenting symptom. Often, there is sufficient systemic evidence to help the physician decide between any one of the aforementioned possible systemic diseases. For those patients who present with only vasculitis of the retinal vessels, great investigative effort (Chest X-ray, blood test, urinary analysis, vascular biopsy, ophthalmology assessment, etc.) should be undertaken to ensure that a systemic disease is not the hidden culprit.
Findings
Ophthalmic examination may reveal neovascularization (creation of new vessels in the retina), retinal vessel narrowing, retinal vessel cuffing, retinal hemorrhage, or possible vitritis (inflammation of the vitreous body) or choroiditis (inflammation of the choroid).[1]
Treatment
Intravitreal administration of corticosteroid and immunosuppressants in a case non infectious retinal vasculitis
Antimicrobial therapy is required in the case of infectious retinal vasculitis
Sources
- Lynn K. Gordon, M.D., Ph.D. (January 2003). "Retinal Vasculitis". American Uveitis Society. Archived from the original on July 31, 2010. Retrieved December 10, 2010.
{{cite web}}: CS1 maint: multiple names: authors list (link) - Bolster, Marcy B.; Collier, Virginia U.; Bass, Anne R.; Brasington, Richard D.; Brown, Alan N.; Jonas, Beth; Staudt, Leslie S. (2009). Medical Knowledge Self-Assessment Program (MKSAP-15): Rheumatology. ACP (American College of Physicians). pp. 71–3. ISBN 978-1-934465-30-1.
- Guo, Jingli; Tang, Wenyi; Liu, Wei; Zhang, Yongjin; Wang, Ling; Wang, Wenji (September 2019). "Bilateral methamphetamine-induced ischemic retinopathy". American Journal of Ophthalmology Case Reports. 15: 100473. doi:10.1016/j.ajoc.2019.100473. PMC 6551529. PMID 31194074.
- J. C. van Meurs, S. Lightman, P. W. T. De Waard et al., “Retinal vasculitis occurring with common variable immunodeficiency syndrome,” American Journal of Ophthalmology, vol. 129, no. 2, pp. 269–270, 2000.