Burn
A burn is an injury to skin, or other tissues, caused by heat, cold, electricity, chemicals, friction, or ultraviolet radiation (like sunburn).[5] Most burns are due to heat from hot liquids (called scalding), solids, or fire.[9] Burns occur mainly in the home or the workplace. In the home, risks are associated with domestic kitchens, including stoves, flames, and hot liquids.[6] In the workplace, risks are associated with fire and chemical and electric burns.[6] Alcoholism and smoking are other risk factors.[6] Burns can also occur as a result of self-harm or violence between people (assault).[6]
| Burn | |
|---|---|
 | |
| Second-degree burn of the hand | |
| Specialty | Dermatology Critical care medicine, plastic surgery[1] |
| Symptoms | First degree: Red without blisters[2] Second degree: Blisters and pain[2] Third degree: Area stiff and not painful[2] Fourth degree: Bone and tendon loss[3] |
| Complications | Infection[4] |
| Duration | Days to weeks[2] |
| Types | First degree, Second degree, Third degree,[2] Fourth degree[3] |
| Causes | Heat, cold, electricity, chemicals, friction, radiation[5] |
| Risk factors | Open cooking fires, unsafe cook stoves, smoking, alcoholism, dangerous work environment[6] |
| Treatment | Depends on the severity[2] |
| Medication | Pain medication, intravenous fluids, tetanus toxoid[2] |
| Frequency | 67 million (2015)[7] |
| Deaths | 176,000 (2015)[8] |
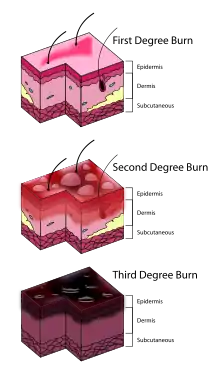
Burns that affect only the superficial skin layers are known as superficial or first-degree burns.[2][10] They appear red without blisters and pain typically lasts around three days.[2][10] When the injury extends into some of the underlying skin layer, it is a partial-thickness or second-degree burn.[2] Blisters are frequently present and they are often very painful.[2] Healing can require up to eight weeks and scarring may occur.[2] In a full-thickness or third-degree burn, the injury extends to all layers of the skin.[2] Often there is no pain and the burnt area is stiff.[2] Healing typically does not occur on its own.[2] A fourth-degree burn additionally involves injury to deeper tissues, such as muscle, tendons, or bone.[2] The burn is often black and frequently leads to loss of the burned part.[2][11]
Burns are generally preventable.[6] Treatment depends on the severity of the burn.[2] Superficial burns may be managed with little more than simple pain medication, while major burns may require prolonged treatment in specialized burn centers.[2] Cooling with tap water may help pain and decrease damage; however, prolonged cooling may result in low body temperature.[2][10] Partial-thickness burns may require cleaning with soap and water, followed by dressings.[2] It is not clear how to manage blisters, but it is probably reasonable to leave them intact if small and drain them if large.[2] Full-thickness burns usually require surgical treatments, such as skin grafting.[2] Extensive burns often require large amounts of intravenous fluid, due to capillary fluid leakage and tissue swelling.[10] The most common complications of burns involve infection.[4] Tetanus toxoid should be given if not up to date.[2]
In 2015, fire and heat resulted in 67 million injuries.[7] This resulted in about 2.9 million hospitalizations and 176,000 deaths.[8][12] Among women in much of the world, burns are most commonly related to the use of open cooking fires or unsafe cook stoves.[6] Among men, they are more likely a result of unsafe workplace conditions.[6] Most deaths due to burns occur in the developing world, particularly in Southeast Asia.[6] While large burns can be fatal, treatments developed since 1960 have improved outcomes, especially in children and young adults.[13] In the United States, approximately 96% of those admitted to a burn center survive their injuries.[14] The long-term outcome is related to the size of burn and the age of the person affected.[2]
Signs and symptoms
The characteristics of a burn depend upon its depth. Superficial burns cause pain lasting two or three days, followed by peeling of the skin over the next few days.[10][15] Individuals with more severe burns may indicate discomfort or complain of feeling pressure rather than pain. Full-thickness burns may be entirely insensitive to light touch or puncture.[15] While superficial burns are typically red in color, severe burns may be pink, white or black.[15] Burns around the mouth or singed hair inside the nose may indicate that burns to the airways have occurred, but these findings are not definitive.[16] More worrisome signs include: shortness of breath, hoarseness, and stridor or wheezing.[16] Itchiness is common during the healing process, occurring in up to 90% of adults and nearly all children.[17] Numbness or tingling may persist for a prolonged period of time after an electrical injury.[18] Burns may also produce emotional and psychological distress.[19]
| Type[2] | Layers involved | Appearance | Texture | Sensation | Healing Time | Prognosis and Complications | Example |
|---|---|---|---|---|---|---|---|
| Superficial (first-degree) | Epidermis[10] | Red without blisters[2] | Dry | Painful[2] | 5–10 days[2][20] | Heals well.[2] |  |
| Superficial partial thickness (second-degree) | Extends into superficial (papillary) dermis[2] | Redness with clear blister.[2] Blanches with pressure.[2] | Moist[2] | Very painful[2] | 2–3 weeks[2][15] | Local infection (cellulitis) but no scarring typically[15] |
|
| Deep partial thickness (second-degree) | Extends into deep (reticular) dermis[2] | Yellow or white. Less blanching. May be blistering.[2] | Fairly dry[15] | Pressure and discomfort[15] | 3–8 weeks[2] | Scarring, contractures (may require excision and skin grafting)[15] |  |
| Full thickness (third-degree) | Extends through entire dermis[2] | Stiff and white/brown.[2] No blanching.[15] | Leathery[2] | Painless[2] | Prolonged (months) and unfinished/incomplete[2] | Scarring, contractures, amputation (early excision recommended)[15] |  |
| Fourth-degree | Extends through entire skin, and into underlying fat, muscle and bone[2] | Black; charred with eschar | Dry | Painless | Does not heal; Requires excision[2] | Amputation, significant functional impairment and, in some cases, death.[2] |  |
Cause
Burns are caused by a variety of external sources classified as thermal (heat-related), chemical, electrical, and radiation.[21] In the United States, the most common causes of burns are: fire or flame (44%), scalds (33%), hot objects (9%), electricity (4%), and chemicals (3%).[22] Most (69%) burn injuries occur at home or at work (9%),[14] and most are accidental, with 2% due to assault by another, and 1–2% resulting from a suicide attempt.[19] These sources can cause inhalation injury to the airway and/or lungs, occurring in about 6%.[4]
Burn injuries occur more commonly among the poor.[19] Smoking and alcoholism are other risk factors.[9] Fire-related burns are generally more common in colder climates.[19] Specific risk factors in the developing world include cooking with open fires or on the floor[5] as well as developmental disabilities in children and chronic diseases in adults.[23]
Thermal
In the United States, fire and hot liquids are the most common causes of burns.[4] Of house fires that result in death, smoking causes 25% and heating devices cause 22%.[5] Almost half of injuries are due to efforts to fight a fire.[5] Scalding is caused by hot liquids or gases and most commonly occurs from exposure to hot drinks, high temperature tap water in baths or showers, hot cooking oil, or steam.[25] Scald injuries are most common in children under the age of five[2] and, in the United States and Australia, this population makes up about two-thirds of all burns.[4] Contact with hot objects is the cause of about 20–30% of burns in children.[4] Generally, scalds are first- or second-degree burns, but third-degree burns may also result, especially with prolonged contact.[26] Fireworks are a common cause of burns during holiday seasons in many countries.[27] This is a particular risk for adolescent males.[28] In the United States, for non-fatal burn injuries, white males, aged <6 comprise most cases.[29] Thermal burns from grabbing/touching and spilling/splashing were the most common type of burn and mechanism, while the bodily areas most impacted were hands and fingers followed by head/neck.[29]
Chemical
Chemical burns can be caused by over 25,000 substances,[2] most of which are either a strong base (55%) or a strong acid (26%).[30] Most chemical burn deaths are secondary to ingestion.[2] Common agents include: sulfuric acid as found in toilet cleaners, sodium hypochlorite as found in bleach, and halogenated hydrocarbons as found in paint remover, among others.[2] Hydrofluoric acid can cause particularly deep burns that may not become symptomatic until some time after exposure.[31] Formic acid may cause the breakdown of significant numbers of red blood cells.[16]
Electrical
Electrical burns or injuries are classified as high voltage (greater than or equal to 1000 volts), low voltage (less than 1000 volts), or as flash burns secondary to an electric arc.[2] The most common causes of electrical burns in children are electrical cords (60%) followed by electrical outlets (14%).[4][32] Lightning may also result in electrical burns.[33] Risk factors for being struck include involvement in outdoor activities such as mountain climbing, golf and field sports, and working outside.[18] Mortality from a lightning strike is about 10%.[18]
While electrical injuries primarily result in burns, they may also cause fractures or dislocations secondary to blunt force trauma or muscle contractions.[18] In high voltage injuries, most damage may occur internally and thus the extent of the injury cannot be judged by examination of the skin alone.[18] Contact with either low voltage or high voltage may produce cardiac arrhythmias or cardiac arrest.[18]
Radiation
Radiation burns may be caused by protracted exposure to ultraviolet light (such as from the sun, tanning booths or arc welding) or from ionizing radiation (such as from radiation therapy, X-rays or radioactive fallout).[34] Sun exposure is the most common cause of radiation burns and the most common cause of superficial burns overall.[35] There is significant variation in how easily people sunburn based on their skin type.[36] Skin effects from ionizing radiation depend on the amount of exposure to the area, with hair loss seen after 3 Gy, redness seen after 10 Gy, wet skin peeling after 20 Gy, and necrosis after 30 Gy.[37] Redness, if it occurs, may not appear until some time after exposure.[37] Radiation burns are treated the same as other burns.[37] Microwave burns occur via thermal heating caused by the microwaves.[38] While exposures as short as two seconds may cause injury, overall this is an uncommon occurrence.[38]
Non-accidental
In those hospitalized from scalds or fire burns, 3–10% are from assault.[39] Reasons include: child abuse, personal disputes, spousal abuse, elder abuse, and business disputes.[39] An immersion injury or immersion scald may indicate child abuse.[26] It is created when an extremity, or sometimes the buttocks are held under the surface of hot water.[26] It typically produces a sharp upper border and is often symmetrical,[26] known as "sock burns", "glove burns", or "zebra stripes" - where folds have prevented certain areas from burning.[40] Deliberate cigarette burns most often found on the face, or the back of the hands and feet.[40] Other high-risk signs of potential abuse include: circumferential burns, the absence of splash marks, a burn of uniform depth, and association with other signs of neglect or abuse.[41]
Bride burning, a form of domestic violence, occurs in some cultures, such as India where women have been burned in revenge for what the husband or his family consider an inadequate dowry.[42][43] In Pakistan, acid burns represent 13% of intentional burns, and are frequently related to domestic violence.[41] Self-immolation (setting oneself on fire) is also used as a form of protest in various parts of the world.[19]
Pathophysiology
At temperatures greater than 44 °C (111 °F), proteins begin losing their three-dimensional shape and start breaking down.[44] This results in cell and tissue damage.[2] Many of the direct health effects of a burn are caused by failure of the skin to perform its normal functions, which include: protection from bacteria, skin sensation, body temperature regulation, and prevention of evaporation of the body's water. Disruption of these functions can lead to infection, loss of skin sensation, hypothermia, and hypovolemic shock via dehydration (i.e. water in the body evaporated away).[2] Disruption of cell membranes causes cells to lose potassium to the spaces outside the cell and to take up water and sodium.[2]
In large burns (over 30% of the total body surface area), there is a significant inflammatory response.[45] This results in increased leakage of fluid from the capillaries,[16] and subsequent tissue edema.[2] This causes overall blood volume loss, with the remaining blood suffering significant plasma loss, making the blood more concentrated.[2] Poor blood flow to organs like the kidneys and gastrointestinal tract may result in kidney failure and stomach ulcers.[46]
Increased levels of catecholamines and cortisol can cause a hypermetabolic state that can last for years.[45] This is associated with increased cardiac output, metabolism, a fast heart rate, and poor immune function.[45]
Diagnosis
Burns can be classified by depth, mechanism of injury, extent, and associated injuries. The most commonly used classification is based on the depth of injury. The depth of a burn is usually determined via examination, although a biopsy may also be used.[2] It may be difficult to accurately determine the depth of a burn on a single examination and repeated examinations over a few days may be necessary.[16] In those who have a headache or are dizzy and have a fire-related burn, carbon monoxide poisoning should be considered.[47] Cyanide poisoning should also be considered.[16]
Size
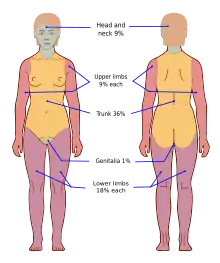
The size of a burn is measured as a percentage of total body surface area (TBSA) affected by partial thickness or full thickness burns.[2] First-degree burns that are only red in color and are not blistering are not included in this estimation.[2] Most burns (70%) involve less than 10% of the TBSA.[4]
There are a number of methods to determine the TBSA, including the Wallace rule of nines, Lund and Browder chart, and estimations based on a person's palm size.[10] The rule of nines is easy to remember but only accurate in people over 16 years of age.[10] More accurate estimates can be made using Lund and Browder charts, which take into account the different proportions of body parts in adults and children.[10] The size of a person's handprint (including the palm and fingers) is approximately 1% of their TBSA.[10]
Severity
| Minor | Moderate | Major |
|---|---|---|
| Adult <10% TBSA | Adult 10–20% TBSA | Adult >20% TBSA |
| Young or old < 5% TBSA | Young or old 5–10% TBSA | Young or old >10% TBSA |
| <2% full thickness burn | 2–5% full thickness burn | >5% full thickness burn |
| High voltage injury | High voltage burn | |
| Possible inhalation injury | Known inhalation injury | |
| Circumferential burn | Significant burn to face, joints, hands, or feet | |
| Other health problems | Associated injuries |
To determine the need for referral to a specialized burn unit, the American Burn Association devised a classification system. Under this system, burns can be classified as major, moderate, and minor. This is assessed based on a number of factors, including total body surface area affected, the involvement of specific anatomical zones, the age of the person, and associated injuries.[47] Minor burns can typically be managed at home, moderate burns are often managed in a hospital, and major burns are managed by a burn center.[47] Severe burn injury represents one of the most devastating forms of trauma.[48] Despite improvements in burn care, patients can be left to suffer for as many as three years post-injury.[49]
Signs of smoke inhalation
Signs of smoke inhalation includes hoarse voice, dyspnea, facial burns, singed nasal hairs, sputum which contains carbonaceous materials, Stridor and wheezing may be present in later stages.[50]
Prevention
Historically, about half of all burns were deemed preventable.[5] Burn prevention programs have significantly decreased rates of serious burns.[44] Preventive measures include: limiting hot water temperatures, smoke alarms, sprinkler systems, proper construction of buildings, and fire-resistant clothing.[5] Experts recommend setting water heaters below 48.8 °C (119.8 °F).[4] Other measures to prevent scalds include using a thermometer to measure bath water temperatures, and splash guards on stoves.[44] While the effect of the regulation of fireworks is unclear, there is tentative evidence of benefit[51] with recommendations including the limitation of the sale of fireworks to children.[4]
Management
Resuscitation begins with the assessment and stabilization of the person's airway, breathing and circulation.[10] If inhalation injury is suspected, early intubation may be required.[16] This is followed by care of the burn wound itself. People with extensive burns may be wrapped in clean sheets until they arrive at a hospital.[16] As burn wounds are prone to infection, a tetanus booster shot should be given if an individual has not been immunized within the last five years.[52] In the United States, 95% of burns that present to the emergency department are treated and discharged; 5% require hospital admission.[19] With major burns, early feeding is important.[45] Protein intake should also be increased, and trace elements and vitamins are often required.[53] Hyperbaric oxygenation may be useful in addition to traditional treatments.[54]
Intravenous fluids
In those with poor tissue perfusion, boluses of isotonic crystalloid solution should be given.[10] In children with more than 10–20% TBSA (Total Body Surface Area) burns, and adults with more than 15% TBSA burns, formal fluid resuscitation and monitoring should follow.[10][55][56] This should be begun pre-hospital if possible in those with burns greater than 25% TBSA.[55] The Parkland formula can help determine the volume of intravenous fluids required over the first 24 hours. The formula is based on the affected individual's TBSA and weight. Half of the fluid is administered over the first 8 hours, and the remainder over the following 16 hours. The time is calculated from when the burn occurred, and not from the time that fluid resuscitation began. Children require additional maintenance fluid that includes glucose.[16] Additionally, those with inhalation injuries require more fluid.[57] While inadequate fluid resuscitation may cause problems, over-resuscitation can also be detrimental.[58] The formulas are only a guide, with infusions ideally tailored to a urinary output of >30 mL/h in adults or >1mL/kg in children and mean arterial pressure greater than 60 mmHg.[16]
While lactated Ringer's solution is often used, there is no evidence that it is superior to normal saline.[10] Crystalloid fluids appear just as good as colloid fluids, and as colloids are more expensive they are not recommended.[59][60] Blood transfusions are rarely required.[2] They are typically only recommended when the hemoglobin level falls below 60-80 g/L (6-8 g/dL)[61] due to the associated risk of complications.[16] Intravenous catheters may be placed through burned skin if needed or intraosseous infusions may be used.[16]
Wound care
Early cooling (within 30 minutes of the burn) reduces burn depth and pain, but care must be taken as over-cooling can result in hypothermia.[2][10] It should be performed with cool water 10–25 °C (50.0–77.0 °F) and not ice water as the latter can cause further injury.[10][44] Chemical burns may require extensive irrigation.[2] Cleaning with soap and water, removal of dead tissue, and application of dressings are important aspects of wound care. If intact blisters are present, it is not clear what should be done with them. Some tentative evidence supports leaving them intact. Second-degree burns should be re-evaluated after two days.[44]
In the management of first and second-degree burns, little quality evidence exists to determine which dressing type to use.[62] It is reasonable to manage first-degree burns without dressings.[44] While topical antibiotics are often recommended, there is little evidence to support their use.[63][64] Silver sulfadiazine (a type of antibiotic) is not recommended as it potentially prolongs healing time.[62][65] There is insufficient evidence to support the use of dressings containing silver[66] or negative-pressure wound therapy.[67] Silver sulfadiazine does not appear to differ from silver containing foam dressings with respect to healing.[68]
Medications
Burns can be very painful and a number of different options may be used for pain management. These include simple analgesics (such as ibuprofen and acetaminophen) and opioids such as morphine. Benzodiazepines may be used in addition to analgesics to help with anxiety.[44] During the healing process, antihistamines, massage, or transcutaneous nerve stimulation may be used to aid with itching.[17] Antihistamines, however, are only effective for this purpose in 20% of people.[69] There is tentative evidence supporting the use of gabapentin[17] and its use may be reasonable in those who do not improve with antihistamines.[70] Intravenous lidocaine requires more study before it can be recommended for pain.[71]
Intravenous antibiotics are recommended before surgery for those with extensive burns (>60% TBSA).[72] As of 2008, guidelines do not recommend their general use due to concerns regarding antibiotic resistance[63] and the increased risk of fungal infections.[16] Tentative evidence, however, shows that they may improve survival rates in those with large and severe burns.[63] Erythropoietin has not been found effective to prevent or treat anemia in burn cases.[16] In burns caused by hydrofluoric acid, calcium gluconate is a specific antidote and may be used intravenously and/or topically.[31] Recombinant human growth hormone (rhGH) in those with burns that involve more than 40% of their body appears to speed healing without affecting the risk of death.[73] The use of steroids is of unclear evidence.[74]
Allogeneic cultured keratinocytes and dermal fibroblasts in murine collagen (Stratagraft) was approved for medical use in the United States in June 2021.[75]
Surgery
Wounds requiring surgical closure with skin grafts or flaps (typically anything more than a small full thickness burn) should be dealt with as early as possible.[76] Circumferential burns of the limbs or chest may need urgent surgical release of the skin, known as an escharotomy.[77] This is done to treat or prevent problems with distal circulation, or ventilation.[77] It is uncertain if it is useful for neck or digit burns.[77] Fasciotomies may be required for electrical burns.[77]
Skin grafts can involve temporary skin substitutes, derived from animal (human donor or pig) skin or synthesized. They are used to cover the wound as a dressing, preventing infection and fluid loss, but will eventually need to be removed. Alternatively, human skin can be treated to be left on permanently without rejection.[78]
There is no evidence that the use of copper sulphate to visualise phosphorus particles for removal can help with wound healing due to phosphorus burns. Meanwhile, absorption of copper sulphate into the blood circulation can be harmful.[79]
Alternative medicine
Honey has been used since ancient times to aid wound healing and may be beneficial in first- and second-degree burns.[80] There is moderate evidence that honey helps heal partial thickness burns.[81][82] The evidence for aloe vera is of poor quality.[83] While it might be beneficial in reducing pain,[20] and a review from 2007 found tentative evidence of improved healing times,[84] a subsequent review from 2012 did not find improved healing over silver sulfadiazine.[83] There were only three randomized controlled trials for the use of plants for burns, two for aloe vera and one for oatmeal.[85]
There is little evidence that vitamin E helps with keloids or scarring.[86] Butter is not recommended.[87] In low income countries, burns are treated up to one-third of the time with traditional medicine, which may include applications of eggs, mud, leaves or cow dung.[23] Surgical management is limited in some cases due to insufficient financial resources and availability.[23] There are a number of other methods that may be used in addition to medications to reduce procedural pain and anxiety including: virtual reality therapy, hypnosis, and behavioral approaches such as distraction techniques.[70]
Patient support
Burn patients require support and care – both physiological and psychological. Respiratory failure, sepsis, and multi-organ system failure are common in hospitalized burn patients. To prevent hypothermia and maintain normal body temperature, burn patients with over 20% of burn injuries should be kept in an environment with the temperature at or above 30 degree Celsius.[88]
Metabolism in burn patients proceeds at a higher than normal speed due to the whole-body process and rapid fatty acid substrate cycles, which can be countered with an adequate supply of energy, nutrients, and antioxidants. Enteral feeding a day after resuscitation is required to reduce risk of infection, recovery time, non-infectious complications, hospital stay, long-term damage, and mortality. Controlling blood glucose levels can have an impact on liver function and survival.
Risk of thromboembolism is high and acute respiratory distress syndrome (ARDS) that does not resolve with maximal ventilator use is also a common complication. Scars are long-term after-effects of a burn injury. Psychological support is required to cope with the aftermath of a fire accident, while to prevent scars and long-term damage to the skin and other body structures consulting with burn specialists, preventing infections, consuming nutritious foods, early and aggressive rehabilitation, and using compressive clothing are recommended.
Prognosis
| TBSA | Mortality |
|---|---|
| 0–9% | 0.6% |
| 10–19% | 2.9% |
| 20–29% | 8.6% |
| 30–39% | 16% |
| 40–49% | 25% |
| 50–59% | 37% |
| 60–69% | 43% |
| 70–79% | 57% |
| 80–89% | 73% |
| 90–100% | 85% |
| Inhalation | 23% |
The prognosis is worse in those with larger burns, those who are older, and females.[2] The presence of a smoke inhalation injury, other significant injuries such as long bone fractures, and serious co-morbidities (e.g. heart disease, diabetes, psychiatric illness, and suicidal intent) also influence prognosis.[2] On average, of those admitted to the United States burn centers, 4% die,[4] with the outcome for individuals dependent on the extent of the burn injury. For example, admittees with burn areas less than 10% TBSA had a mortality rate of less than 1%, while admittees with over 90% TBSA had a mortality rate of 85%.[89] In Afghanistan, people with more than 60% TBSA burns rarely survive.[4] The Baux score has historically been used to determine prognosis of major burns. However, with improved care, it is no longer very accurate.[16] The score is determined by adding the size of the burn (% TBSA) to the age of the person and taking that to be more or less equal to the risk of death.[16] Burns in 2013 resulted in 1.2 million years lived with disability and 12.3 million disability adjusted life years.[12]
Complications
A number of complications may occur, with infections being the most common.[4] In order of frequency, potential complications include: pneumonia, cellulitis, urinary tract infections and respiratory failure.[4] Risk factors for infection include: burns of more than 30% TBSA, full-thickness burns, extremes of age (young or old), or burns involving the legs or perineum.[90] Pneumonia occurs particularly commonly in those with inhalation injuries.[16]
Anemia secondary to full thickness burns of greater than 10% TBSA is common.[10] Electrical burns may lead to compartment syndrome or rhabdomyolysis due to muscle breakdown.[16] Blood clotting in the veins of the legs is estimated to occur in 6 to 25% of people.[16] The hypermetabolic state that may persist for years after a major burn can result in a decrease in bone density and a loss of muscle mass.[45] Keloids may form subsequent to a burn, particularly in those who are young and dark skinned.[86] Following a burn, children may have significant psychological trauma and experience post-traumatic stress disorder.[91] Scarring may also result in a disturbance in body image.[91] To treat hypertrophic scars (raised, tense, stiff and itchy scars) and limit their effect on physical function and everyday activities, silicone sheeting and compression garments are recommended.[92][93][94] In the developing world, significant burns may result in social isolation, extreme poverty and child abandonment.[19]
Epidemiology

|
no data
< 50
50–100
100–150
150–200
200–250
250–300 |
300–350
350–400
400–450
450–500
500–600
> 600
|
In 2015 fire and heat resulted in 67 million injuries.[7] This resulted in about 2.9 million hospitalizations and 238,000 dying.[12] This is down from 300,000 deaths in 1990.[96] This makes it the fourth leading cause of injuries after motor vehicle collisions, falls, and violence.[19] About 90% of burns occur in the developing world.[19] This has been attributed partly to overcrowding and an unsafe cooking situation.[19] Overall, nearly 60% of fatal burns occur in Southeast Asia with a rate of 11.6 per 100,000.[4] The number of fatal burns has changed from 280,000 in 1990 to 176,000 in 2015.[97][8]
In the developed world, adult males have twice the mortality as females from burns. This is most probably due to their higher risk occupations and greater risk-taking activities. In many countries in the developing world, however, females have twice the risk of males. This is often related to accidents in the kitchen or domestic violence.[19] In children, deaths from burns occur at more than ten times the rate in the developing than the developed world.[19] Overall, in children it is one of the top fifteen leading causes of death.[5] From the 1980s to 2004, many countries have seen both a decrease in the rates of fatal burns and in burns generally.[19]
Developed countries
An estimated 500,000 burn injuries receive medical treatment yearly in the United States.[44] They resulted in about 3,300 deaths in 2008.[5] Most burns (70%) and deaths from burns occur in males.[2][14] The highest incidence of fire burns occurs in those 18–35 years old, while the highest incidence of scalds occurs in children less than five years old and adults over 65.[2] Electrical burns result in about 1,000 deaths per year.[98] Lightning results in the death of about 60 people a year.[18] In Europe, intentional burns occur most commonly in middle aged men.[39]
Developing countries
In India, about 700,000 to 800,000 people per year sustain significant burns, though very few are looked after in specialist burn units.[99] The highest rates occur in women 16–35 years of age.[99] Part of this high rate is related to unsafe kitchens and loose-fitting clothing typical to India.[99] It is estimated that one-third of all burns in India are due to clothing catching fire from open flames.[100] Intentional burns are also a common cause and occur at high rates in young women, secondary to domestic violence and self-harm.[19][39]
History

Cave paintings from more than 3,500 years ago document burns and their management.[13] The earliest Egyptian records on treating burns describes dressings prepared with milk from mothers of baby boys,[101] and the 1500 BCE Edwin Smith Papyrus describes treatments using honey and the salve of resin.[13] Many other treatments have been used over the ages, including the use of tea leaves by the Chinese documented to 600 BCE, pig fat and vinegar by Hippocrates documented to 400 BCE, and wine and myrrh by Celsus documented to the 1st century CE.[13] French barber-surgeon Ambroise Paré was the first to describe different degrees of burns in the 1500s.[102] Guillaume Dupuytren expanded these degrees into six different severities in 1832.[13][103]
The first hospital to treat burns opened in 1843 in London, England, and the development of modern burn care began in the late 1800s and early 1900s.[13][102] During World War I, Henry D. Dakin and Alexis Carrel developed standards for the cleaning and disinfecting of burns and wounds using sodium hypochlorite solutions, which significantly reduced mortality.[13] In the 1940s, the importance of early excision and skin grafting was acknowledged, and around the same time, fluid resuscitation and formulas to guide it were developed.[13] In the 1970s, researchers demonstrated the significance of the hypermetabolic state that follows large burns.[13]
References
Citations
- "Burns - British Association of Plastic Reconstructive and Aesthetic Surgeons". BAPRAS.
- Tintinalli, Judith E. (2010). Emergency Medicine: A Comprehensive Study Guide (Emergency Medicine (Tintinalli)). New York: McGraw-Hill Companies. pp. 1374–1386. ISBN 978-0-07-148480-0.
- Singer A (June 2007). "Management of local burn wounds in the ED". The American Journal of Emergency Medicine. 25 (6): 666–671. doi:10.1016/j.ajem.2006.12.008. PMID 17606093.
- Herndon D, ed. (2012). "Chapter 3: Epidemiological, Demographic, and Outcome Characteristics of Burn Injury". Total burn care (4th ed.). Edinburgh: Saunders. p. 23. ISBN 978-1-4377-2786-9.
- Herndon D, ed. (2012). "Chapter 4: Prevention of Burn Injuries". Total burn care (4th ed.). Edinburgh: Saunders. p. 46. ISBN 978-1-4377-2786-9.
- "Burns". World Health Organization. September 2016. Archived from the original on 21 July 2017. Retrieved 1 August 2017.
- Vos T, Allen C, Arora M, Barber RM, Bhutta ZA, Brown A, et al. (October 2016). "Global, regional, and national incidence, prevalence, and years lived with disability for 310 diseases and injuries, 1990-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1545–1602. doi:10.1016/S0140-6736(16)31678-6. PMC 5055577. PMID 27733282.
- Wang H, Naghavi M, Allen C, Barber R, Bhutta Z, Carter A, et al. (October 2016). "Global, regional, and national life expectancy, all-cause mortality, and cause-specific mortality for 249 causes of death, 1980-2015: a systematic analysis for the Global Burden of Disease Study 2015". Lancet. 388 (10053): 1459–1544. doi:10.1016/S0140-6736(16)31012-1. PMC 5388903. PMID 27733281.
- "Burns Fact sheet N°365". WHO. April 2014. Archived from the original on 10 November 2015. Retrieved 3 March 2016.
- Granger J (January 2009). "An Evidence-Based Approach to Pediatric Burns". Pediatric Emergency Medicine Practice. 6 (1). Archived from the original on 17 October 2013.
- Ferri, Fred F. (2012). Ferri's netter patient advisor (2nd ed.). Philadelphia, PA: Saunders. p. 235. ISBN 9781455728268. Archived from the original on 21 December 2016.
- Haagsma JA, Graetz N, Bolliger I, Naghavi M, Higashi H, Mullany EC, et al. (February 2016). "The global burden of injury: incidence, mortality, disability-adjusted life years and time trends from the Global Burden of Disease study 2013". Injury Prevention. 22 (1): 3–18. doi:10.1136/injuryprev-2015-041616. PMC 4752630. PMID 26635210.
- Herndon D, ed. (2012). "Chapter 1: A Brief History of Acute Burn Care Management". Total burn care (4th ed.). Edinburgh: Saunders. p. 1. ISBN 978-1-4377-2786-9.
- "Burn Incidence and Treatment in the United States: 2012 Fact Sheet". American Burn Association. 2012. Archived from the original on 21 February 2013. Retrieved 20 April 2013.
- Herndon D, ed. (2012). "Chapter 10: Evaluation of the burn wound: management decisions". Total burn care (4th ed.). Edinburgh: Saunders. p. 127. ISBN 978-1-4377-2786-9.
- Brunicardi C (2010). "Chapter 8: Burns". Schwartz's principles of surgery (9th ed.). New York: McGraw-Hill, Medical Pub. Division. ISBN 978-0-07-154769-7.
- Goutos I, Dziewulski P, Richardson PM (March–April 2009). "Pruritus in burns: review article". Journal of Burn Care & Research. 30 (2): 221–8. doi:10.1097/BCR.0b013e318198a2fa. PMID 19165110. S2CID 3679902.
- Marx J (2010). "Chapter 140: Electrical and Lightning Injuries". Rosen's emergency medicine : concepts and clinical practice (7th ed.). Philadelphia: Mosby/Elsevier. ISBN 978-0-323-05472-0.
- Peck MD (November 2011). "Epidemiology of burns throughout the world. Part I: Distribution and risk factors". Burns. 37 (7): 1087–100. doi:10.1016/j.burns.2011.06.005. PMID 21802856.
- Lloyd EC, Rodgers BC, Michener M, Williams MS (January 2012). "Outpatient burns: prevention and care". American Family Physician. 85 (1): 25–32. PMID 22230304.
- Rosdahl CB, Kowalski MT (2008). Textbook of basic nursing (9th ed.). Philadelphia: Lippincott Williams & Wilkins. p. 1109. ISBN 978-0-7817-6521-3. Archived from the original on 12 May 2016.
- National Burn Repository Pg. i
- Forjuoh SN (August 2006). "Burns in low- and middle-income countries: a review of available literature on descriptive epidemiology, risk factors, treatment, and prevention". Burns. 32 (5): 529–37. doi:10.1016/j.burns.2006.04.002. PMID 16777340.
- "Fire death rates". Our World in Data. Retrieved 17 November 2019.
- Eisen S, Murphy C (2009). Murphy C, Gardiner M, Eisen S (eds.). Training in paediatrics : the essential curriculum. Oxford: Oxford University Press. p. 36. ISBN 978-0-19-922773-0. Archived from the original on 25 April 2016.
- Maguire S, Moynihan S, Mann M, Potokar T, Kemp AM (December 2008). "A systematic review of the features that indicate intentional scalds in children". Burns. 34 (8): 1072–81. doi:10.1016/j.burns.2008.02.011. PMID 18538478.
- Peden M (2008). World report on child injury prevention. Geneva, Switzerland: World Health Organization. p. 86. ISBN 978-92-4-156357-4. Archived from the original on 24 April 2016.
- World Health Organization. "World report on child injury prevention" (PDF). Archived (PDF) from the original on 31 May 2013.
- Mitchell M, Kistamgari S, Chounthirath T, McKenzie LB, Smith GA (January 2020). "Children Younger Than 18 Years Treated for Nonfatal Burns in US Emergency Departments". Clinical Pediatrics. 59 (1): 34–44. doi:10.1177/0009922819884568. PMID 31672059. S2CID 207816299.
- Hardwicke J, Hunter T, Staruch R, Moiemen N (May 2012). "Chemical burns--an historical comparison and review of the literature". Burns. 38 (3): 383–7. doi:10.1016/j.burns.2011.09.014. PMID 22037150.
- Makarovsky I, Markel G, Dushnitsky T, Eisenkraft A (May 2008). "Hydrogen fluoride--the protoplasmic poison". The Israel Medical Association Journal. 10 (5): 381–5. PMID 18605366.
- Nasoori, A.; Hoomand, R. (2017). "Maggot debridement therapy for an electrical burn injury with instructions for the use of Lucilia sericata larvae". Journal of Wound Care. 26 (12): 734–741. doi:10.12968/jowc.2017.26.12.734. PMID 29244970.
- Edlich RF, Farinholt HM, Winters KL, Britt LD, Long WB (2005). "Modern concepts of treatment and prevention of lightning injuries". Journal of Long-Term Effects of Medical Implants. 15 (2): 185–96. doi:10.1615/jlongtermeffmedimplants.v15.i2.60. PMID 15777170.
- Prahlow J (2010). Forensic pathology for police, death investigators, and forensic scientists. Totowa, N.J.: Humana. p. 485. ISBN 978-1-59745-404-9. Archived from the original on 20 May 2016.
- Kearns RD, Cairns CB, Holmes JH, Rich PB, Cairns BA (January 2013). "Thermal burn care: a review of best practices. What should prehospital providers do for these patients?". EMS World. 42 (1): 43–51. PMID 23393776.
- Balk SJ (March 2011). "Ultraviolet radiation: a hazard to children and adolescents". Pediatrics. 127 (3): e791-817. doi:10.1542/peds.2010-3502. PMID 21357345.
- Marx J (2010). "Chapter 144: Radiation Injuries". Rosen's emergency medicine : concepts and clinical practice (7th ed.). Philadelphia: Mosby/Elsevier. ISBN 978-0-323-05472-0.
- Krieger J (2001). Clinical environmental health and toxic exposures (2nd ed.). Philadelphia, Pa. [u.a.]: Lippincott Williams & Wilkins. p. 205. ISBN 978-0-683-08027-8. Archived from the original on 5 May 2016.
- Peck MD (August 2012). "Epidemiology of burns throughout the World. Part II: intentional burns in adults". Burns. 38 (5): 630–7. doi:10.1016/j.burns.2011.12.028. PMID 22325849.
- Gondim RM, Muñoz DR, Petri V (June 2011). "Child abuse: skin markers and differential diagnosis". Anais Brasileiros de Dermatologia. 86 (3): 527–36. doi:10.1590/S0365-05962011000300015. PMID 21738970.
- Herndon D, ed. (2012). "Chapter 61: Intential burn injuries". Total burn care (4th ed.). Edinburgh: Saunders. pp. 689–698. ISBN 978-1-4377-2786-9.
- Jutla RK, Heimbach D (March–April 2004). "Love burns: An essay about bride burning in India". The Journal of Burn Care & Rehabilitation. 25 (2): 165–70. doi:10.1097/01.bcr.0000111929.70876.1f. PMID 15091143.
- Peden M (2008). World report on child injury prevention. Geneva, Switzerland: World Health Organization. p. 82. ISBN 978-92-4-156357-4. Archived from the original on 17 June 2016.
- Marx J (2010). "Chapter 60: Thermal Burns". Rosen's emergency medicine : concepts and clinical practice (7th ed.). Philadelphia: Mosby/Elsevier. ISBN 978-0-323-05472-0.
- Rojas Y, Finnerty CC, Radhakrishnan RS, Herndon DN (December 2012). "Burns: an update on current pharmacotherapy". Expert Opinion on Pharmacotherapy. 13 (17): 2485–94. doi:10.1517/14656566.2012.738195. PMC 3576016. PMID 23121414.
- Hannon R (2010). Porth pathophysiology : concepts of altered health states (1st Canadian ed.). Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 1516. ISBN 978-1-60547-781-7. Archived from the original on 1 May 2016.
- Mahadevan SV, Garmel GM, eds. (2012). An introduction to clinical emergency medicine (2nd ed.). Cambridge: Cambridge University Press. pp. 216–219. ISBN 978-0-521-74776-9. Archived from the original on 20 May 2016.
- Barayan D, Vinaik R, Auger C, Knuth CM, Abdullahi A, Jeschke MG. Inhibition of Lipolysis With Acipimox Attenuates Postburn White Adipose Tissue Browning and Hepatic Fat Infiltration. Shock. 2020;53(2):137-145. doi:10.1097/SHK.0000000000001439, 10.1097/SHK.0000000000001439
- Jeschke MG, Gauglitz GG, Kulp GA, Finnerty CC, Williams FN, Kraft R,Suman OE, Mlcak RP, Herndon DN: Long-term persistence of the pathophysi-ologic response to severe burn injury.PLoS One6:E21245, 2011.
- Gupta, Kapil; Mehrotra, Mayank; Kumar, Parul; Gogia, Anoop Raj; Prasad, Arun; Fisher, Joseph Arnold (March 2018). "Smoke Inhalation Injury: Etiopathogenesis, Diagnosis, and Management". Indian Journal of Critical Care Medicine. 22 (3): 180–188. doi:10.4103/ijccm.IJCCM_460_17. ISSN 0972-5229. PMC 5879861. PMID 29657376.
- Jeschke M (2012). Handbook of Burns Volume 1: Acute Burn Care. Springer. p. 46. ISBN 978-3-7091-0348-7. Archived from the original on 17 May 2016.
- Klingensmith M, ed. (2007). The Washington manual of surgery (5th ed.). Philadelphia, Pa.: Lippincott Williams & Wilkins. p. 422. ISBN 978-0-7817-7447-5. Archived from the original on 20 May 2016.
- Rousseau AF, Losser MR, Ichai C, Berger MM (August 2013). "ESPEN endorsed recommendations: nutritional therapy in major burns". Clinical Nutrition. 32 (4): 497–502. doi:10.1016/j.clnu.2013.02.012. PMID 23582468.
- Cianci P, Slade JB, Sato RM, Faulkner J (January–February 2013). "Adjunctive hyperbaric oxygen therapy in the treatment of thermal burns". Undersea & Hyperbaric Medicine. 40 (1): 89–108. PMID 23397872.
- Enoch S, Roshan A, Shah M (April 2009). "Emergency and early management of burns and scalds". BMJ. 338: b1037. doi:10.1136/bmj.b1037. PMID 19357185. S2CID 40561988.
- Hettiaratchy S, Papini R (July 2004). "Initial management of a major burn: II--assessment and resuscitation". BMJ. 329 (7457): 101–3. doi:10.1136/bmj.329.7457.101. PMC 449823. PMID 15242917.
- Jeschke M (2012). Handbook of Burns Volume 1: Acute Burn Care. Springer. p. 77. ISBN 978-3-7091-0348-7. Archived from the original on 19 May 2016.
- Endorf FW, Ahrenholz D (December 2011). "Burn management". Current Opinion in Critical Care. 17 (6): 601–5. doi:10.1097/MCC.0b013e32834c563f. PMID 21986459. S2CID 5525939.
- Lewis SR, Pritchard MW, Evans DJ, Butler AR, Alderson P, Smith AF, Roberts I (August 2018). "Colloids versus crystalloids for fluid resuscitation in critically ill people". The Cochrane Database of Systematic Reviews. 8 (8): CD000567. doi:10.1002/14651858.CD000567.pub7. PMC 6513027. PMID 30073665.
- Eljaiek R, Heylbroeck C, Dubois MJ (February 2017). "Albumin administration for fluid resuscitation in burn patients: A systematic review and meta-analysis". Burns. 43 (1): 17–24. doi:10.1016/j.burns.2016.08.001. PMID 27613476.
- Curinga G, Jain A, Feldman M, Prosciak M, Phillips B, Milner S (August 2011). "Red blood cell transfusion following burn". Burns. 37 (5): 742–52. doi:10.1016/j.burns.2011.01.016. PMID 21367529.
- Wasiak J, Cleland H, Campbell F, Spinks A (March 2013). "Dressings for superficial and partial thickness burns". The Cochrane Database of Systematic Reviews. 3 (3): CD002106. doi:10.1002/14651858.CD002106.pub4. hdl:10072/58266. PMC 7065523. PMID 23543513.
- Avni T, Levcovich A, Ad-El DD, Leibovici L, Paul M (February 2010). "Prophylactic antibiotics for burns patients: systematic review and meta-analysis". BMJ. 340: c241. doi:10.1136/bmj.c241. PMC 2822136. PMID 20156911.
- Hoogewerf CJ, Hop MJ, Nieuwenhuis MK, Oen IM, Middelkoop E, Van Baar ME (July 2020). "Topical treatment for facial burns". The Cochrane Database of Systematic Reviews. 2020 (7): CD008058. doi:10.1002/14651858.cd008058.pub3. PMC 7390507. PMID 32725896.
- Barajas-Nava LA, López-Alcalde J, Roqué i Figuls M, Solà I, Bonfill Cosp X (June 2013). "Antibiotic prophylaxis for preventing burn wound infection". The Cochrane Database of Systematic Reviews (6): CD008738. doi:10.1002/14651858.CD008738.pub2. PMID 23740764.
- Storm-Versloot MN, Vos CG, Ubbink DT, Vermeulen H (March 2010). Storm-Versloot MN (ed.). "Topical silver for preventing wound infection". The Cochrane Database of Systematic Reviews (3): CD006478. doi:10.1002/14651858.CD006478.pub2. PMID 20238345.
- Dumville JC, Munson C, Christie J (December 2014). "Negative pressure wound therapy for partial-thickness burns". The Cochrane Database of Systematic Reviews. 12 (12): CD006215. doi:10.1002/14651858.CD006215.pub4. PMC 7389115. PMID 25500895.
- Chaganti P, Gordon I, Chao JH, Zehtabchi S (June 2019). "A systematic review of foam dressings for partial thickness burns". The American Journal of Emergency Medicine. 37 (6): 1184–1190. doi:10.1016/j.ajem.2019.04.014. PMID 31000315. S2CID 121615225.
- Zachariah JR, Rao AL, Prabha R, Gupta AK, Paul MK, Lamba S (August 2012). "Post burn pruritus--a review of current treatment options". Burns. 38 (5): 621–9. doi:10.1016/j.burns.2011.12.003. PMID 22244605.
- Herndon D, ed. (2012). "Chapter 64: Management of pain and other discomforts in burned patients". Total burn care (4th ed.). Edinburgh: Saunders. p. 726. ISBN 978-1-4377-2786-9.
- Wasiak J, Mahar PD, McGuinness SK, Spinks A, Danilla S, Cleland H, Tan HB (October 2014). "Intravenous lidocaine for the treatment of background or procedural burn pain". The Cochrane Database of Systematic Reviews. 10 (10): CD005622. doi:10.1002/14651858.CD005622.pub4. PMC 6508369. PMID 25321859.
- Herndon D, ed. (2012). "Chapter 31: Etiology and prevention of multisystem organ failure". Total burn care (4th ed.). Edinburgh: Saunders. p. 664. ISBN 978-1-4377-2786-9.
- Breederveld RS, Tuinebreijer WE (September 2014). "Recombinant human growth hormone for treating burns and donor sites". The Cochrane Database of Systematic Reviews. 9 (9): CD008990. doi:10.1002/14651858.CD008990.pub3. PMC 7119450. PMID 25222766.
- Snell JA, Loh NH, Mahambrey T, Shokrollahi K (October 2013). "Clinical review: the critical care management of the burn patient". Critical Care. 17 (5): 241. doi:10.1186/cc12706. PMC 4057496. PMID 24093225.
- "FDA Approves StrataGraft for the Treatment of Adults with Thermal Burns". U.S. Food and Drug Administration (FDA) (Press release). 15 June 2021. Retrieved 20 April 2023.
- Jeschke M (2012). Handbook of Burns Volume 1: Acute Burn Care. Springer. p. 266. ISBN 978-3-7091-0348-7. Archived from the original on 10 May 2016.
- Orgill DP, Piccolo N (September–October 2009). "Escharotomy and decompressive therapies in burns". Journal of Burn Care & Research. 30 (5): 759–68. doi:10.1097/BCR.0b013e3181b47cd3. PMID 19692906.
- "General data about burns". Burn Centre Care.
- Barqouni L, Abu Shaaban N, Elessi K, et al. (Cochrane Wounds Group) (June 2014). "Interventions for treating phosphorus burns". The Cochrane Database of Systematic Reviews. 2014 (6): CD008805. doi:10.1002/14651858.CD008805.pub3. PMC 7173745. PMID 24896368.
- Wijesinghe M, Weatherall M, Perrin K, Beasley R (May 2009). "Honey in the treatment of burns: a systematic review and meta-analysis of its efficacy". The New Zealand Medical Journal. 122 (1295): 47–60. PMID 19648986.
- Norman G, Christie J, Liu Z, Westby MJ, Jefferies JM, Hudson T, et al. (July 2017). "Antiseptics for burns". The Cochrane Database of Systematic Reviews. 7 (7): CD011821. doi:10.1002/14651858.cd011821.pub2. PMC 6483239. PMID 28700086.
- Jull AB, Cullum N, Dumville JC, Westby MJ, Deshpande S, Walker N (March 2015). "Honey as a topical treatment for wounds". The Cochrane Database of Systematic Reviews. 3 (3): CD005083. doi:10.1002/14651858.CD005083.pub4. PMC 9719456. PMID 25742878.
- Dat AD, Poon F, Pham KB, Doust J (February 2012). "Aloe vera for treating acute and chronic wounds". The Cochrane Database of Systematic Reviews. 2012 (2): CD008762. doi:10.1002/14651858.CD008762.pub2. PMC 9943919. PMID 22336851.
- Maenthaisong R, Chaiyakunapruk N, Niruntraporn S, Kongkaew C (September 2007). "The efficacy of aloe vera used for burn wound healing: a systematic review". Burns. 33 (6): 713–8. doi:10.1016/j.burns.2006.10.384. PMID 17499928.
- Bahramsoltani R, Farzaei MH, Rahimi R (September 2014). "Medicinal plants and their natural components as future drugs for the treatment of burn wounds: an integrative review". Archives of Dermatological Research. 306 (7): 601–17. doi:10.1007/s00403-014-1474-6. PMID 24895176. S2CID 23859340.
- Juckett G, Hartman-Adams H (August 2009). "Management of keloids and hypertrophic scars". American Family Physician. 80 (3): 253–60. PMID 19621835.
- Turkington C, Dover JS, Cox B (2007). The encyclopedia of skin and skin disorders (3rd ed.). New York, NY: Facts on File. p. 64. ISBN 978-0-8160-7509-6. Archived from the original on 18 May 2016.
- "Medically Sound: Treating and Caring for Burn, Electricity, and Radiation Victims". Medically Sound. 26 September 2020. Retrieved 1 November 2020.
- National Burn Repository, Pg. 10
- King C, Henretig FM, King BR, Loiselle J, Ruddy RM, Wiley II JF, eds. (2008). Textbook of pediatric emergency procedures (2nd ed.). Philadelphia: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 1077. ISBN 978-0-7817-5386-9. Archived from the original on 22 May 2016.
- Roberts MC (2009). Handbook of pediatric psychology (4th ed.). New York: Guilford. p. 421. ISBN 978-1-60918-175-8. Archived from the original on 30 April 2016.
- "ACI Statewide Burn Injury Service. Physiotherapy and Occupational Therapy Clinical Practice Guidelines" (PDF). 5 March 2018.
- Monstrey, Stan; Middelkoop, Esther; Vranckx, Jan Jeroen; Bassetto, Franco; Ziegler, Ulrich E.; Meaume, Sylvie; Téot, Luc (August 2014). "Updated Scar Management Practical Guidelines: Non-invasive and invasive measures". Journal of Plastic, Reconstructive & Aesthetic Surgery. 67 (8): 1017–1025. doi:10.1016/j.bjps.2014.04.011. PMID 24888226.
- Meaume, Sylvie; Le Pillouer-Prost, Anne; Richert, Bertrand; Roseeuw, Diane; Vadoud, Javid (July 2014). "Management of scars: updated practical guidelines and use of silicones". European Journal of Dermatology. 24 (4): 435–443. doi:10.1684/ejd.2014.2356. ISSN 1167-1122. PMID 25141160. S2CID 25937084.
- "WHO Disease and injury country estimates". World Health Organization. 2009. Archived from the original on 11 November 2009. Retrieved 11 November 2009.
- GBD 2013 Mortality Causes of Death Collaborators (January 2015). "Global, regional, and national age-sex specific all-cause and cause-specific mortality for 240 causes of death, 1990–2013: a systematic analysis for the Global Burden of Disease Study 2013". Lancet. 385 (9963): 117–71. doi:10.1016/s0140-6736(14)61682-2. PMC 4340604. PMID 25530442.
{{cite journal}}:|author=has generic name (help) - Lozano R, Naghavi M, Foreman K, Lim S, Shibuya K, Aboyans V, et al. (December 2012). "Global and regional mortality from 235 causes of death for 20 age groups in 1990 and 2010: a systematic analysis for the Global Burden of Disease Study 2010". Lancet. 380 (9859): 2095–128. doi:10.1016/S0140-6736(12)61728-0. hdl:10536/DRO/DU:30050819. PMID 23245604. S2CID 1541253.
- Edlich RF, Farinholt HM, Winters KL, Britt LD, Long WB (2005). "Modern concepts of treatment and prevention of electrical burns". Journal of Long-Term Effects of Medical Implants. 15 (5): 511–32. doi:10.1615/jlongtermeffmedimplants.v15.i5.50. PMID 16218900.
- Ahuja RB, Bhattacharya S (August 2004). "Burns in the developing world and burn disasters". BMJ. 329 (7463): 447–9. doi:10.1136/bmj.329.7463.447. PMC 514214. PMID 15321905.
- Gupta (2003). Textbook of Surgery. Jaypee Brothers Publishers. p. 42. ISBN 978-81-7179-965-7. Archived from the original on 27 April 2016.
- Pećanac M, Janjić Z, Komarcević A, Pajić M, Dobanovacki D, Misković SS (2013). "Burns treatment in ancient times". Medicinski Pregled. 66 (5–6): 263–7. doi:10.1016/s0264-410x(02)00603-5. PMID 23888738.
- Song D (5 September 2012). Plastic surgery (3rd ed.). Edinburgh: Saunders. p. 393.e1. ISBN 978-1-4557-1055-3. Archived from the original on 2 May 2016.
- Wylock P (2010). The life and times of Guillaume Dupuytren, 1777–1835. Brussels: Brussels University Press. p. 60. ISBN 978-90-5487-572-7. Archived from the original on 16 May 2016.
General and cited references
- National Burn Repository 2012 Report (PDF). Dataset Version 8.0. Chicago: American Burn Association. 2012. Archived from the original (PDF) on 3 March 2016. Retrieved 20 April 2013.
External links
- Parkland Formula
- "Burns". MedlinePlus. U.S. National Library of Medicine.
