Aberrant subclavian artery
Aberrant subclavian artery, or aberrant subclavian artery syndrome, is a rare anatomical variant of the origin of the right or left subclavian artery. This abnormality is the most common congenital vascular anomaly of the aortic arch,[1] occurring in approximately 1% of individuals.[1][2][3]
| Aberrant subclavian artery | |
|---|---|
| Other names | Aberrant subclavian artery syndrome |
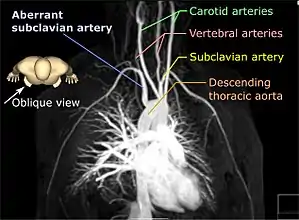 | |
| Aberrant subclavian artery on MR angiography. | |
| Specialty | Medical genetics |
Presentation
This condition is usually asymptomatic.[1] The aberrant artery usually arises just distal to the left subclavian artery and crosses in the posterior part of the mediastinum on its way to the right upper extremity.[2] In 80% of individuals it crosses behind the esophagus.[2] Such course of this aberrant vessel may cause a vascular ring around the trachea and esophagus. Dysphagia due to an aberrant right subclavian artery is termed dysphagia lusoria, although this is a rare complication.[2][3] In addition to dysphagia, aberrant right subclavian artery may cause stridor, dyspnoea, chest pain, or fever.[1] An aberrant right subclavian artery may compress the recurrent laryngeal nerve causing a palsy of that nerve, which is termed Ortner's syndrome.[4]
The aberrant right subclavian artery frequently arises from a dilated segment of the proximal descending aorta, the so-called Diverticulum of Kommerell (which was named for the German radiologist Burkhard Friedrich Kommerell (1901–1990), who discovered it in 1936).[5][6] It is alternatively known as a lusorian artery.[1][3]
Pathophysiology

In the normal embryological development of the aortic arches, the right dorsal aorta regresses caudal to the origin of the 7th intersegmental artery which gives rise to the right subclavian artery. In formation of an aberrant right subclavian artery, the regression occurs instead between the 7th intersegmental artery and the right common carotid so that the right subclavian artery is then connected to the left dorsal aorta via the part of the right dorsal aorta which normally regresses. During growth, the origin of the right subclavian artery migrates until it is just distal to that of the left subclavian.[3]
Diagnosis
Treatment
Surgery is occasionally used to treat the condition.[7]
Images
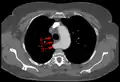 Aberrant subclavian artery at axial CT-scan. (1) trachea, (2) esophagus, (3) Aberrant subclavian artery.
Aberrant subclavian artery at axial CT-scan. (1) trachea, (2) esophagus, (3) Aberrant subclavian artery. Aberrant right subclavian artery at angiography.
Aberrant right subclavian artery at angiography. Tape-like impression of the esophagus caused by aberrant subclavian artery. Below (arrows) narrowing of the esophagus by a tumor that is causing the swallowing problems.
Tape-like impression of the esophagus caused by aberrant subclavian artery. Below (arrows) narrowing of the esophagus by a tumor that is causing the swallowing problems. Aberrant subclavian artery seen at swallowing study: Impression of the esophagus from behind.
Aberrant subclavian artery seen at swallowing study: Impression of the esophagus from behind.
See also
References
- Mahmodlou, Rahim; Sepehrvand, Nariman; Hatami, Sanaz (2014). "Aberrant Right Subclavian Artery: A Life-threatening Anomaly that should be considered during Esophagectomy". Journal of Surgical Technique and Case Report. 6 (2): 61–63. doi:10.4103/2006-8808.147262. PMC 4290042. PMID 25598945.
- Kau, Thomas; Sinzig, Marietta; Gasser, Johann; Lesnik, Gerald; Rabitsch, Egon; Celedin, Stefan; Eicher, Wolfgang; Illiasch, Herbert; Hausegger, Klaus Armin (2007). "Aortic Development and Anomalies". Seminars in Interventional Radiology. 24 (2): 141–152. doi:10.1055/s-2007-980040. PMC 3036416. PMID 21326792.
- Chaoui, R; Rake, A; Heling, KS (2008). "Aortic arch with four vessels: aberrant right subclavian artery". Ultrasound in Obstetrics and Gynecology. 31 (1): 115–117. doi:10.1002/uog.5240. PMID 18098341.
- Bickle, IC; Kelly, BE; Brooker, DS (2002). "Ortner's syndrome: a radiological diagnosis". The Ulster Medical Journal. 71 (1): 55–56. PMC 2475354. PMID 12137166.
- St-Amant, Maxime. "Kommerell diverticulum (right aberrant subclavian artery)". Radiopaedia. Retrieved 17 November 2017.
- Jha, Praveen. "Kommerell diverticulum". Radiopaedia. Retrieved 17 November 2017.
- Kouchoukos NT, Masetti P (April 2007). "Aberrant subclavian artery and Kommerell aneurysm: surgical treatment with a standard approach". The Journal of Thoracic and Cardiovascular Surgery. 133 (4): 888–92. doi:10.1016/j.jtcvs.2006.12.005. PMID 17382621.