Accessory spleen
An accessory spleen is a small nodule of splenic tissue found apart from the main body of the spleen. Accessory spleens are found in approximately 10 percent of the population[1] and are typically around 1 centimetre in diameter. They may resemble a lymph node or a small spleen. They form either by the result of developmental anomalies or trauma.[2] They are medically significant in that they may result in interpretation errors in diagnostic imaging[2] or continued symptoms after therapeutic splenectomy.[1] Polysplenia is the presence of multiple accessory spleens rather than one normal spleen.
| Accessory spleen | |
|---|---|
| Other names | Supernumerary spleen, splenule, splenunculus |
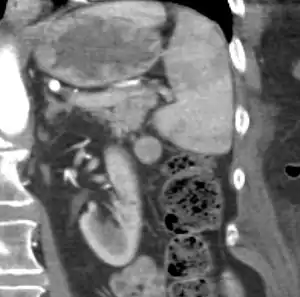 | |
| CT scan of an accessory spleen (in center of image) between the spleen and left kidney. | |
| Specialty | Medical genetics |
Causes and locations
| Accessory spleen | |
|---|---|
| Details | |
| Identifiers | |
| Latin | splen accessorius, lien accessorius |
| TA98 | A13.2.01.022 |
| TA2 | 5177 |
| FMA | 16028 |
| Anatomical terminology | |
Accessory spleens may be formed during embryonic development when some of the cells from the developing spleen are deposited along the path from the midline, where the spleen forms, over to its final location on the left side of the abdomen by the 9th–11th ribs. The most common locations for accessory spleens are the hilum of the spleen and adjacent to the tail of the pancreas. They may be found anywhere along the splenic vessels, in the gastrosplenic ligament, the splenorenal ligament, the walls of the stomach or intestines,[3][4] the pancreatic tail,[5][6] the greater omentum,[7][8] the mesentery,[9] the renal fossa,[10][11] or the gonads and their path of descent.[12] The typical size is approximately 1 centimeter, but sizes ranging from a few millimeters up to 2–3 centimeters are not uncommon.[2]
Splenogonadal fusion can result in one or more accessory spleens along a path from the abdomen into the pelvis or scrotum. The developing spleen forms near the urogenital ridge from which the gonads develop. The gonads may pick up some tissue from the spleen, and as they descend through the abdomen during development, they can produce either a continuous or a broken line of deposited splenic tissue.[12]
Splenosis is a condition where foci of splenic tissue undergo autotransplantation, most often following physical trauma or splenectomy. Displaced tissue fragments can implant on well vascularized surfaces in the abdominal cavity, or, if the diaphragmatic barrier is broken, the thorax.[13][14]
_photomicrograph.JPG.webp) Histologic section of an accessory spleen
Histologic section of an accessory spleen Ultrasonography of an accessory spleen.
Ultrasonography of an accessory spleen.
Significance

If splenectomy is performed for conditions in which blood cells are sequestered in the spleen, failure to remove accessory spleens may result in the failure of the condition to resolve.[1] During medical imaging, accessory spleens may be confused for enlarged lymph nodes or neoplastic growth in the tail of the pancreas,[5] gastrointestinal tract, adrenal glands or gonads.[2]
References
- Moore, Keith L. (1992). Clinically Oriented Anatomy (3rd ed.). Baltimore: Williams & Wilkins. p. 187. ISBN 978-0-683-06133-8.
- Gayer G; Zissin R; Apter S; Atar E; Portnoy O; Itzchak Y (August 2001). "CT findings in congenital anomalies of the spleen". British Journal of Radiology. 74 (884): 767–772. doi:10.1259/bjr.74.884.740767. PMID 11511506.
- Wang G, Chen P, Zong L (February 2014). "Accessory spleen arising from the gastric fundus mimicking gastrointestinal stromal tumor following splenectomy: A case report". Exp Ther Med. 7 (2): 349–351. doi:10.3892/etm.2013.1415. PMC 3881060. PMID 24396402.
- Almazeedi S, Alhaddad E, Al-Khithr T, Alhunaidi M (2017). "Incidental gastric accessory spleen during laparoscopic sleeve gastrectomy". Int J Surg Case Rep. 36: 119–121. doi:10.1016/j.ijscr.2017.05.022. PMC 5447567. PMID 28558346.
- Kim SH; Lee JM; Han JK; Lee JY; Kim KW; Cho KC; Choi BI (March–April 2008). "Intrapancreatic Accessory Spleen: Findings on MR Imaging, CT, US and Scintigraphy, and the Pathologic Analysis". Korean J Radiol. 9 (2): 162–174. doi:10.3348/kjr.2008.9.2.162. PMC 2627219. PMID 18385564.
- Bostancı EB, Oter V, Okten S, Küçük NO, Soydal C, Turhan N, Akoglu M (November 2016). "Intra-pancreatic Accessory Spleen Mimicking Pancreatic Neuroendocrine Tumor on 68-Ga-Dotatate PET/CT". Arch Iran Med. 19 (11): 816–819. PMID 27845553.
- Zhang C, Zhang XF (September 2011). "Accessory spleen in the greater omentum". Am. J. Surg. 202 (3): e28–30. doi:10.1016/j.amjsurg.2010.06.032. PMID 21784408.
- Gill N, Nasir A, Douglin J, Pretterklieber B, Steinke H, Pretterklieber M, Cotofana S (2017). "Accessory Spleen in the Greater Omentum: Embryology and Revisited Prevalence Rates". Cells Tissues Organs (Print). 203 (6): 374–378. doi:10.1159/000458754. PMID 28420007.
- Ruiz-Tovar J, Ripalda E, Beni R, Nistal J, Monroy C, Carda P (2009). "Hypersplenism caused by an accessory spleen mimicking an intra-abdominal neoplasm: report of a case". Surg. Today. 39 (9): 818–20. doi:10.1007/s00595-008-3919-z. PMID 19779782.
- Servadio Y, Leibovitch I, Apter S, Mor Y, Goldwasser B (1994). "Symptomatic heterotopic splenic tissue in the left renal fossa". Eur. Urol. 25 (2): 174–6. doi:10.1159/000475275. PMID 8137861.
- Azar GB, Awwad JT, Mufarrij IK (October 1993). "Accessory spleen presenting as adnexal mass". Acta Obstet Gynecol Scand. 72 (7): 587–8. doi:10.3109/00016349309058171. PMID 8213112.
- Chen S–L; Kao Y–L; Sun H–S; Lin W–L (November 2008). "Splenogonadal Fusion". Journal of the Formosan Medical Association. 107 (11): 892–5. doi:10.1016/S0929-6646(08)60206-5. ISSN 0929-6646. PMID 18971159. Archived from the original on 2009-06-09. Retrieved 2009-03-03.
- Abu Hilal M; Harb A; Zeidan B; Steadman B; Primrose JN; Pearce NW (January 5, 2009). "Hepatic splenosis mimicking HCC in a patient with hepatitis C liver cirrhosis and mildly raised alpha feto protein; the important role of explorative laparoscopy". World Journal of Surgical Oncology. 7 (1): 1. doi:10.1186/1477-7819-7-1. PMC 2630926. PMID 19123935.
- Madjar S; Weissberg D (October 1994). "Thoracic splenosis". Thorax. 49 (10): 1020–1022. doi:10.1136/thx.49.10.1020. ISSN 0040-6376. PMC 475241. PMID 7974296.
- W. Richard Webb; Wiliam E. Brant; Nancy M. Major (2014). Fundamentals of Body CT, Fundamentals of Radiology (4 ed.). Elsevier Health Sciences. p. 242. ISBN 9780323263580.
- Note: The case is possibly splenosis rather than an accessory spleen:
Maki, Takehiro; Omi, Makoto; Ishii, Daisuke; Kaneko, Hiroyuki; Misu, Kenjiro; Inomata, Hitoshi; Tateno, Masatoshi; Nihei, Kazuyoshi (2015). "Spontaneous hemorrhage from splenic tissue 13 years after total splenectomy: report of a case". Surgical Case Reports. 1 (1): 91. doi:10.1186/s40792-015-0099-0. ISSN 2198-7793. PMC 4593983. PMID 26943415.