Auditory neuropathy
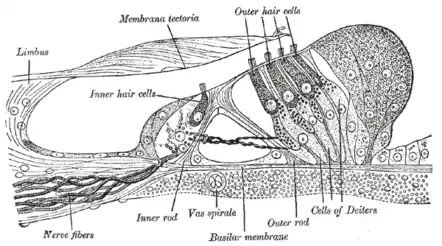
Auditory neuropathy (AN) is a hearing disorder in which the outer hair cells of the cochlea are present and functional, but sound information is not transmitted sufficiently by the auditory nerve to the brain. Hearing loss with AN can range from normal hearing sensitivity to profound hearing loss.
A neuropathy usually refers to a disease of the peripheral nerve or nerves, but the auditory nerve itself is not always affected in auditory neuropathy spectrum disorders.[1] Prevalence in the population is relatively unknown. Neonates with high risk factors for hearing loss have a prevalence of up to 40% (Vignesh, Jaya, & Muraleedharan 2016). These high-risk factors are: hypoxia, low birth weight, premature birth, hyperbilirubinemia, jaundice, and aminoglycoside antibiotic treatments (NIDCD, 2018).
Possible sites of lesion
| Hair cell | |
|---|---|
 Three rows of Outer Hair Cells in the Organ of Corti, one row of Inner Hair Cells. | |
| Identifiers | |
| MeSH | C538268 |
| Anatomical terms of neuroanatomy | |
Based on clinical testing of subjects with auditory neuropathy, the disruption in the stream of sound information has been localized to one or more of three probable locations: the inner hair cells of the cochlea, the synapse between the inner hair cells and the auditory nerve, or a lesion of the ascending auditory nerve itself.[2]
Diagnosing auditory neuropathy
Diagnosis is possible after a test battery, that must necessarily include the following: the auditory brainstem response and otoacoustic emissions. Auditory brainstem response should be tested with both polarities (helps in identifying cochlear microphonics).[3]
Auditory Neuropathy can be diagnosed with a battery of tests including Otoacoustic Emissions (OAE), Auditory Brainstem Response (ABR), and acoustic reflexes. The classic AN paradigm would include present OAEs indicating normal outer hair cell function, absent or abnormal ABR with presence of the cochlear microphonic, and absent acoustic reflexes. Other tests would include pure-tone and speech audiometry. AN patients can have a range of hearing thresholds with difficulty in speech perception. Patients with auditory neuropathy spectrum disorders have to date never been shown to have normal middle ear muscle reflexes at 95 dB HL or less despite having normal otoacoustic emissions.[4]
Auditory neuropathy can occur spontaneously, or in combination with diseases like Charcot-Marie-Tooth disease and Friedreich's ataxia. AN can have either congenital or acquired causes. AN can be due to genetic factors in syndromic, non-syndromic, and mitochondrial related patterns. Approximately 40% of AN cases are estimated to have a genetic cause.[5]
It appears that regardless of the audiometric pattern (hearing thresholds) or of their function on traditional speech testing in quiet the vast majority of those affected have very poor hearing in background noise situations.[6]
Residual auditory function
When testing the auditory system, there really is no characteristic presentation on the audiogram.
When diagnosing someone with auditory neuropathy, there is no characteristic level of functioning either. People can present relatively little dysfunction other than problems of hearing speech in noise, or can present as completely deaf and gaining no useful information from auditory signals.
Hearing aids are sometimes prescribed, with mixed success.[7]
FM systems in combination with hearing aids or cochlear implants could increase success of these amplification devices.
Some people with auditory neuropathy obtain cochlear implants, also with mixed success.[7][8]
Screening
Universal Newborn Hearing Screenings are mandated in a majority of the United States. In most parts of Australia, hearing screening via AABR testing is mandated, meaning that essentially all congenital (i.e., not those related to later onset degenerative disorders) auditory neuropathy cases should be diagnosed at birth.
Auditory neuropathy is sometimes difficult to catch right away, even with these precautions in place. Parental suspicion of a hearing loss is a trustworthy screening tool for hearing loss, too; if it is suspected, that is sufficient reason to seek a hearing evaluation from an audiologist.[9]
See also
References
- Amatuzzi, Monica; Liberman, M. Charles; Northrop, Clarinda (14 June 2011). "Selective Inner Hair Cell Loss in Prematurity: A Temporal Bone Study of Infants from a Neonatal Intensive Care Unit". Journal of the Association for Research in Otolaryngology. 12 (5): 595–604. doi:10.1007/s10162-011-0273-4. PMC 3173554. PMID 21674215.
- Starr, Arnold; Picton, Terence W.; Sininger, Yvonnc; Hood, Linda J.; Berlin, Charles I. (1996). "Auditory neuropathy". Brain. 119 (3): 741–753. doi:10.1093/brain/119.3.741. PMID 8673487.
- Roush, P. (2008). "Auditory Neuropathy Spectrum Disorder, Evaluation and Management". The Hearing Journal. 61 (11): 36–41. doi:10.1097/01.HJ.0000342437.78354.f7. S2CID 147587370.
- Berlin, Charles I.; Hood, Linda J.; Morlet, Thierry; Wilensky, Diane; John, Patti St.; Montgomery, Elizabeth; Thibodaux, Melanie (1 September 2005). "Absent or Elevated Middle Ear Muscle Reflexes in the Presence of Normal Otoacoustic Emissions: A Universal Finding in 136 Cases of Auditory Neuropathy/Dys-synchrony". Journal of the American Academy of Audiology. 16 (8): 546–553. doi:10.3766/jaaa.16.8.3. PMID 16295241.
- Manchaiah, Vinaya K.C.; Zhao, Fei; Danesh, Ali A.; Duprey, Rachel (February 2011). "The genetic basis of auditory neuropathy spectrum disorder (ANSD)". International Journal of Pediatric Otorhinolaryngology. 75 (2): 151–158. doi:10.1016/j.ijporl.2010.11.023. PMID 21176974.
- Zeng, Fan-Gang; Liu, Sheng (April 2006). "Speech Perception in Individuals With Auditory Neuropathy". Journal of Speech, Language, and Hearing Research. 49 (2): 367–380. doi:10.1044/1092-4388(2006/029). PMID 16671850. S2CID 8531043.
- Roush, Patricia; Frymark, Tobi; Venediktov, Rebecca; Wang, Beverly (December 2011). "Audiologic Management of Auditory Neuropathy Spectrum Disorder in Children: A Systematic Review of the Literature". American Journal of Audiology. 20 (2): 159–170. doi:10.1044/1059-0889(2011/10-0032). PMID 21940978. S2CID 12773097.
- Carvalho, Ana Claudia Martinho de; Bevilacqua, Maria Cecilia; Sameshima, Koichi; Costa Filho, Orozimbo Alves (August 2011). "Auditory neuropathy/auditory dyssynchrony in children with cochlear implants". Brazilian Journal of Otorhinolaryngology. 77 (4): 481–487. doi:10.1590/s1808-86942011000400012. PMID 21860975.
- Cohen, Elizabeth. "Don't let a doctor destroy your baby's hearing". CNN. Archived from the original on 12 March 2011.
Further reading
- Vlastarakos, Petros V.; Nikolopoulos, Thomas P.; Tavoulari, Evangelia; Papacharalambous, George; Korres, Stavros (August 2008). "Auditory neuropathy: Endocochlear lesion or temporal processing impairment? Implications for diagnosis and management". International Journal of Pediatric Otorhinolaryngology. 72 (8): 1135–1150. doi:10.1016/j.ijporl.2008.04.004. PMID 18502518.
- Vignesh, S. S.; Jaya, V.; Muraleedharan, A. (12 August 2014). "Prevalence and Audiological Characteristics of Auditory Neuropathy Spectrum Disorder in Pediatric Population: A Retrospective Study". Indian Journal of Otolaryngology and Head & Neck Surgery. 68 (2): 196–201. doi:10.1007/s12070-014-0759-6. PMC 4899353. PMID 27340636.
External links
- Auditory neuropathy: What is it and what can we do about it? from the LSU Medical School
- Auditory Neuropathy Information site
- Auditory Neuropathy by Timothy C. Hain
- https://www.nidcd.nih.gov/health/auditory-neuropathy
- https://www.audiology.org/tags/auditory-neuropathy-spectrum-disorder-ansd
- http://www.asha.org/auditory-neuropathy
- Auditory Neuropathy. (2018, March 16). Retrieved from https://www.nidcd.nih.gov/health/auditory- neuropathy
- Interacoustics. (2016). Cochlear Microphonics CM. Retrieved from https://www.interacoustics.com/guides/test/abr-tests/cochlear-microphonics-cm