Cerebrovascular disease
Cerebrovascular disease includes a variety of medical conditions that affect the blood vessels of the brain and the cerebral circulation. Arteries supplying oxygen and nutrients to the brain are often damaged or deformed in these disorders.[2] The most common presentation of cerebrovascular disease is an ischemic stroke or mini-stroke and sometimes a hemorrhagic stroke.[2] Hypertension (high blood pressure) is the most important contributing risk factor for stroke and cerebrovascular diseases as it can change the structure of blood vessels and result in atherosclerosis.[5] Atherosclerosis narrows blood vessels in the brain, resulting in decreased cerebral perfusion. Other risk factors that contribute to stroke include smoking and diabetes.[6] Narrowed cerebral arteries can lead to ischemic stroke, but continually elevated blood pressure can also cause tearing of vessels, leading to a hemorrhagic stroke.[4]
| Cerebrovascular disease | |
|---|---|
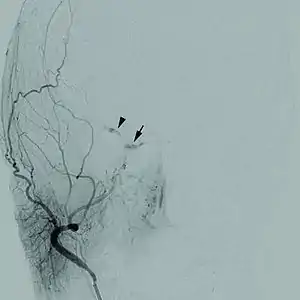 | |
| Cerebral angiogram of a carotid-cavernous fistula | |
| Specialty | Neurology |
| Symptoms | Weakness on one side of body[1] |
| Types | Stroke, vascular dementia, TIA, subarachnoid haemorrhage[2] |
| Diagnostic method | Neurological exam, physical exam[3] |
| Treatment | Blood thinners, anti-hypertensives[4] |
A stroke usually presents with an abrupt onset of a neurologic deficit – such as hemiplegia (one-sided weakness), numbness, aphasia (language impairment), or ataxia (loss of coordination) – attributable to a focal vascular lesion.[7] The neurologic symptoms manifest within seconds because neurons need a continual supply of nutrients, including glucose and oxygen, that are provided by the blood. Therefore, if blood supply to the brain is impeded, injury and energy failure is rapid.[8]
Besides hypertension, there are also many less common causes of cerebrovascular disease, including those that are congenital or idiopathic and include CADASIL, aneurysms, amyloid angiopathy, arteriovenous malformations, fistulas, and arterial dissections.[9] Many of these diseases can be asymptomatic until an acute event, such as a stroke, occurs.[9] Cerebrovascular diseases can also present less commonly with headache or seizures.[10] Any of these diseases can result in vascular dementia due to ischemic damage to the brain.[11][12]
Signs and symptoms

The most common presentation of cerebrovascular diseases is an acute stroke, which occurs when blood supply to the brain is compromised.[13] Symptoms of stroke are usually rapid in onset, and may include weakness of one side of the face or body, numbness on one side of the face or body, inability to produce or understand speech, vision changes, and balance difficulties.[1] Hemorrhagic strokes can present with a very severe, sudden headache associated with vomiting, neck stiffness, and decreased consciousness.[13] Symptoms vary depending on the location and the size of the area of involvement of the stroke. Edema, or swelling, of the brain may occur which increases intracranial pressure and may result in brain herniation. A stroke may result in coma or death if it involves key areas of the brain.[14]
Other symptoms of cerebrovascular disease include migraines, seizures, epilepsy, or cognitive decline. However, cerebrovascular disease may go undetected for years until an acute stroke occurs. In addition, patients with some rare congenital cerebrovascular diseases may begin to have these symptoms in childhood.[15]
Causes
Congenital
Congenital diseases are medical conditions that are present at birth that may be associated with or inherited through genes.[16] Examples of congenital cerebrovascular diseases include arteriovenous malformations, germinal matrix hemorrhage, and CADASIL (cerebral autosomal-dominant arteriopathy with subcortical infarcts and leukoencephalopathy).[9] Arteriovenous malformations are abnormal tangles of blood vessels. Usually, a capillary bed separates arteries from veins, which protects the veins from the higher blood pressures that occur in arteries. In arteriovenous malformations, arteries are directly connected to veins, which increases the risk of venous rupture and hemorrhage. Arteriovenous malformations in the brain have a 2–4% chance of rupture each year. However, many arteriovenous malformations go unnoticed and are asymptomatic throughout a person's lifetime.[17]

A germinal matrix hemorrhage is bleeding into the brain of premature infants caused by the rupture of fragile blood vessels within the germinal matrix of premature babies.[18] The germinal matrix is a highly vascularized area within an unborn infant's brain from which brain cells, including neurons and glial cells, originate. Infants are at most risk to germinal matrix hemorrhages when they are born prematurely, before 32 weeks.[18] The stresses exposed after birth, along with the fragile blood vessels, increase risk of hemorrhage. Signs and symptoms include flaccid weakness, seizures, abnormal posturing, or irregular respiration.[18]
CADASIL is an inherited disorder caused by mutations in the Notch 3 gene located on chromosome 19.[19] The Notch 3 gene codes for a transmembrane protein whose function is not well-known. However, the mutation causes accumulation of this protein within small to medium-sized blood vessels.[19] This disease often presents in early adulthood with migraines, stroke, mood disturbances, and cognitive deterioration. MRI shows white matter changes in the brain and also signs of repeated strokes. The diagnosis can be confirmed by gene testing.[20]
Acquired
Acquired cerebrovascular diseases are those that are obtained throughout a person's life that may be preventable by controlling risk factors. The incidence of cerebrovascular disease increases as an individual ages.[21] Causes of acquired cerebrovascular disease include atherosclerosis, embolism, aneurysms, and arterial dissections.[9] Atherosclerosis leads to narrowing of blood vessels and less perfusion to the brain, and it also increases the risk of thrombosis, or a blockage of an artery, within the brain. Major modifiable risk factors for atherosclerosis include:[22]

Controlling these risk factors can reduce the incidence of atherosclerosis and stroke.[25] Atrial fibrillation is also a major risk factor for strokes. Atrial fibrillation causes blood clots to form within the heart, which may travel to the arteries within the brain and cause an embolism. The embolism prevents blood flow to the brain, which leads to a stroke.
An aneurysm is an abnormal bulging of small sections of arteries, which increases the risk of artery rupture. Intracranial aneurysms are a leading cause of subarachnoid hemorrhage, or bleeding around the brain within the subarachnoid space. There are various hereditary disorders associated with intracranial aneurysms, such as Ehlers-Danlos syndrome, autosomal dominant polycystic kidney disease, and familial hyperaldosteronism type I.[26][27][28] However, individuals without these disorders may also obtain aneurysms. The American Heart Association and American Stroke Association recommend controlling modifiable risk factors including smoking and hypertension.[29]
Arterial dissections are tears of the internal lining of arteries, often associated with trauma.[30] Dissections within the carotid arteries or vertebral arteries may compromise blood flow to the brain due to thrombosis, and dissections increase the risk of vessel rupture.[31]
Idiopathic
Idiopathic diseases are those that occur spontaneously without a known cause.[32] Moyamoya is an example of an idiopathic cerebrovascular disorder that results in narrowing and occlusion of intracranial blood vessels.[9] The most common presentation is stroke or transient ischemic attack, but cognitive decline within children may also be a presenting symptom.[9][13] The disease may begin to show symptoms beginning in adolescence, but some may not have symptoms until adulthood.[13]
Pathophysiology
Mechanism of brain cell death
When a reduction in blood flow lasting seconds occurs, the brain tissue suffers ischemia, or inadequate blood supply.[33][34] If the interruption of blood flow is not restored in minutes, the tissue suffers infarction followed by tissue death.[35] When the low cerebral blood flow persists for a longer duration, this may develop into an infarction in the border zones (areas of poor blood flow between the major cerebral artery distributions). In more severe instances, global hypoxia-ischemia causes widespread brain injury leading to a severe cognitive sequelae called hypoxic-ischemic encephalopathy.[36]
An ischemic cascade occurs where an energetic molecular problem arises due to lack of oxygen and nutrients. The cascade results in decreased production of adenosine triphosphate (ATP), which is a high-energy molecule needed for cells in the brain to function.[37] Consumption of ATP continues in spite of insufficient production, this causes total levels of ATP to decrease and lactate acidosis to become established (ionic homeostasis in neurons is lost). The downstream mechanisms of the ischemic cascade thus begins. Ion pumps no longer transport Ca2+ out of cell, this triggers release of glutamate, which in turn allows calcium into cell walls. In the end the apoptosis pathway is initiated and cell death occurs.[38]
There are several arteries that supply oxygen to different areas of the brain, and damage or occlusion of any of them can result in stroke.[39] The carotid arteries cover the majority of the cerebrum. The common carotid artery divides into the internal and the external carotid arteries. The internal carotid artery becomes the anterior cerebral artery and the middle central artery. The ACA transmits blood to the frontal parietal. From the basilar artery are two posterior cerebral arteries. Branches of the basilar and PCA supply the occipital lobe, brain stem, and the cerebellum.[40] Ischemia is the loss of blood flow to the focal region of the brain. This produces heterogeneous areas of ischemia at the affected vascular region, furthermore, blood flow is limited to a residual flow. Regions with blood flow of less than 10 mL/100 g of tissue/min are core regions (cells here die within minutes of a stroke). The ischemic penumbra with a blood flow of <25 ml/100g tissue/min, remain usable for more time (hours).[41]
Types of stroke
There are two main divisions of strokes: ischemic and hemorrhagic. Ischemic stroke involves decreased blood supply to regions of the brain, while hemorrhagic stroke is bleeding into or around the brain.[42]
Ischemic
- Ischemic stroke, the most common is caused by a blockage of a blood vessel in the brain, usually caused by thrombosis or emboli from a proximal arterial source or the heart, that leads to the brain being starved of oxygen.[43] The neurologic signs and symptoms must last longer than 24 hours or the brain infarction is demonstrated, mainly by imaging techniques.[44]
- Transient ischemic attack (TIA) also called a mini-stroke. This is a condition in which the blood flow to a region of the brain is blocked, but blood flow is quickly restored and the brain tissue can fully recover. The symptoms are only transient, leaving no sequelae, or long-term deficits.[45] In order to diagnose this entity, all neurologic signs and symptoms must have been resolved within 24 hrs without evidence of brain infarction on brain imaging.[46]
Hemorrhagic
- Subarachnoid haemorrhage occurs when blood leaks out of damaged vessels into the cerebrospinal fluid in the subarachnoid space around the brain.[2] The most common cause of a subarachnoid hemorrhage is an aneurysm rupture due to the weakened blood vessel walls and increased wall stress.[47] The neurologic symptoms are produced by the blood mass effect on neural structures, from the toxic effects of blood on the brain tissue, or by the increasing of intracranial pressure.[48]
- Intracerebral haemorrhage is bleeding directly into the brain rather than around the brain.[42] Causes and risk factors include hypertension, blood thinning medications, trauma, and arteriovenous malformations.[49]
Diagnosis
Diagnoses of cerebrovascular disease may include:[3]
- medical history
- physical exam
- neurological examination.
- acute stroke imaging is generally performed in significant symptoms of new onset.
It is important to differentiate the symptoms caused by a stroke from those caused by syncope (fainting) which is also a reduction in cerebral blood flow, almost always generalized, but they are usually caused by systemic hypotension of various origins: cardiac arrhythmias, myocardial infarction, hemorrhagic shock, among others.[50]
Treatment
Treatment for cerebrovascular disease may include medication, lifestyle changes, and surgery, depending on the cause.[4]
Examples of medications are:
- antiplatelets (aspirin, clopidogrel)
- blood thinners (heparin, warfarin)
- antihypertensives:
- ACE inhibitors
- beta blockers
- calcium channel blockers - in particular Nimodipine reduces the incidence and severity of ischemic deficits in patients with subarachnoid hemorrhage (SAH)[51]
- anti-diabetic medications.
Surgical procedures include:
- endovascular surgery and vascular surgery (for future stroke prevention).
Prognosis
Prognostics factors: Lower Glasgow Coma Scale score, higher pulse rate, higher respiratory rate and lower arterial oxygen saturation level is prognostic features of in-hospital mortality rate in acute ischemic stroke.[52]
Epidemiology

Worldwide, it is estimated there are 31 million stroke survivors, though about 6 million deaths were due to cerebrovascular disease (2nd most common cause of death in the world and 6th most common cause of disability).[54]
Cerebrovascular disease primarily occurs with advanced age; the risk for developing it goes up significantly after 65 years of age. CVD tends to occur earlier than Alzheimer's Disease (which is rare before the age of 80). In some countries such as Japan, CVD is more common than AD.
In 2012, 6.4 million adults from the US had a stroke, which corresponds to 2.7% of the US. This is approximately 129,000 deaths in 2013.[55]
Geographically, a "stroke belt" in the US has long been known, similar to the "diabetes belt" which includes all of Mississippi and parts of Alabama, Arkansas, Florida, Georgia, Kentucky, Louisiana, North Carolina, Ohio, Pennsylvania, South Carolina, Tennessee, Texas, Virginia, and West Virginia.[56]
References
- "Stroke symptoms and diagnosis". www.uptodate.com. Retrieved 2017-12-12.
- "Cerebrovascular disease – Introduction – NHS Choices". www.nhs.uk. Retrieved 2015-09-01.
- Serena-Leal, Joaquín; Ustrell-Roig, Xavier (July 2007). "Stroke. Diagnosis and Therapeutic Management of Cerebrovascular Disease | Revista Española de Cardiología (English Version)". www.revespcardiol.org. 60 (7): 753–769. doi:10.1016/S1885-5857(08)60011-0. S2CID 618662. Retrieved 2015-09-01.
- MedlinePlus Encyclopedia: Stroke
- "Who Is at Risk for a Stroke? – NHLBI, NIH". www.nhlbi.nih.gov. Retrieved 2017-11-25.
- Prakash, Dibya (2014-04-10). Nuclear Medicine: A Guide for Healthcare Professionals and Patients. Springer Science & Business Media. p. 142. ISBN 9788132218265.
- "AccessMedicine | Content". accessmedicine.mhmedical.com. Retrieved 2015-11-05.
- "AccessMedicine | Content". accessmedicine.mhmedical.com. Archived from the original on 2016-03-04. Retrieved 2015-11-05.
- Sabiston textbook of surgery : the biological basis of modern surgical practice. Townsend, Courtney M., Jr.; Beauchamp, R. Daniel; Evers, B. Mark; Mattox, Kenneth L. (20th ed.). Philadelphia, PA: Elsevier. 2017. pp. 1900–1937. ISBN 978-0323299879. OCLC 951748294.
{{cite book}}: CS1 maint: others (link) - Salmela, Michael B; Mortazavi, Shabnam; Jagadeesan, Bharathi D; Broderick, Daniel F; Burns, Judah; Deshmukh, Tejaswini K; Harvey, H. Benjamin; Hoang, Jenny; Hunt, Christopher H; Kennedy, Tabassum A; Khalessi, Alexander A; Mack, William; Patel, Nandini D; Perlmutter, Joel S; Policeni, Bruno; Schroeder, Jason W; Setzen, Gavin; Whitehead, Matthew T; Cornelius, Rebecca S; Corey, Amanda S; Corey, A. S (2017). "ACR Appropriateness Criteria ® Cerebrovascular Disease". Journal of the American College of Radiology. 14 (5): S34–S61. doi:10.1016/j.jacr.2017.01.051. PMID 28473091.
- Kuźma, Elżbieta; Lourida, Ilianna; Moore, Sarah F.; Levine, Deborah A.; Ukoumunne, Obioha C.; Llewellyn, David J. (2018). "Stroke and dementia risk: A systematic review and meta-analysis". Alzheimer's & Dementia. 14 (11): 1416–1426. doi:10.1016/j.jalz.2018.06.3061. hdl:2027.42/152961. ISSN 1552-5260. PMC 6231970. PMID 30177276.
- "Vascular dementia - Causes - NHS Choices". www.nhs.uk. Retrieved 2015-09-01.
- Portegies, M.L.P; Koudstaal, P.J; Ikram, M.A (2016). "Cerebrovascular disease". Neuroepidemiology. Handbook of Clinical Neurology. Vol. 138. pp. 239–261. doi:10.1016/b978-0-12-802973-2.00014-8. ISBN 9780128029732. PMID 27637962.
- "Acute ischemic stroke syndromes". www.uptodate.com. Retrieved 2017-12-05.
- "Pediatric Cerebrovascular Disorders". childrensnational.org. Retrieved 2017-12-07.
- "the definition of congenital". Dictionary.com. Retrieved 2017-12-12.
- Kim, H; Al-Shahi Salman, R; McCulloch, C. E; Stapf, C; Young, W. L (2014). "Untreated brain arteriovenous malformation: Patient-level meta-analysis of hemorrhage predictors". Neurology. 83 (7): 590–597. doi:10.1212/wnl.0000000000000688. PMC 4141996. PMID 25015366.
- "Clinical manifestations and diagnosis of intraventricular hemorrhage in the newborn". www.uptodate.com. Retrieved 2017-12-07.
- Joutel, Anne; Corpechot, Christophe; Ducros, Anne; Vahedi, Katayoun; Chabriat, Hugues; Mouton, Philippe; Alamowitch, Sonia; Domenga, Valérie; Cécillion, Michaelle; Maréchal, Emmanuelle; MacIazek, Jacqueline; Vayssière, Céline; Cruaud, Corinne; Cabanis, Emmanuel-Alain; Ruchoux, Marie Madeleine; Weissenbach, Jean; Bach, Jean François; Bousser, Marie Germaine; Tournier-Lasserve, Elisabeth (1996). "Notch3 mutations in CADASIL, a hereditary adult-onset condition causing stroke and dementia". Nature. 383 (6602): 707–710. Bibcode:1996Natur.383..707J. doi:10.1038/383707a0. PMID 8878478. S2CID 4351873.
- "Cerebral autosomal dominant arteriopathy with subcortical infarcts and leukoencephalopathy (CADASIL)". www.uptodate.com. Retrieved 2017-12-09.
- "AANS | Cerebrovascular Disease". www.aans.org. Retrieved 2017-12-11.
- "Cerebrovascular disease – NHS Choices – Risks and prevention". www.nhs.uk. Retrieved 2015-09-01.
- Mitsios, John Peter; Ekinci, Elif Ilhan; Mitsios, Gregory Peter; Churilov, Leonid; Thijs, Vincent (2018). "Relationship Between Glycated Hemoglobin and Stroke Risk: A Systematic Review and Meta‐Analysis". Journal of the American Heart Association. 7 (11): e007858. doi:10.1161/JAHA.117.007858. PMC 6015363. PMID 29773578.
- Alloubani, Aladeen; Saleh, Abdulmoneam; Abdelhafiz, Ibrahim (2018). "Hypertension and diabetes mellitus as a predictive risk factors for stroke". Diabetes & Metabolic Syndrome: Clinical Research & Reviews. 12 (4): 577–584. doi:10.1016/j.dsx.2018.03.009. PMID 29571978. S2CID 4231800.
- Kernan, W. N; Ovbiagele, B; Black, H. R; Bravata, D. M; Chimowitz, M. I; Ezekowitz, M. D; Fang, M. C; Fisher, M; Furie, K. L; Heck, D. V; Johnston, S. C; Kasner, S. E; Kittner, S. J; Mitchell, P. H; Rich, M. W; Richardson, D; Schwamm, L. H; Wilson, J. A; American Heart Association Stroke Council, Council on Cardiovascular Stroke Nursing (2014). "Guidelines for the Prevention of Stroke in Patients with Stroke and Transient Ischemic Attack: A Guideline for Healthcare Professionals from the American Heart Association/American Stroke Association". Stroke. 45 (7): 2160–2236. doi:10.1161/STR.0000000000000024. PMID 24788967.
- Litchfield, W. R; Anderson, B. F; Weiss, R. J; Lifton, R. P; Dluhy, R. G (1998). "Intracranial aneurysm and hemorrhagic stroke in glucocorticoid-remediable aldosteronism". Hypertension. 31 (1 Pt 2): 445–50. doi:10.1161/01.HYP.31.1.445. PMID 9453343.
- Pepin, Melanie; Schwarze, Ulrike; Superti-Furga, Andrea; Byers, Peter H (2000). "Clinical and Genetic Features of Ehlers–Danlos Syndrome Type IV, the Vascular Type". New England Journal of Medicine. 342 (10): 673–680. CiteSeerX 10.1.1.603.1293. doi:10.1056/NEJM200003093421001. PMID 10706896.
- Vlak, Monique HM; Algra, Ale; Brandenburg, Raya; Rinkel, Gabriël JE (2011). "Prevalence of unruptured intracranial aneurysms, with emphasis on sex, age, comorbidity, country, and time period: A systematic review and meta-analysis". The Lancet Neurology. 10 (7): 626–636. doi:10.1016/S1474-4422(11)70109-0. PMID 21641282. S2CID 19706811.
- Thompson, B. Gregory; Brown, Robert D; Amin-Hanjani, Sepideh; Broderick, Joseph P; Cockroft, Kevin M; Connolly, E. Sander; Duckwiler, Gary R; Harris, Catherine C; Howard, Virginia J; Johnston, S. Claiborne (Clay); Meyers, Philip M; Molyneux, Andrew; Ogilvy, Christopher S; Ringer, Andrew J; Torner, James; American Heart Association Stroke Council, Council on Cardiovascular Stroke Nursing (2015). "Guidelines for the Management of Patients with Unruptured Intracranial Aneurysms". Stroke. 46 (8): 2368–2400. doi:10.1161/STR.0000000000000070. PMID 26089327.
- Debette, Stéphanie (2014). "Pathophysiology and risk factors of cervical artery dissection". Current Opinion in Neurology. 27 (1): 20–28. doi:10.1097/WCO.0000000000000056. PMID 24300790.
- "Spontaneous cerebral and cervical artery dissection: Clinical features and diagnosis". www.uptodate.com. Retrieved 2017-12-09.
- "the definition of idiopathic". Dictionary.com. Retrieved 2017-12-12.
- "Cerebral Ischemia | Columbia Neurosurgery". www.columbianeurosurgery.org. Retrieved 2015-11-05.
- "Stroke: Hope Through Research". www.ninds.nih.gov. Retrieved 2015-11-05.
- Wang, Hai-Rong; Chen, Miao; Wang, Fei-Long; Dai, Li-hua; Fei, Ai-hua; Liu, Jia-fu; Li, Hao-jun; Shen, Sa; Liu, Ming; Pan, Shu-Ming (2015). "Comparison of Therapeutic Effect of Recombinant Tissue Plasminogen Activator by Treatment Time after Onset of Acute Ischemic Stroke". Scientific Reports. 5: 11743. Bibcode:2015NatSR...511743W. doi:10.1038/srep11743. PMC 4513278. PMID 26206308.
- "Neurological disorders: public health challenges" (PDF). 2006.
{{cite journal}}: Cite journal requires|journal=(help) - "adenosine triphosphate | coenzyme". Encyclopedia Britannica. Retrieved 2017-12-12.
- Xing, Changhong; Arai, Ken; Lo, Eng H; Hommel, Marc (2012). "Pathophysiologic Cascades in Ischemic Stroke". International Journal of Stroke. 7 (5): 378–385. doi:10.1111/j.1747-4949.2012.00839.x. PMC 3985770. PMID 22712739.
- "Clinical diagnosis of stroke subtypes". www.uptodate.com. Retrieved 2017-12-12.
- Cipolla, Marilyn J. (2009-01-01). "Anatomy and Ultrastructure". Morgan & Claypool Life Sciences.
{{cite journal}}: Cite journal requires|journal=(help) - Ischemic Stroke at eMedicine
- R., Caplan, Louis (2009). Caplan's stroke : a clinical approach (4th ed.). Philadelphia: Elsevier/Saunders. ISBN 9781416047216. OCLC 460932706.
- "Stroke". MedlinePlus. Retrieved 2015-09-01.
- Stroke Imaging at eMedicine
- Sacco, R. L; Kasner, S. E; Broderick, J. P; Caplan, L. R; Connors, J. J; Culebras, A; Elkind, M. S. V; George, M. G; Hamdan, A. D; Higashida, R. T; Hoh, B. L; Janis, L. S; Kase, C. S; Kleindorfer, D. O; Lee, J.-M; Moseley, M. E; Peterson, E. D; Turan, T. N; Valderrama, A. L; Vinters, H. V; American Heart Association Stroke Council, Council on Cardiovascular Surgery Anesthesia; Council on Cardiovascular Radiology Intervention; Council on Cardiovascular Stroke Nursing; Council on Epidemiology Prevention; Council on Peripheral Vascular Disease; Council On Nutrition, Physical Activity Metabolism (2013). "An Updated Definition of Stroke for the 21st Century: A Statement for Healthcare Professionals from the American Heart Association/American Stroke Association". Stroke. 44 (7): 2064–2089. doi:10.1161/STR.0b013e318296aeca. PMID 23652265.
- Easton, J. Donald; Saver, Jeffrey L.; Albers, Gregory W.; Alberts, Mark J.; Chaturvedi, Seemant; Feldmann, Edward; Hatsukami, Thomas S.; Higashida, Randall T.; Johnston, S. Claiborne; Kidwell, Chelsea S.; Lutsep, Helmi L.; Miller, Elaine; Sacco, Ralph L. (2009). "Definition and evaluation of transient ischemic attack: a scientific statement for healthcare professionals from the American Heart Association/American Stroke Association Stroke Council; Council on Cardiovascular Surgery and Anesthesia; Council on Cardiovascular Radiology and Intervention; Council on Cardiovascular Nursing; and the Interdisciplinary Council on Peripheral Vascular Disease. The American Academy of Neurology affirms the value of this statement as an educational tool for neurologists". Stroke. 40 (6): 2276–2293. doi:10.1161/STROKEAHA.108.192218. ISSN 1524-4628. PMID 19423857.
- Van Gijn, Jan; Kerr, Richard S; Rinkel, Gabriel JE (2007). "Subarachnoid haemorrhage". The Lancet. 369 (9558): 306–318. doi:10.1016/S0140-6736(07)60153-6. PMID 17258671. S2CID 29126514.
- Xi, Guohua; Keep, Richard F; Hoff, Julian T (2006). "Mechanisms of brain injury after intracerebral haemorrhage". The Lancet Neurology. 5 (1): 53–63. doi:10.1016/S1474-4422(05)70283-0. PMID 16361023. S2CID 30474999.
- Meretoja, A; Strbian, D; Putaala, J; Curtze, S; Haapaniemi, E; Mustanoja, S; Sairanen, T; Satopaa, J; Silvennoinen, H; Niemela, M; Kaste, M; Tatlisumak, T (2012). "SMASH-U: A Proposal for Etiologic Classification of Intracerebral Hemorrhage". Stroke. 43 (10): 2592–2597. doi:10.1161/STROKEAHA.112.661603. PMID 22858729.
- Bonanno, Fabriziogiuseppe (2011). "Clinical pathology of the shock syndromes". Journal of Emergencies, Trauma, and Shock. 4 (2): 233–43. doi:10.4103/0974-2700.82211. PMC 3132364. PMID 21769211.
- Research, Center for Drug Evaluation and (2018-11-03). "Postmarket Drug and Biologic Safety Evaluations Completed from July 2016 – September 2016". FDA.
- Shah, Bhupendra; Bartaula, Bijay; Adhikari, Janak; Neupane, Harishankar; Shah, Birendraprasad; Poudel, Gunaraj (2017). "Predictors of in-hospital mortality of acute ischemic stroke in adult population". Journal of Neurosciences in Rural Practice. 8 (4): 591–594. doi:10.4103/jnrp.jnrp_265_17. PMC 5709883. PMID 29204020.
- "WHO Disease and injury country estimates". World Health Organization. 2009. Retrieved Nov 11, 2009.
- Ward, Helen; Toledano, Mireille B.; Shaddick, Gavin; Davies, Bethan; Elliott, Paul (2012-05-24). Oxford Handbook of Epidemiology for Clinicians. OUP Oxford. p. 310. ISBN 9780191654787.
- "FastStats". www.cdc.gov. Retrieved 2015-09-01.
- BORHANI NO (1965). "Changes and Geographic Distribution of Mortality from Cerebrovascular Disease". American Journal of Public Health and the Nation's Health. 55 (5): 673–81. doi:10.2105/AJPH.55.5.673. PMC 1256296. PMID 14287837.
Further reading
- Chan, Pak H. (2002-03-28). Cerebrovascular Disease: 22nd Princeton Conference. Cambridge University Press. ISBN 9781139439657.
- Mark, S. D; Wang, W; Fraumeni, J. F; Li, J.-Y; Taylor, P. R; Wang, G.-Q; Guo, W; Dawsey, S. M; Li, B; Blot, W. J (1996). "Lowered Risks of Hypertension and Cerebrovascular Disease after Vitamin/Mineral Supplementation: The Linxian Nutrition Intervention Trial". American Journal of Epidemiology. 143 (7): 658–664. doi:10.1093/oxfordjournals.aje.a008798. PMID 8651227.
- Ning, Mingming; Lopez, Mary; Cao, Jing; Buonanno, Ferdinando S; Lo, Eng H (2012). "Application of proteomics to cerebrovascular disease". Electrophoresis. 33 (24): 3582–3597. doi:10.1002/elps.201200481. PMC 3712851. PMID 23161401.
