Eccrine carcinoma
Eccrine carcinoma is a rare skin condition characterized by a plaque or nodule on the scalp, trunk, or extremities.[1]: 669 It originates from the eccrine sweat glands of the skin, accounting for less than 0.01% of diagnosed cutaneous malignancies.[2] Eccrine carcinoma tumors are locally aggressive, with a high rate of recurrence. Lack of reliable immunohistochemical markers and similarity to other common tumors has made identification of eccrine carcinoma difficult.[2]
| Eccrine carcinoma | |
|---|---|
| Other names | Syringoid carcinoma |
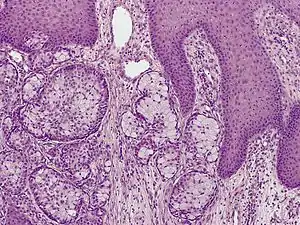 | |
| Eccrine carcinoma, alveolar type | |
| Specialty | Dermatology |
Most eccrine carcinomas which have not spread can be cured by wide local excision. However, metastatic disease carries a poor prognosis.[2]
Symptoms
Eccrine carcinoma results in brown, bluish, erythematous skin lesions across the body. Common regions where lesions are found are in the lower extremities (35%), head and neck (24%), and upper extremities (14%).[3][4]
Complications
Metastases and/or antagonistic side effects can occur after surgical excision of tumors.[2]
Types
Eccrine carcinomas include porocarcinoma, hidradenocarcinoma, malignant spiradenoma carcinoma, malignant cylindroma, syringoid eccrine carcinoma, microcystic adnexal carcinoma, mucinous carcinoma, adenoid cystic carcinoma, and ductal papillary adenocarcinoma.[2] Other tumors not classified include eccrine ductal carcinoma, basaloid eccrine carcinoma, clear cell eccrine carcinoma and non-specified sweat gland carcinomas.[2]
Causes
There is no research yet as to what causes Eccrine carcinoma.[2]
Diagnosis
A skin biopsy is the most common test used to diagnose eccrine carcinoma.[2] The biopsy will detect growth of new or abnormal tissue. Another test that can be performed is using immunohistochemistry, but it is inconsistent.[2] Markers used to detect eccrine carcinoma consist of carcinoembryonic antigen, progesterone receptors, estrogen receptors, epithelial membrane antigen, pancytokeratins, and cytokeratin 7.[5][6]
Treatment
Wide surgical excision is the mainstay of treatment.[2][7] Chemotherapy and radiation therapy have been used in metastatic disease.[2][8]
Prognosis
In the absence of metastasis, local excision is curative in 70–80% of cases.[9] Metastatic eccrine carcinoma has a relative mortality rate of 65% (with local lymph node involvement alone) to 80% (with distant metastases), and the 10-year overall survival rate is 9%.[3][9]
Frequency
Eccrine carcinoma accounts for 0.005-0.01% of diagnosed cutaneous malignancies.[9]
See also
References
- James, William D.; Berger, Timothy G.; et al. (2006). Andrews' Diseases of the Skin: Clinical Dermatology. Saunders Elsevier. ISBN 0-7216-2921-0.
- Kaseb, Hatem; Babiker, Hani M. (2020), "Cancer, An Overview of Eccrine Carcinoma", StatPearls, StatPearls Publishing, PMID 31082086, retrieved 2020-04-22
- Larson, Kristian; Babiker, Hani M.; Kovoor, Andrew; Liau, Joy; Eldersveld, Jordan; Elquza, Emad (2018). "Oral Capecitabine Achieves Response in Metastatic Eccrine Carcinoma". Case Reports in Oncological Medicine. 2018: 1–5. doi:10.1155/2018/7127048. ISSN 2090-6706. PMC 5852884. PMID 29686913.
- Idrissi Serhrouchni, Karima; Harmouch, Taoufiq; Chbani, Laila; El Fatemi, Hind; Sekal, Mohammed; Hammas, Nawal; Soughi, Meriem; Benchat, Loubna; Amarti, Afaf (2013-02-04). "Eccrine carcinoma: a rare cutaneous neoplasm". Diagnostic Pathology. 8 (1): 15. doi:10.1186/1746-1596-8-15. ISSN 1746-1596. PMC 3570399. PMID 23379908.
- Swanson, P. E.; Cherwitz, D. L.; Neumann, M. P.; Wick, M. R. (1987–2004). "Eccrine sweat gland carcinoma: an histologic and immunohistochemical study of 32 cases*". Journal of Cutaneous Pathology. 14 (2): 65–86. doi:10.1111/j.1600-0560.1987.tb00477.x. ISSN 0303-6987. PMID 2439558. S2CID 1897717.
- Ohnishi, Takamitsu; Kaneko, Sakae; Egi, Motoko; Takizawa, Hajime; Watanabe, Shinichi (2002–2010). "Syringoid Eccrine Carcinoma". The American Journal of Dermatopathology. 24 (5): 409–413. doi:10.1097/00000372-200210000-00007. ISSN 0193-1091. PMID 12357203. S2CID 20147934.
- Moy, Ronald L.; Rivkin, Jonathan E.; Lee, Hyo; Brooks, Walter S.; Zitelli, John A. (1991–2005). "Syringoid eccrine carcinoma". Journal of the American Academy of Dermatology. 24 (5): 857–860. doi:10.1016/0190-9622(91)70133-m. ISSN 0190-9622. PMID 2050853.
- Sidiropoulos, M.; Sade, S.; Al-Habeeb, A.; Ghazarian, D. (2011-06-04). "Syringoid eccrine carcinoma: a clinicopathological and immunohistochemical study of four cases". Journal of Clinical Pathology. 64 (9): 788–792. doi:10.1136/jclinpath-2011-200069. ISSN 0021-9746. PMID 21642659. S2CID 46508699.
- Salih, Abdulwahid M.; Kakamad, F.H.; Essa, Rawand A.; Rauf, Goran M.; S.A., Masrur; H.M., Shvan; Q.S., Rawezh; A.H., Hunar; A.H., Dahat; Othman, Snur (2017). "Porocarcinoma: A systematic review of literature with a single case report". International Journal of Surgery Case Reports. 30: 13–16. doi:10.1016/j.ijscr.2016.10.051. ISSN 2210-2612. PMC 5128823. PMID 27898349.