Lines of Zahn
Lines of Zahn are a characteristic of thrombi. They have layers, with lighter layers of platelets and fibrin, and darker layers of red blood cells. They are more present on thrombi formed with faster blood flow, more so on thrombi from the heart and aorta. They are only seen on thrombi formed before death. They are named after German–Swiss pathologist Friedrich Wilhelm Zahn.
| Lines of Zahn | |
|---|---|
.jpg.webp) | |
| A recent pulmonary thrombo-embolus with prominent lines of Zahn. The pale areas consist of fibrin and platelets. The red areas consist of erythrocytes. | |
| Specialty | Pathology |
| Causes | Thrombosis |
Definition
Lines of Zahn are a characteristic of thrombi.[1] They have visible and microscopic alternating layers (laminations).[2][3] Platelets mixed with fibrin form lighter layers.[2] Red blood cells form darker layers.[2] Sometimes, the term "lines of Zahn" only refers to the lighter layers.[4]
Evaluation
Lines of Zahn can be used to confirm diagnosis of a thrombus.[1] Their presence implies thrombosis at a site of rapid blood flow that happened before death. They are more common in thrombi formed in the heart or aorta.[5] In veins or smaller arteries, where flow is not as constant, they occur less frequently.[5] They are also only seen on thrombi formed when blood is flowing. This is a distinguishing marker between thrombi that formed before death and after death.
History
Lines of Zahn are named after German–Swiss pathologist Friedrich Wilhelm Zahn.[6]
Additional images
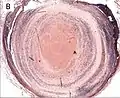 Thrombus showing circumferential lines of Zahn.
Thrombus showing circumferential lines of Zahn. Low magnification micrograph showing laminations in a thrombus in a fatal pulmonary embolism. H&E stain.
Low magnification micrograph showing laminations in a thrombus in a fatal pulmonary embolism. H&E stain. Intermediate magnification micrograph showing laminations in a thrombus in a fatal pulmonary embolism. H&E stain.
Intermediate magnification micrograph showing laminations in a thrombus in a fatal pulmonary embolism. H&E stain. High magnification micrograph showing laminations in a thrombus in a fatal pulmonary embolism. H&E stain.
High magnification micrograph showing laminations in a thrombus in a fatal pulmonary embolism. H&E stain.
References
- "11 - Thrombosis". Thrombosis and Bleeding Disorders - Theory and Methods. Academic Press. 1971. pp. 488–534. doi:10.1016/B978-0-12-077750-1.50015-5. ISBN 978-0-12-077750-1.
- Lee R, Adlam D, Clelland CA, Channon KM (May 2012). "Lines of Zahn in coronary artery thrombus". European Heart Journal. 33 (9): 1039. doi:10.1093/eurheartj/ehs028. PMID 22345124.
- Saha P, Humphries J, Modarai B, Mattock K, Waltham M, Evans CE, et al. (March 2011). "Leukocytes and the natural history of deep vein thrombosis: current concepts and future directions". Arteriosclerosis, Thrombosis, and Vascular Biology. 31 (3): 506–512. doi:10.1161/ATVBAHA.110.213405. PMC 3079895. PMID 21325673.
- Stone J, Hangge P, Albadawi H, Wallace A, Shamoun F, Knuttien MG, et al. (December 2017). "Deep vein thrombosis: pathogenesis, diagnosis, and medical management". Cardiovascular Diagnosis and Therapy. 7 (Suppl 3): S276–S284. doi:10.21037/cdt.2017.09.01. PMC 5778510. PMID 29399531.
- Heo JH, Nam HS, Kim YD, Choi JK, Kim BM, Kim DJ, Kwon I (January 2020). "Pathophysiologic and Therapeutic Perspectives Based on Thrombus Histology in Stroke". Journal of Stroke. 22 (1): 64–75. doi:10.5853/jos.2019.03440. PMC 7005358. PMID 32027792.
- Stegman JK, ed. (2006), Stedman's Medical Dictionary (28th ed.), Baltimore, MD: Lippincott, Williams, & Wilkins
Further reading
- Kumar V, Abbas AK, Fausto N (2005). Robbins & Cotran Pathologic Basis of Disease (7th ed.). Pennsylvania: Elsevier/Saunders. ISBN 978-0-7216-0187-8.
- Cross SS, ed. (2013). "Chapter 6: Thrombosis, Embolism and Infarction". Underwood's pathology : a clinical approach (PDF) (6th ed.). Edinburgh: Churchill Livingstone. ISBN 978-0-7020-4672-8.