Nursing home
A nursing home is a facility for the residential care of elderly or disabled people.[1] Nursing homes may also be referred to as skilled nursing facility (SNF), long-term care facilities, old people's homes, assisted living facilities[2] care homes, rest homes, convalescent homes or convalescent care. Often, these terms have slightly different meanings to indicate whether the institutions are public or private, and whether they provide mostly assisted living, or nursing care and emergency medical care. Nursing homes are used by people who do not need to be in a hospital, but cannot be cared for at home. The nursing home facility nurses have the responsibilities of caring for the patients' medical needs and also the responsibility of being in charge of other employees, depending on their ranks. Most nursing homes have nursing aides and skilled nurses on hand 24 hours a day.

In the United States, while nearly 1 in 10 residents age 75 to 84 stays in a nursing home for five or more years, nearly 3 in 10 residents in that age group stay less than 100 days, the maximum duration covered by Medicare, according to the American Association for Long-Term Care Insurance. Some nursing homes also provide short-term rehabilitative stays following surgery, illness, or injury. Services may include physical therapy, occupational therapy, or speech-language therapy. Nursing homes also offer other services, such as planned activities and daily housekeeping. Nursing homes may offer memory care services, often called dementia care.[3]
History
.jpg.webp)
From before the 17th century to modern day, many families care for their elders in the family's home. While this is still common practice for many communities and families around the world, this has become increasingly more difficult over time as life expectancy increases, family size decreases, and increased expertise in caring for a person with a chronic disease. In the 21st century, nursing homes have become a standard form of care for most aged and incapacitated persons to account for those complexities. Nearly 6 percent of older adults are sheltered in residential facilities that provide a wide range of care. Yet such institutions have not always existed; rather, their history and development reflect relatively recent demographic and political realities that shape the experience of growing old.[4]
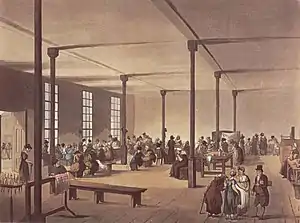
In the 17th century, poorhouses (also referred to as almshouses) originated in England as municipalities were expected to care for their poor. Orphans, people determined to be mentally ill, and elderly people were often placed into these living commons while able-bodied individuals were expected to work and could be imprisoned if they refused. This model was brought to North America by English settlers.[5] Before the 19th century, no age-restricted institutions existed for long-term care; elderly individuals, who needed shelter because of incapacity, impoverishment, or family isolation, often ended their days in an almshouse. Placed alongside people deemed insane, people who were inebriated, or people who were homeless, they were simply categorized as part of the community's most needy recipients. Poorhouses gave a place where they could be given shelter and daily meals.
In the 1800s in the US, women's and church groups began to establish special homes for the elderly persons. Often concerned that individuals of their own ethnic or religious communities might die alongside the most despised society. This led to the creation of private care facilities for the elderly in these communities.[4] Poorhouses continued to exist into the early 20th century, despite the criticism of the poor conditions of the poorhouses. In the US, the Great Depression overwhelmed the poorhouses, but not enough space and funding. Due to muckraking in the 1930s, the less-than-favorable living conditions of the poorhouses were exposed to the public. This led to the provision of the Social Security Act (1935) to only give people their pension if they did not live in poorhouses, but could live in private institutions.[6]
In the US, poorhouses were then replaced with residential living home, known as board-and-care homes or convalescent homes. These board-and-care homes provided basic levels of care and meals in a private setting for a specific fee. Board-and-care homes proved to be a success and by World War II, the new way of nursing homes began to take shape. As the times continued to change, the government identified the issue of people spending extensive amounts of time in hospitals. To combat these long stays in short-term settings, board-and-care homes began to convert into something more public and permanent that was state and federally funded. From this, by 1965 nursing homes were a solid fixture. Nursing homes were a permanent residence where the elderly and disabled could receive any necessary medical care and receive daily meals. These nursing homes showed improvement in maintaining care and cleanliness standards in comparison to almshouses and poorhouses. From the 1950s through the 1970s, the dynamics of nursing homes began changing significantly. In the United States, Medicare and Medicaid began to make up much of the money that would filter through the homes and the 1965 amendment laws enforced nursing homes to comply with safety codes and required registered nurses to be on hand at all times. Additionally, nursing homes may sue children for the costs of caring for their parents in jurisdictions which have filial responsibility laws. Later in 1987, in the U.S. the Nursing Reform Act was introduced to begin defining the different types of nursing home services and later added the Residents' Bill of Rights.[7]
In the UK, after World War II many soldiers and civilians needing hospital care due to casualties during the war were planced in the hospital along with the many elderly patients present there, leading to overcrowding. The implementation of the NHS in 1948 and the abolishment of the Old Poor Law allowed for the creation of what would become modern day, public nursing homes. In the 1950s, Professor Peter Townsend brought to light the discrepancies the standard of care between the publicly and privately funded cares homes, leading to health policy reforms that assured the standard care practices for the elderly living in NHS funded care homes. The 1980s and 1990s saw care homes becoming a large industry in the UK. Thus, policies ensuring that private care homes are regulated (Registered Homes Act 1984) and patient needs are met (Care Standards Act of 2000) were established.[7]
Today, nursing homes are varied. Some nursing homes still resemble a hospital while others look more like a home. Nursing home residents can pay for their care out of pocket or with government assistance. In the U.S., others may receive Medicare for a short time, while in other countries, public assistance may be available, and some may use long-term insurance plans. Across the spectrum, most nursing homes in the U.S. will accept Medicaid as a source of payment.[8]
Considerations
Below are a few reasons to consider a nursing home
- managing a worsening and progressive disease such as Alzheimers
- after a recent hospital admission and not ready to transition to independently caring for oneself at home
- when medical needs at home become unmanageable by the primary caregiver at home.[9]
When looking into nursing homes, consider what activities and/or medical needs patients one would need from the nursing home. Also consider finances, such as medical insurance and personal funds. Ensure the nursing home is properly licensed and has qualified staff. If time allows, visit the nursing home in person to receive a walk through of the facility and if given the opportunity to speak with a guest or family member of guest, ask about their experience thus far.
Staff
Nursing home employees are all required to be licensed or uphold a certificate in the state of which they work. In most facilities, nursing homes are required to provide enough staff to adequately care for residents. In the U.S., for instance, nursing homes must have at least one registered nurse (RN) available for at least 8 straight hours a day throughout the week, and at least one licensed practical nurse (LPN) on duty 24 hours a day.[10] Direct care nursing home employees usually include registered nurses, licensed practical nurses, social workers, certified nursing assistants, and physical therapists, amongst others.
Nurses
Nursing homes require assessment and monitoring of residents by a registered nurse (RN) who is typically required to have between two and six years of education. The RN's job duties include implementing care plans, administering medications, recording and maintaining accurate reports for each resident, monitoring and recording medical changes, and providing direction to the nursing assistants and licensed practical nurses (LPN).[11] RNs are not required to choose a specialization. To gain recognition as a specialized nurse professional, RNs typically need education in their specialized field, and further experience through clinical practices. LPNs are typically required to have a year of training before working with any patients. The LPN monitors residents' well-being and administers treatments and medications, such as dressing wounds and dispensing prescribed drugs. LPNs are responsible for patients' direct bed care and carry out a daily routine.
Nursing assistants
A nursing assistant provides basic care to patients while working directly under a LPN or RN. These basic care activities, also referred to as activities of daily living, can include assisting with bathing and dressing residents, helping residents with meals, either serving them or with feeding, transferring to and from the bed or wheelchair, making and cleaning beds, assisting with toileting, and answering call lights. Nursing assistants' official titles can vary between jurisdictions and facilities. They can include Certified Nursing Assistants (CNAs), nursing aides, caregivers, patient care associates, patient care technicians, personal care attendants (PCAs), and care assistants.
Physicians
At skilled nursing facilities, in addition to required 24 hour skilled nursing, a licensed physician supervises individual patients.[9] At nursing homes other than skilled nursing facilities, patients receive care from physicians not affiliated with the nursing home. These physicians are typically employed by a private agency that sends physicians to nursing homes per the request of the patient, nursing home, or patient's family. The majority of these physicians are family medicine doctors or internists; however, some specialists such as cardiologist or nephrologist may also make independent visits to supplement their care.[12]
Administration
Depending on the size of the nursing home, a nursing home may have either a nursing home administrator or an executive director. Some nursing homes may have both, but their job duties are similar and can include overseeing staff, supplying medical supplies, and financial matters. Some nursing homes also have human resources personnel, who are in charge of all aspects of hiring new employees. Human resources job duties vary but can also include coordinating payroll, organizing orientation programs for new employees, interviewing, disciplinary actions, and ensuring compliance with federal and state laws.[13] Nursing homes are usually licensed and heavily regulated under governing legislation. Compliance with the federal and state legislatures are reviewed regularly for adherence to strict standards of building codes, care plans, behavior and altercations between residents, nutrition and dietary services, medical services, nursing and personal care, religious and spiritual practices, pets, and recreational programs.[14]
Housekeeping
Housekeepers perform everyday cleaning and upkeep in nursing homes. They play a huge part in ensuring that nursing homes are kept clean and free of disease causing agents. Housekeepers have a long list of duties which include cleaning floors, changing linens, disinfecting bathrooms, changing towels, washing clothes, emptying trashcans, sanitizing rooms, replenishing supplies, dusting, vacuuming, and keeping windows and woodwork clean. These duties can vary from facility to facility but it will overall include basic cleaning. Housekeeping does not require any licensure or schooling, but some jobs may prefer experienced housekeepers.[15]
Recreational staff
Recreational staff usually include an activity director and possibly activity assistants depending on the size of the nursing home. Activities aim to meet each resident's emotional, intellectual, physical, social, spiritual, and vocational needs. The transition from being independent to having to depend on others and be away from home is oftentimes very difficult, which is why activities are important to combat depression and anxiety.[16] Some of the different activities that may be offered include hosting birthday parties, celebrating holidays, book clubs, musical events, outdoor activities, discussion and social groups, exercise, arts and crafts, pet therapy, religious services and community outings. Volunteer involvement is also an important part of nursing home activities given that volunteers can act as a link between the nursing home and the outside community.
Therapy
Occupational therapy
One of the many services offered in a nursing home is occupational therapy. Occupational therapy may be necessary following an injury or illness in order to regain skills and to receive support during any physical or cognitive changes.[17] Occupational therapy will focus on activities of daily living such as bathing, dressing, grooming. Occupational therapy also assists with instrumental activities of daily living which include home and financial management, rest and sleep, education, work, play, leisure, and social participation. Occupational therapists work to allow the person to safely and comfortably reintegrate into society by practicing public dining, transferring to different surfaces (chairs, beds, couches etc.), and will assess the need for any home modifications or safety equipment to ensure a proper and safe transition. When a cognitive and/or perceptual deficit is presented, therapists will work with the person by teaching strategies to maximize memory, sequencing and attention span length.[18]
Physical therapy

Another important service found in a nursing home is physical therapy. Physical therapy may be necessary following an injury, illness or surgery. Physical therapy works with the person to help them regain strength, endurance, flexibility, balance and range of motion. Physical therapy is also used as a way of preventing injuries and accidents by focusing on restoring mobility, increasing fitness levels, reducing pain and overall reaching a certain point of independence. There are many conditions that can benefit from receiving physical therapy in a nursing home, these conditions include arthritis, pain associated with cancer, dementia, Alzheimer's, stroke and incontinence.[19][20]
Speech language therapy
Speech-language pathology is another service found in a nursing home. Speech language pathologists specialize in working with those who have a difficult time with language and/or speech, usually following an injury or an underlying diagnoses.[21] The SLP will evaluate the persons speech. If the person is having trouble with speech, this points to an issue with coordinating the movements and muscles used to produce speech. While trouble with language points to the person having difficulty with understanding what they are hearing and seeing. The SLP will also look at difficulty with swallowing food and will evaluate the person in order to figure out which part of the swallowing process is not working. Some of the many speech disorders worked with by the SLP are:
- phonology meaning the speech patterns used,
- apraxia meaning difficulty with coordinating the movements needed to make sounds,
- receptive language meaning difficulty understanding language,
- fluency meaning stuttering,
- expressive language meaning difficulty using language, and many other disorders.
Elder abuse
Elder abuse is more prevalent in hospitalized settings including nursing homes than in the general community.[22] There are three major types of abuses reported in nursing homes: physical, emotional, and sexual abuse.
Physical abuse is the intention or action to hurt an elderly person resulting in scars and bruising.
Emotional abuse occurs when an employee makes verbal threats and continuously degrades the patient, resulting in the patient experiencing mood swings, anxiety, and depression.
Sexual abuse is when an elderly patient is being forced into unwanted sexual activity by an employee, resident or visitor, usually attempted and reported when the patient is sleeping, sick, or weak.
Nursing home neglect is similar to elder abuse. It is when employees begin to repeatedly ignore and leave a patient alone, neglect the patient's personal hygiene like bathing and brushing of teeth, provide the patient with an inadequate amount of food and water, or neglect to provide the patient with the correct amount of medication they require. One factor unique to elder abuse in nursing homes is that many nursing home contracts require residents to sign delegation clauses, giving up their right to trial by jury and instead using an Arbitrator to settle disputes.[23]
By country
Canada
Long-term care facilities exist under three major types: privately owned, non-profit/charitable, and municipal. Regardless of their ownership, aspects of funding, admission criteria, and cost to the individuals are all regulated by their respective provincial governments.[24] As medical care is publicly funded in Canada, all long-term care facilities receive funding from provincial governments for the health care component of the residence – the nurses and personal support workers. Residents pay daily rates for 'room and board' (accommodation and food) that are determined by the type of room chosen, either shared or private. Provincial governments manage waiting lists for long-term care facilities. People who cannot afford to pay the monthly fees receive subsidies, and no one is refused due to inability to pay.[25]
United Kingdom
In the United Kingdom, care homes and care homes with nursing are regulated by different organisations in England, Scotland, Wales and Northern Ireland. To enter a care home, a candidate patient needs an assessment of needs and of their financial condition from their local council. The candidate may also have an assessment by a nurse, should the patient require nursing care. The cost of a care home is means tested in England.
Care homes for adults in the UK are regulated by Care Quality Commission, which replaced the Commission for Social Care Inspection, and each care home is inspected at least every three years. In Wales the Care Standards Inspectorate for Wales has responsibility for oversight, In Scotland Social Care and Social Work Improvement Scotland otherwise known as the Care Inspectorate, and in Northern Ireland the Regulation and Quality Improvement Authority in Northern Ireland.
In 2002, nursing homes became known as care homes with nursing, and residential homes became known as care homes.[26]
As of April 2009, the lower capital limit is £13,500. At this level, all income from pensions, savings, benefits and other sources, except a "personal expenses allowance" (currently £21.90), goes towards paying the care home fees. The local council pays the remaining contribution provided the room occupied is not more expensive than the local council's normal rate. The NHS has full responsibility for funding the whole placement if the resident is in a care home with nursing that meets the criteria for NHS continuing Health Care. This is identified by a multidisciplinary assessment process.[27]
In May 2010, a coalition government announced the formation of an independent commission on the funding of long-term care, which was due to report within a 12-month time frame on the financing of care for an ageing population. It delivered its recommendations on Monday 4 July 2011. The Care Quality Commission have themselves implemented a re-registration process, completed in October 2010, which will result in a new form of regulation being outlined in April 2011.[28]
In 2020 it emerged that some UK care home residents had blanket Do Not Attempt Resuscitation (DNACPR) orders applied during the COVID-19 pandemic.[29] These decisions were made without discussion with the patients involved, and the practice is being investigated by the Care Quality Commission.[30]
United States
In the United States, there are three main types of nursing facilities (NFs).
An intermediate care facility (ICF) is a health care facility for individuals who are disabled, elderly, or non-acutely ill, usually providing less intensive care than that offered at a hospital or skilled nursing facility. Typically an ICF is privately paid by the individual or by the individual's family. An individual's private health insurance and/or a third party service like a hospice company may cover the cost. Board and Care Homes are special facilities designed to provide those who require assisted living services both living quarters and proper care. Often referred to as residential care homes, these facilities can either be located in a small residential home or a large modern facility. In fact, a large majority of board and care homes are designed to accommodate fewer than 6 people. Board and care homes are typically staffed by licensed professionals, including nurses, doctors and other medical professionals. These facilities are highly regulated in order to ensure that the best possible care is being provided for the residents. Board and care homes offer residents 24-hour assistance, making them a highly popular choice for those in need of regular assistance.
Assisted living residences or assisted living facilities (ALFs) are housing facilities for people with disabilities. These facilities provide supervision or assistance with activities of daily living (ADLs); ALFs are an eldercare alternative on the continuum of care for people, for whom independent living is not appropriate but who do not need the 24-hour medical care provided by a nursing home and are too young to live in a retirement home. Assisted living is a philosophy of care and services promoting independence and dignity.[31][32][33]
A skilled nursing facility (SNF) is a nursing home certified to participate in, and be reimbursed by Medicare. Medicare is the federal program primarily for the aged (65+) who contributed to Social Security and Medicare while they were employed. Medicaid is the federal program implemented with each state to provide health care and related services to those who are below the poverty line. Each state defines poverty and therefore Medicaid eligibility. Those eligible for Medicaid may be low-income parents, children (including those in State Children's Health Insurance Programs (SCHIPs) and maternal-child wellness and food programs),[34] seniors, and people with disabilities. The Centers for Medicare and Medicaid Services is the component of the U.S. Department of Health and Human Services (DHHS) that oversees Medicare and Medicaid. A large portion of Medicare and Medicaid dollars is used each year to cover nursing home care and services for the elderly and disabled. State governments oversee the licensing of nursing homes. In addition, states have a contract with CMS to monitor those nursing homes that want to be eligible to provide care to Medicare and Medicaid beneficiaries. Congress established minimum requirements for nursing homes that want to provide services under Medicare and Medicaid. These requirements are broadly outlined in the Social Security Act, which also entrusts the Secretary of Health and Human Services with the responsibility of monitoring and enforcing these requirements. CMS is also charged with the responsibility of working out the details of the law and how it will be implemented, which it does by writing regulations and manuals.[35]
See also
- American Medical Directors Association
- Care Quality Commission
- Child care
- Elderly care
- Home care
- International Association of Homes and Services for the Aging
- List of companies operating nursing homes
- Retirement community
- Caring for people with dementia
References
- "Types of Care Facilities". Care givers library.
- old people's home in the Cambridge Advanced Learner's Dictionary
- Esposito, Lisa (1 June 2016). "What Nursing Home 'Memory Care' Means". U.S. News & World Report. Retrieved 29 July 2017.
- "Nursing Homes: History | Encyclopedia.com". www.encyclopedia.com. Retrieved 8 September 2021.
- Blakemore, Erin. "Poorhouses Were Designed to Punish People for Their Poverty". HISTORY. Retrieved 8 September 2021.
- Watson, Sidney D. (March 2012). "From Almshouses to Nursing Homes and community care: Lessons from Medicaid History". Georgia State University Law Review. 26 (3, Spring 2010).
- "A history of care homes". www.carehome.co.uk. Retrieved 13 September 2021.
- "Nursing Facilities | Medicaid". www.medicaid.gov. Retrieved 20 September 2021.
- "A Guide to Nursing Homes - HelpGuide.org". www.helpguide.org. Retrieved 8 September 2021.
- "A Guide to Nursing Homes - HelpGuide.org". www.helpguide.org. Retrieved 13 September 2021.
- "What Nurses Do". American Nurses Association. Archived from the original on 12 July 2015.
- "Role of the Attending Physician in the Nursing Home | AMDA". paltc.org. Retrieved 8 September 2021.
- "Human Resources". HealthCareers.com.
- "A Guide to the Long-Term Care Homes Act, 2007 and Regulation 79/10" (PDF).
- Erika Winston. "Job Description of Senior Living Housekeeper". work.chron.com. Houston Chronicle.
- Petrea, RN, Jennifer (27 June 2014). "Importance of Being Social in a Nursing Home". McKnight's Long Term Care News. Retrieved 24 March 2021.
- "About Occupational Therapy". AOTA.org.
- "Occupational Therapy's Role in Skilled Nursing Facilities" (PDF). AOTA.org.
- Ling, Shari M. (13 October 2011). "Rehabilitation of Older Adult Patients with Arthritis". Johns Hopkins Arthritis Center. Retrieved 29 July 2017.
- "Physical Therapy". University Hospitals. St. John Medical Center. Retrieved 29 July 2017.
- "Speech Language Pathology in Long Term Care". SpeechPathology.com.
- Eubank, Kathryn J.; Pierluissi, Edgar; Landefeld, C. Seth (2014), Williams, Brie A.; Chang, Anna; Ahalt, Cyrus; Chen, Helen (eds.), "Hospital Care", Current Diagnosis & Treatment: Geriatrics (2 ed.), New York, NY: McGraw-Hill Education, retrieved 13 September 2021
- Edwards, Haley Sweetland (16 November 2017). "An 87-Year-Old Nun Said She Was Raped in Her Nursing Home. Here's Why She Couldn't Sue". Time Magazine.
- "This is Long Term Care 2016" (PDF).
- "Long-term care overview". ontario.ca.
- "NHS Continuing Healthcare, NHS funded healthcare and intermediate care" (PDF). Age Concern. August 2007. Archived from the original (PDF) on 8 March 2012. Retrieved 15 June 2010.
- as detailed on the Department of Health website
- "Dilnot Commission on Funding of Care and Support". Age UK. Retrieved 28 April 2013.
- Booth, R (1 April 2020). "UK healthcare regulator brands resuscitation strategy unacceptable". The Guardian. Retrieved 8 March 2021.
- Booth, R (12 October 2020). "Inquiry begins into blanket use in England of Covid 'do not resuscitate' orders". The Guardian. Retrieved 8 March 2021.
- Heumann, L.F. (2004). Assisted living for low-income and frail older persons from the housing and built environmental perspective. In: J. Pynoos, P. Hollander Feldman, & J. Ahrens, "Linking Housing and Services for Older Adults". London: The Haworth Press.
- Tillery, D. (2004). Supportive housing initiatives in Arkansas. In: J. Pynoos et al, Linking Housing and Services for Older Adults." Binghamton, NY: The Haworth Press.
- Vinton, L. (2004). Perceptions of the need for social work in assisted living facilities. "Journal of Social Work in Long-Term Care", 3(1): 85-101.
- Gage B, et al (Feb 2009). Examining Post Acute Care Relationships in an Integrated Hospital System. RTI International. Accessed 2021-03-27.
- "Nursing Home Inspections". medicare.gov. Retrieved 12 October 2012.