Tenosynovial giant cell tumor
Tenosynovial giant cell tumor (TGCT) is a group of rare, typically non-malignant tumors of the joints. TGCT tumors often develop from the lining of joints (also known as synovial tissue).[1][2][2]: 100 [3][3]: 245
| Tenosynovial giant cell tumor | |
|---|---|
| Other names | Localized: Localized pigmented villonodular synovitis (L-PVNS), Giant cell tumor of the tendon sheath (GCT-TS), Nodular tenosynovitis, Localized nodular tenosynovitis, and L-TGCT Diffuse: Pigmented villonodular synovitis (PVNS), Conventional PVNS, and D-TGCT |
 | |
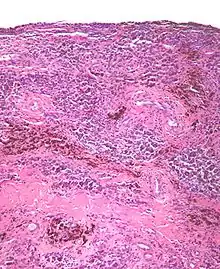
| Micrograph of diffuse TGCT, also known as pigmented villonodular synovitis. H&E stain. | |
| Specialty | Rheumatology |
| Symptoms | Swelling, pain, sensitivity, and/or limited range of motion |
| Complications | Spreading of tumors to surrounding tissues |
| Types | Diffuse and localized |
| Diagnostic method | MRI, biopsy, surgery |
| Treatment | Surgery, CSF1R inhibitors |
Common symptoms of TGCT include swelling, pain, stiffness and reduced mobility in the affected joint or limb.[2]: 102 This group of tumors can be divided into different subsets according to their site, growth pattern, and prognosis.[4][4]: 361 Localized TGCT is sometimes referred to as giant cell tumor of the tendon sheath;[2]: 100 diffuse TGCT is also called pigmented villonodular synovitis (PVNS).[2]: 102
Classification
Classification for TGCT encompasses two subtypes that can be divided according to site – within a joint (intra-articular) or outside of the joint (extra-articular) – and growth pattern (localized or diffuse) of the tumor(s).[2]: 100 [4]: 361 Localized and diffuse subsets of TGCT differ in their prognosis, clinical presentation, and biological behavior, but share a similar manner of disease development.[2]: 100
Localized TGCT
.jpg.webp)
Localized TGCT is sometimes referred to as localized pigmented villonodular synovitis (L-PVNS), giant cell tumor of the tendon sheath (GCT-TS), nodular tenosynovitis, localized nodular tenosynovitis, and L-TGCT.[1]: 1 [2]: 100
The localized form of TGCT is more common.[2]: 100 [3]: 245 Localized TGCT tumors are typically 0.5 cm-4 cm),[2]: 101 develop over years,[2]: 100 are benign and non-destructive to the surrounding tissue, and may reoccur in the affected area.[2]: 101 The most common symptom is painless swelling.[2]: 101 Localized TGCT most often occurs in fingers, but can also occur in other joints.[2][5]
Diffuse TGCT
Diffuse TGCT is sometimes referred to as pigmented villonodular synovitis (PVNS), conventional PVNS, and D-TGCT.[1]: 1 [4]: 361 [6]: 1 [2]: 102
Diffuse TGCT occurs less frequently and is locally aggressive (in some cases, tumors may infiltrate surrounding soft tissue).[3]: 245 [1]: 1 [2]: 102 [6][6]: 1 It most commonly affects people under 40 years old, though the age of occurrence varies.[2]: 102 Diffuse TGCT may occur inside a joint (intra-articular) or outside of a joint (extra-articular). Intra-articular tumors typically occur in the knee (approximately 75% of cases) and hip (approximately 15% of cases).[2]: 102 Extra-articular tumors are usually found in the knee, thigh, and foot.[2]: 101 Symptoms include swelling, pain, sensitivity, and/or limited range of motion.[2]: 102 The rate of reoccurrence is estimated to be 18-46% for intra-articular tumors and 33-50% for extra-articular tumors.[2]: 103 [6]: 1
Mechanism
TGCT tumors grow due to genetic overexpression of colony stimulating factor 1. This causes colony-stimulating factor-1 receptor (CSF1R) cells to accumulate in the joint tissue.[9][10]
Diagnosis
TGCT can be diagnosed by magnetic resonance imaging (MRI), by biopsy, or during surgery.[11][12] The disorder is difficult to identify and is often not diagnosed for years due to nonspecific symptoms or a general paucity of symptoms.[13] TGCT cases are often misdiagnosed as osteoarthritis,[14] localized trauma,[15] sports injuries,[16][17] xanthomas,[18] or other conditions.[19] One study of 122 diffuse TGCT patients found that the average delay in diagnosis was 2.9 years.[20]
Treatment
Surgery has been the most common form of treatment for both localized[2]: 101 [4]: 361 and diffuse TGCT.[2]: 103 [4]: 361 [6]: 1 After surgery, patients may receive physical therapy in order to help rehabilitate affected joints.[16][8] However, recurrence of TGCT after surgery is common,[14] with a higher rate of recurrence for diffuse TGCT than for localized TGCT.[4]: 361 In cases of recurrent or resistant disease, multiple surgeries, total joint arthroplasties, or amputation may be required.[6]: 1
A multidisciplinary approach, supplementing surgery with radiotherapy or other treatments, can also improve outcomes in cases of recurrent TGCT.[21] In the late 2010s, treatment with CSF1R inhibitors emerged as an option[22] that may help improve functionality for patients with recurrent TGCT or TGCT that is not easily managed by surgery.[4]: 361
Epidemiology
A study conducted in the Netherlands estimated that the worldwide incidence of TGCT is 43 cases per million person-years. The majority – 39 cases per million person-years – were estimated to be localized TGCT; the remaining 4 cases per million person-years were estimated to be diffuse TGCT.[5] TGCT can occur in patients of any age, but people with localized TGCT are typically between 30 and 50 years old,[2]: 100–101 while diffuse TGCT tends to affect people under the age of 40.[2]: 102–103
References
- Lucas, David R. (2012). "Tenosynovial Giant Cell Tumor: Case Report and Review". Archives of Pathology & Laboratory Medicine. 136 (8): 901–906. doi:10.5858/arpa.2012-0165-CR. PMID 22849738.
- Fletcher, C. D.M.; Bridge, J.A.; Hogendoorn, P.; Mertens, F. (2013). WHO Classification of Tumours of Soft Tissue and Bone. Fourth Edition. World Health Organization. ISBN 9789283224341. Archived from the original on July 19, 2016.
- Rateb, Kochbati; Hassen, Ben Ghozlen; Leila, Abid; Faten, Farah; Med Samir, Daghfous (2017). "Giant cell tumor of soft tissues: A case report of extra-articular diffuse-type giant cell tumor of the quadriceps". International Journal of Surgery Case Reports. 31: 245–249. doi:10.1016/j.ijscr.2016.12.019. PMC 5310176. PMID 28199932.
- Ravi, Vinod; Wang, Wei-Lien; Lewis, Valerae O. (2011). "Treatment of tenosynovial giant cell tumor and pigmented villonodular synovitis". Current Opinion in Oncology. 23 (4): 361–366. doi:10.1097/CCO.0b013e328347e1e3. PMID 21577109. S2CID 1608847.
- Mastboom, Monique J L.; Verspoor, Floortje G M.; Verschoor, Arjan J.; Uittenbogaard, Daniël; Nemeth, Banne; Mastboom, Walter J B.; Bovée, Judith V M G.; Dijkstra, P D Sander; Schreuder, H W Bart; Gelderblom, Hans; Van De Sande, Michiel A J.; TGCT study group (2017). "Higher incidence rates than previously known in tenosynovial giant cell tumors". Acta Orthopaedica. 88 (6): 688–694. doi:10.1080/17453674.2017.1361126. PMC 5694816. PMID 28787222.
- Mastboom, Monique J. L.; Verspoor, Floortje G. M.; Gelderblom, Hans; Sande, Michiel A. J. van de (2017). "Limb Amputation after Multiple Treatments of Tenosynovial Giant Cell Tumour: Series of 4 Dutch Cases". Case Reports in Orthopedics. 2017: 1–6. doi:10.1155/2017/7402570. PMC 5506462. PMID 28744388.
- "Clinical Study". The Stone Clinic. Archived from the original (web journal) on 2007-07-01. Retrieved 2007-08-07.
- Jabalameli, M; Jamshidi, K; Radi, M; Hadi, H; Bagherifard, A (2014). "Surgical outcomes of 26 patients with pigmented villonodular synovitis (PVNS) of the knee at a mean follow-up of 4 years: Introducing a novel technique". Medical Journal of the Islamic Republic of Iran. 28: 123. PMC 4313448. PMID 25679002.
- West, R. B.; Rubin, B. P.; Miller, M. A.; Subramanian, S.; Kaygusuz, G.; Montgomery, K.; Zhu, S.; Marinelli, R. J.; De Luca, A.; Downs-Kelly, E.; Goldblum, J. R.; Corless, C. L.; Brown, P. O.; Gilks, C. B.; Nielsen, T. O.; Huntsman, D.; Van De Rijn, M. (2006). "A landscape effect in tenosynovial giant-cell tumor from activation of CSF1 expression by a translocation in a minority of tumor cells". Proceedings of the National Academy of Sciences. 103 (3): 690–695. Bibcode:2006PNAS..103..690W. doi:10.1073/pnas.0507321103. PMC 1325107. PMID 16407111.
The CSF1 translocations result in overexpression of CSF1. In cases of TGCT and PVNS carrying this translocation, it is present in a minority of the intratumoral cells, leading to CSF1 expression only in these cells, whereas the majority of cells express CSF1R but not CSF1, suggesting a tumor-landscaping effect with aberrant CSF1 expression in the neoplastic cells, leading to the abnormal accumulation of nonneoplastic cells that form a tumorous mass.
- Cupp, John S.; Miller, Melinda A.; Montgomery, Kelli D.; Nielsen, Torsten O.; o??Connell, John X.; Huntsman, David; Rijn, Matt van de; Gilks, Cyril B.; West, Robert B. (2007). "Translocation and Expression of CSF1 in Pigmented Villonodular Synovitis, Tenosynovial Giant Cell Tumor, Rheumatoid Arthritis and Other Reactive Synovitides". The American Journal of Surgical Pathology. 31 (6): 970–976. doi:10.1097/PAS.0b013e31802b86f8. PMID 17527089. S2CID 29544370.
As the CSF1 translocation is postulated to play an important role in the biology of PVNS/TGCT, the consistent presence of CSF1 expression in translocation-negative cases implies that other mechanisms can lead to CSF1 up-regulation.
- Akinci, Orhan; Akalin, Y.; Incesu, M.; Eren, A. (2011). "Long-term results of surgical treatment of pigmented villonodular synovitis of the knee". Acta Orthopaedica et Traumatologica Turcica. 45 (3): 149–155. doi:10.3944/AOTT.2011.2442. PMID 21765227.
- Verspoor, Floortje G. M.; Zee, Aniek A. G.; Hannink, Gerjon; Van Der Geest, Ingrid C. M.; Veth, Rene P. H.; Schreuder, H. W. Bart (2014). "Long-term follow-up results of primary and recurrent pigmented villonodular synovitis". Rheumatology. 53 (11): 2063–2070. doi:10.1093/rheumatology/keu230. PMID 24917565.
- Frassica FJ, Bhimani MA, McCarthy EF, Wenz J (October 1999). "Pigmented villonodular synovitis of the hip and knee". Am Fam Physician. 60 (5): 1404–10, discussion 1415. PMID 10524485.
- Lei, Pengfei; Sun, Rongxin; Liu, Hao; Zhu, Jianxi; Wen, Ting; Hu, Yihe (2017). "Prognosis of Advanced Tenosynovial Giant Cell Tumor of the Knee Diagnosed During Total Knee Arthroplasty". The Journal of Arthroplasty. 32 (6): 1850–1855. doi:10.1016/j.arth.2016.12.053. PMID 28161138.
- Illian, Christian; Kortmann, Horst-Rainer; Künstler, Hans Otto; Poll, Ludger W.; Schofer, Markus (2009). "Tenosynovial giant cell tumors as accidental findings after episodes of distortion of the ankle: Two case reports". Journal of Medical Case Reports. 3: 9331. doi:10.1186/1752-1947-3-9331. PMC 2803852. PMID 20062758.
- Hegedus, Eric J.; Theresa, Kristen (2008). "Postoperative Management of Pigmented Villonodular Synovitis in a Single Subject". Journal of Orthopaedic & Sports Physical Therapy. 38 (12): 790–797. doi:10.2519/jospt.2008.2934. PMID 19047769.
- Krych, Aaron; Odland, Andrew; Rose, Peter; Dahm, Diane; Levy, Bruce; Wenger, Doris; Stuart, Michael; Sim, Franklin (2014). "Oncologic Conditions That Simulate Common Sports Injuries". Journal of the American Academy of Orthopaedic Surgeons. 22 (4): 223–234. doi:10.5435/JAAOS-22-04-223. PMID 24668352. S2CID 37108679.
- Adams, E. L.; Yoder, E. M.; Kasdan, M. L. (2012). "Giant cell tumor of the tendon sheath: Experience with 65 cases". ePlasty. 12: e50. PMC 3499005. PMID 23185646.
- Lee, Yoo Jin; Kang, Youngjin; Jung, Jiyoon; Kim, Seojin; Kim, Chul Hwan (2016). "Intramuscular Tenosynovial Giant Cell Tumor, Diffuse-Type". Journal of Pathology and Translational Medicine. 50 (4): 306–308. doi:10.4132/jptm.2015.11.15. PMC 4963964. PMID 26755356.
- Ottaviani, Sébastien; Ayral, Xavier; Dougados, Maxime; Gossec, Laure (2011). "Pigmented Villonodular Synovitis: A Retrospective Single-Center Study of 122 Cases and Review of the Literature". Seminars in Arthritis and Rheumatism. 40 (6): 539–546. doi:10.1016/j.semarthrit.2010.07.005. PMID 20884045.
- Van Der Heijden, L.; Gibbons, C. L. M. H.; Dijkstra, P. D. S.; Kroep, J. R.; Van Rijswijk, C. S. P.; Nout, R. A.; Bradley, K. M.; Athanasou, N. A.; Hogendoorn, P. C. W.; Van De Sande, M. A. J. (2012). "The management of diffuse-type giant cell tumour (Pigmented villonodular synovitis) and giant cell tumour of tendon sheath (Nodular tenosynovitis)". The Journal of Bone and Joint Surgery. British Volume. 94-B (7): 882–888. doi:10.1302/0301-620X.94B7.28927. PMID 22733940.
- Cannarile, Michael A.; Weisser, Martin; Jacob, Wolfgang; Jegg, Anna-Maria; Ries, Carola H.; Rüttinger, Dominik (2017). "Colony-stimulating factor 1 receptor (CSF1R) inhibitors in cancer therapy". Journal for Immunotherapy of Cancer. 5 (1): 53. doi:10.1186/s40425-017-0257-y. PMC 5514481. PMID 28716061.
The tumor-permissive and immunosuppressive characteristics of tumor-associated macrophages (TAM) have fueled interest in therapeutically targeting these cells. In this context, the colony-stimulating factor 1 (CSF1)/colony-stimulating factor 1 receptor (CSF1R) axis has gained the most attention, and various approaches targeting either the ligands or the receptor are currently in clinical development.