Squamous cell carcinoma
Squamous-cell carcinomas (SCCs), also known as epidermoid carcinomas, comprise a number of different types of cancer that begin in squamous cells.[1] These cells form on the surface of the skin, on the lining of hollow organs in the body, and on the lining of the respiratory and digestive tracts.[1]
Common types include:
- Squamous-cell skin cancer: A type of skin cancer
- Squamous-cell carcinoma of the lung: A type of lung cancer
- Squamous-cell thyroid carcinoma: A type of thyroid cancer
- Esophageal squamous-cell carcinoma: A type of esophageal cancer
- Squamous-cell carcinoma of the vagina: A type of vaginal cancer
Despite sharing the name "squamous-cell carcinoma", the SCCs of different body sites can show differences in their presented symptoms, natural history, prognosis, and response to treatment.
By body location
Human papillomavirus infection has been associated with SCCs of the oropharynx, lung,[2] fingers,[3] and anogenital region.
Head and neck cancer
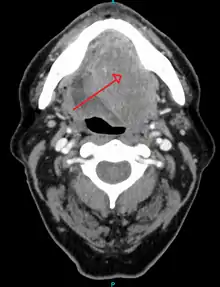
About 90%[4] of cases of head and neck cancer (cancer of the mouth, nasal cavity, nasopharynx, throat and associated structures) are due to SCC.
Skin
Squamous cell carcinoma of the skin is the second most common skin cancer, accounting for over 1 million cases in the United States each year.[5]
Thyroid
Primary squamous-cell thyroid carcinoma shows an aggressive biological phenotype resulting in poor prognosis for patients.[6]
Esophagus
Esophageal cancer may be due to either esophageal squamous cell carcinoma (ESCC) or adenocarcinoma (EAC). SCCs tend to occur closer to the mouth, while adenocarcinomas occur closer to the stomach. Dysphagia (difficulty swallowing, solids worse than liquids) and painful swallowing are common initial symptoms. If the disease is localized, surgical removal of the affected esophagus may offer the possibility of a cure. If the disease has spread, chemotherapy and radiotherapy are commonly used.[7]
Lung

When associated with the lung, it is typically a centrally located large-cell cancer (nonsmall-cell lung cancer). It often has a paraneoplastic syndrome causing ectopic production of parathyroid hormone-related protein, resulting in hypercalcemia, but paraneoplastic syndrome is more commonly associated with small-cell lung cancer. It is primarily due to smoking.[8]
Penis
Human papillomavirus (HPV), primarily HPV 16 and 18, are strongly implicated in the development of SCC of the penis. Three carcinomas in situ are associated with SCCs of the penis:
- Bowen's disease presents as leukoplakia on the shaft. Around a third of cases progress to SCC.
- Erythroplasia of Queyrat, a variation of Bowen's disease, presents as erythroplakia on the glans.
- Bowenoid papulosis, which histologically resembles Bowen disease, presents as reddish papules.[9]
Prostate
When associated with the prostate, squamous-cell carcinoma is very aggressive in nature. It is difficult to detect as no increase in prostate-specific antigen levels is seen, meaning that the cancer is often diagnosed at an advanced stage.
Vagina and cervix
Vaginal SCC spreads slowly and usually stays near the vagina, but may spread to the lungs and liver. This is the most common type of vaginal cancer.[10]
Bladder
Most bladder cancer is transitional cell, but bladder cancer associated with schistosomiasis is often SCC.
Diagnosis
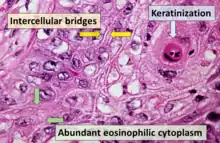
_squamous_cell_carcinoma_histopathology.jpg.webp)
Medical history, physical examination and medical imaging may suggest a squamous cell carcinoma, but a biopsy for histopathology generally establishes the diagnosis. TP63 staining is the main histological marker for Squamous cell carcinoma. In addition, TP63 is an essential transcription factor to establish squamous cell identity.[15]
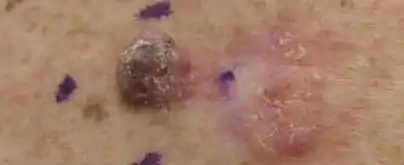 Squamous cell carcinoma, well differentiated, left upper paraspinal back marked for biopsy with adjacent actinic keratosis
Squamous cell carcinoma, well differentiated, left upper paraspinal back marked for biopsy with adjacent actinic keratosis Squamous cell carcinoma, left lateral canthus marked for biopsy
Squamous cell carcinoma, left lateral canthus marked for biopsy Squamous cell carcinoma, left ventral forearm
Squamous cell carcinoma, left ventral forearm
Classification
Cancer can be considered a very large and exceptionally heterogeneous family of malignant diseases, with squamous cell carcinomas comprising one of the largest subsets.[16][17][18] All SCC lesions are thought to begin via the repeated, uncontrolled division of cancer stem cells of epithelial lineage or characteristics. SCCs arise from squamous cells, which are flat cells that line many areas of the body. Some of which are keratinocytes. Accumulation of these cancer cells causes a microscopic focus of abnormal cells that are, at least initially, locally confined within the specific tissue in which the progenitor cell resided. This condition is called squamous cell carcinoma in situ, and it is diagnosed when the tumor has not yet penetrated the basement membrane or other delimiting structure to invade adjacent tissues. Once the lesion has grown and progressed to the point where it has breached, penetrated, and infiltrated adjacent structures, it is referred to as "invasive" squamous cell carcinoma. Once a carcinoma becomes invasive, it is able to spread to other organs and cause the formation of a metastasis, or "secondary tumor".
Tissue of origin
The International Classification of Diseases for Oncology (ICD-O) system lists a number of morphological subtypes and variants of malignant squamous cell neoplasms, including:[19]
- Papillary thyroid carcinoma (code 8050/3)
- Verrucous squamous cell carcinoma (code 8051/3)
- Papillary squamous cell carcinoma (code 8052/3)
- Squamous cell carcinoma (code 8070/3)
- Large-cell keratinizing squamous cell carcinoma (code 8071/3)
- Large-cell nonkeratinizing squamous cell carcinoma (code 8072/3)
- Small-cell keratinizing squamous cell carcinoma (code 8073/3)
- Spindle-cell squamous cell carcinoma (code 8074/3) It is also known as spindle-cell carcinoma,[20] and is a subtype characterized by spindle-shaped atypical cells.[21]
- Adenoid/pseudoglandular squamous cell carcinoma (code 8075/3)
- Intraepidermal squamous cell carcinoma (code 8081/3)
- Lymphoepithelial carcinoma (code 8082/3)
Other variants of SCCs are recognized under other systems, such as keratoacanthoma.
Other histopathologic subtypes
- Erythroplasia of Queyrat
- Marjolin's ulcer is a type of SCC that arises from a nonhealing ulcer or burn wound. More recent evidence, however, suggests that genetic differences exist between SCC and Marjolin's ulcer, which were previously underappreciated.[22]
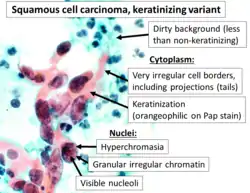
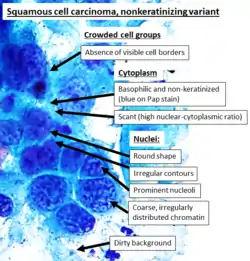
One method of classifying squamous cell carcinomas is by their appearance under microscope. Subtypes may include:
- Adenoid squamous cell carcinoma (also known as pseudoglandular squamous cell carcinoma) is characterized by a tubular microscopic pattern and keratinocyte acantholysis.[21]
- Basaloid squamous cell carcinoma is characterized by a predilection for the tongue base.[21]
- Clear-cell squamous cell carcinoma (also known as clear-cell carcinoma of the skin) is characterized by keratinocytes that appear clear as a result of hydropic swelling.[21]
- Signet ring-cell squamous cell carcinoma (occasionally rendered as signet ring-cell squamous cell carcinoma) is a histological variant characterized by concentric rings composed of keratin and large vacuoles corresponding to markedly dilated endoplasmic reticulum.[21] These vacuoles grow to such an extent that they radically displace the cell nucleus toward the cell membrane, giving the cell a distinctive superficial resemblance to a "signet ring" when viewed under a microscope.
 Adenoid squamous-cell carcinoma
Adenoid squamous-cell carcinoma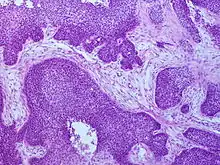 Basaloid squamous-cell carcinoma
Basaloid squamous-cell carcinoma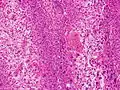 Clear-cell squamous-cell carcinoma
Clear-cell squamous-cell carcinoma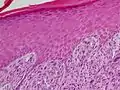 Spindle-cell squamous-cell carcinoma
Spindle-cell squamous-cell carcinoma
Prevention
Studies have found evidences for an association between diet and skin cancers, including SCC. The consumption of high-fat dairy foods increases SCC tumor risk in people with previous skin cancer. Green leafy vegetables may help prevent development of subsequent SCC and multiple studies found that raw vegetables and fruits are significantly protective against SCC risk.[23][24] On the other hand, consumption of whole milk, yogurt, and cheese may increase SCC risk in susceptible people.[25] In addition, meat and fat dietary pattern can increase the risk of SCC in people without a history of SCC, but the association is again more prominent in people with a history of skin cancer.[26] Tobacco smoking and a dietary pattern characterized by high beer and liquor intake also increase the risk of SCC significantly.[27][23]
References
- "NCI Dictionary of Cancer Terms". National Cancer Institute. 2011-02-02. Retrieved 9 November 2016.
- Yu Y, Yang A, Hu S, Yan H (June 2009). "Correlation of HPV-16/18 infection of human papillomavirus with lung squamous cell carcinomas in Western China". Oncology Reports. 21 (6): 1627–32. doi:10.3892/or_00000397. PMID 19424646.
- "Recurrent Squamous Cell Carcinoma In Situ of the Finger". Retrieved 2010-09-22.
- "Types of head and neck cancer - Understanding - Macmillan Cancer Support". Retrieved 15 March 2017.
- Howell, Jesse Y.; Ramsey, Michael L. (2022), "Squamous Cell Skin Cancer", StatPearls, Treasure Island (FL): StatPearls Publishing, PMID 28722968, retrieved 2022-03-09
- Syed MI, Stewart M, Syed S, Dahill S, Adams C, McLellan DR, Clark LJ (January 2011). "Squamous cell carcinoma of the thyroid gland: primary or secondary disease?". The Journal of Laryngology and Otology. 125 (1): 3–9. doi:10.1017/S0022215110002070. PMID 20950510. S2CID 28225556.
- "Esophageal Cancer". The Lecturio Medical Concept Library. 26 October 2020. Retrieved 6 August 2021.
- Pooler C, Hannon RA, Porth C, Matfin G (2010). Porth pathophysiology: concepts of altered health states (1st Canadian ed.). Philadelphia, PA: Wolters Kluwer Health/Lippincott Williams & Wilkins. p. 660. ISBN 978-1-60547-781-7.
- Robbins S, Kumar V, Abbas A, Fausto N (2007). Robbins Basic Pathology (8th ed.). Philadelphia: Saunders/Elsevier. p. 688. ISBN 978-1-4160-2973-1.
- "Squamous-cell Carcinoma of the Vagina". www.dynamed.com. Retrieved 2018-02-20.
- Dr Nicholas Turnbull, A/Prof Patrick Emanual (2014-05-03). "Squamous cell carcinoma pathology". DermNetz.
- - Image annotated by Mikael Häggström
- Reference for entries: Gulisa Turashvili, M.D., Ph.D. "Cervix - Squamous cell carcinoma and variants". Pathology Outlines.{{cite web}}: CS1 maint: multiple names: authors list (link) Last author update: 24 September 2020. Last staff update: 4 April 2022.
- Source image from National Cancer Institute (Public Domain) - - Image annotated by Mikael Häggström
- Reference for entries: Gulisa Turashvili, M.D., Ph.D. "Cervix - Squamous cell carcinoma and variants". Pathology Outlines.{{cite web}}: CS1 maint: multiple names: authors list (link) Last author update: 24 September 2020. Last staff update: 4 April 2022.
- Source image by Ravi Mehrotra, Anurag Gupta, Mamta Singh and Rahela Ibrahim (Creative Commons Attribution 2.0 Generic license.) - Authors: Caroline I.M. Underwood, M.D., Alexis Musick, B.S., Carolyn Glass, M.D., Ph.D. "Adenocarcinoma overview". Pathology Outlines.
{{cite web}}: CS1 maint: multiple names: authors list (link) Last staff update: 19 July 2022 - Prieto-Garcia C, Hartmann O, Reissland M, Braun F, Fischer T, Walz S, et al. (April 2020). "Maintaining protein stability of ∆Np63 via USP28 is required by squamous cancer cells". EMBO Molecular Medicine. 12 (4): e11101. doi:10.15252/emmm.201911101. PMC 7136964. PMID 32128997.
- Berman JJ (November 2004). "Tumor taxonomy for the developmental lineage classification of neoplasms". BMC Cancer. 4 (1): 88. doi:10.1186/1471-2407-4-88. PMC 535937. PMID 15571625.
- Berman JJ (March 2004). "Tumor classification: molecular analysis meets Aristotle". BMC Cancer. 4 (1): 10. doi:10.1186/1471-2407-4-10. PMC 415552. PMID 15113444.
- Travis WD, Brambilla E, Muller-Hermelink HK, Harris CC, eds. (2004). Pathology and Genetics of Tumours of the Lung, Pleura, Thymus and Heart (PDF). World Health Organization Classification of Tumours. Lyon: IARC Press. ISBN 978-92-832-2418-1. Archived from the original (PDF) on 23 August 2009. Retrieved 27 March 2010.
- Van Holten, Valerie; World Health Organization (1990). Muir, C.S.; Percy, C.L.; Van Holten, V. (eds.). International Classification of Diseases for Oncology: ICD-0 (2nd ed.). Geneva, Switzerland: World Health Organization. ISBN 9789241544146.
- Rapini RP, Bolognia JL, Jorizzo JL (2007). Dermatology: 2-Volume Set. St. Louis: Mosby. ISBN 978-1-4160-2999-1.
- Fitzpatrick TB, Freedberg IM, eds. (2003). Fitzpatrick's dermatology in general medicine (6th ed.). New York, NY: McGraw-Hill. p. 743. ISBN 978-0-07-138076-8.
- Sinha S, Su S, Workentine M, Agabalyan N, Cheng M, Gabriel V, Biernaskie J (January 2017). "Transcriptional Analysis Reveals Evidence of Chronically Impeded ECM Turnover and Epithelium-to-Mesenchyme Transition in Scar Tissue Giving Rise to Marjolin's Ulcer". Journal of Burn Care & Research. 38 (1): e14–e22. doi:10.1097/BCR.0000000000000432. PMID 27679957. S2CID 3702018.
- De Stefani E, Deneo-Pellegrini H, Ronco AL, Boffetta P, Brennan P, Muñoz N, Castellsagué X, Correa P, Mendilaharsu M (October 2003). "Food groups and risk of squamous cell carcinoma of the oesophagus: a case-control study in Uruguay". British Journal of Cancer. 89 (7): 1209–14. doi:10.1038/sj.bjc.6601239. PMC 2394307. PMID 14520448.
- Chen YK, Lee CH, Wu IC, Liu JS, Wu DC, Lee JM, Goan YG, Chou SH, Huang CT, Lee CY, Hung HC, Yang JF, Wu MT (July 2009). "Food intake and the occurrence of squamous cell carcinoma in different sections of the esophagus in Taiwanese men". Nutrition. 25 (7–8): 753–61. doi:10.1016/j.nut.2009.02.002. PMID 19394796.
- Hughes MC, van der Pols JC, Marks GC, Green AC (October 2006). "Food intake and risk of squamous cell carcinoma of the skin in a community: the Nambour skin cancer cohort study". International Journal of Cancer. 119 (8): 1953–60. doi:10.1002/ijc.22061. PMID 16721782.
- Ibiebele TI, van der Pols JC, Hughes MC, Marks GC, Williams GM, Green AC (May 2007). "Dietary pattern in association with squamous cell carcinoma of the skin: a prospective study". The American Journal of Clinical Nutrition. 85 (5): 1401–8. doi:10.1093/ajcn/85.5.1401. PMID 17490979.
- Bahmanyar S, Ye W (2006). "Dietary patterns and risk of squamous-cell carcinoma and adenocarcinoma of the esophagus and adenocarcinoma of the gastric cardia: a population-based case-control study in Sweden". Nutrition and Cancer. 54 (2): 171–8. doi:10.1207/s15327914nc5402_3. PMID 16898861. S2CID 1959103.