Involuntary treatment
Involuntary treatment (also referred to by proponents as assisted treatment and by critics as forced drugging) refers to medical treatment undertaken without the consent of the person being treated. Involuntary treatment is permitted by law in some countries when overseen by the judiciary through court orders; other countries defer directly to the medical opinions of doctors.
| Part of series on |
| Involuntary treatment |
|---|
| Restraint |
| Involuntary commitment |
|
| Regulated by |
|
| Alternatives |
| Treatment |
|
Some countries have general legislation allowing for any treatment deemed necessary if an individual is unable to consent to a treatment due to lack of capacity,[1][2] other legislation may specifically deal with involuntary psychiatric treatment of individuals who have been diagnosed with a mental disorder.[3] Psychiatric treatment normally happens in a psychiatric hospital after some form of involuntary commitment, though individuals may be compelled to undergo treatment outside of hospitals via outpatient commitment.[4]
The diagnosis of mental disorders can be carried out by some form clinical practitioner, or in some cases law enforcement or others, to be a danger to themselves or to others is permitted in some jurisdictions, while other jurisdictions have more recently allowed for forced treatment for persons deemed to be "gravely disabled" or asserted to be at risk of psychological deterioration.
A patient may be detained because they are diagnosed with a psychiatric disorder[5] or infectious disease.[6]
History

In the early 20th century, many countries passed laws allowing the compulsory sterilization of some women. In the USA more than half the states passed laws allowing the forced sterilization of people with certain illnesses or criminals as well as sterilization based on race.[7] Forcible sterilization took place in the United States until at least 1981,[8] more than 64 thousand people were forcibly sterilized.[9] Denmark sterilized 60 thousand people between 1935 and 1976.[10] During Nazi rule in Germany as part of their eugenics program about 600 thousand people were compulsorily sterilized.[11]
Involuntary euthanasia was carried out in Nazi Germany for those who had certain psychiatric disorders or learning disabilities as part of the Aktion T4 program.[12] This program was run by Karl Brandt, a medical doctor, and Philipp Bouhler.[13]: 185 Victims were murdered together in gas chambers and this program was a prototype for the extermination camps such as Auschwitz where the Holocaust took place.[14] As part of Action 14f13, physicians involved in the euthanasia program visited concentration camps where they looked at documentation provided by SS camp doctors and approved the murder of camp inmates on the grounds of race, behavior and ability to work using the euthanasia program's facilities.[13]: 192
In the UK the 1950s, homosexual men were given the choice between hormone therapy with female sex hormones or prison including, notably, Alan Turing.[15]
Until 2004, every European state required that transgender people must be sterilized or provably infertile to have their preferred gender formally recognised.[16]: 7 This practice continued in Sweden until 2012[17] and Denmark until 2014[18] Japan currently requires transgender people to be sterilized and have their ovaries removed to be recognised as a different gender.[19]
Ethics and the law
The Hippocratic Corpus, an ancient Greek text discussing medical ethics, advises that physicians conceal most information from patients to give the patients the best care.[20]: 61 The 1767 English case Slater vs Baker and Stapleton found against two doctors who had refractured a patient's leg without consent.[21]: 116 Thomas Percival was a British physician who published a book called Medical Ethics in 1803, which makes no mention of soliciting for the consent of patients or respecting their decisions.[22]: 68 Percival said that patients have a right to truth, but when the physician could provide better treatment by lying or withholding information, he advised that the physician do as he thought best.[22]: 68 Benjamin Rush an 18th-century United States physician, in a lecture entitled "On the duties of patients to their physicians", stated that patients should be strictly obedient to the physician's orders; this was representative of much of his writings.[23]: 65
The US Canterbury v. Spence case established the principle of informed consent in US law. Earlier legal cases had created the underpinnings for informed consent, but his judgment gave a detailed and thought through discourse on the matter.[24] The judgment cites cases going back to 1914 as precedent for informed consent.[25]: 56
Infectious disease
In response to the bubonic plague some city states restricted movement of people into them using cordon sanitaires, and separated those were suspected of being infected into makeshift camps.[26]: 254 Merchant sailors were made to isolate in lazarettos, hospitals for infectious diseases.[26]: 255 England created quarantine regulations in 1663 to confine ships suspected of being infected with the plague.[26]: 255 In response to cholera outbreaks in the 1830s, some European cities people with symptoms were forced into lazarettos.[26]: 256 An 1853 law in the United Kingdom made vaccination compulsory with those refusing to comply receiving fines.[27] People with symptoms of tuberculosis have been detained in New York from 1902.[28]: 237 During the spanish flu pandemic western cities implemented social distancing and closed schools, churches, theatres and restricted public gatherings.[26]: 257 During the COVID-19 pandemic many countries implemented lockdowns restricting movement, enforcing working from home[29] and social distancing.
Mental health
In 1789 during the French Revolution, the French government issued a directive for the management of the insane. This directive ordered that the insane be incarcerated and treated.[30]: 84 Bethlem Royal Hospital is a mental hospital in the United Kingdom, which started exclusively treating mental illness in 1377. In 1818, Urban Metcalf, a patient at Bethlam, published a book describing his experience there. He described physical restraint of patients manacled to walls. This followed a report by the government in 1815 describing conditions in asylums in the UK.[30]: 85
Political use
Psychiatric diagnoses have been used for political purposes.[31]: 65 Psychiatry can be used to bypass standard legal procedures and political incarceration. The use of hospitals instead of jails prevents those detainend from receiving legal aid, makes indefinite incarceration possible, discredits the individuals and their ideas.[32]: 29 During the Nazi era and the Soviet rule religious and political dissenters were labeled as "mentally ill" and subjected to inhumane "treatments".[33][34] From the 1960s to 1986, abuse of psychiatry for political and ideological purposes was reported to be systematic in the Soviet Union, and occasional in Eastern European countries such as Romania, Hungary, Czechoslovakia and Yugoslavia.[35][36]: 66
Legislative distinctions
Legislation may allow for involuntary of a particular disease or class of diseases such as mental disorders.[37]: 263 Some countries have legislation to involuntarily detain or examine those suspected to have tuberculosis, or treat them if infected.[6]: 610 Those treated for mental health disorders are commited before involuntary treatment. Those under community treatment orders may be ordered to take medication, and if they fail to maybe be committed and treated involuntarily.[38]: 16
In some countries, involuntary treatment for mental health is not used to treat a symptom that is present but to reduce the risk of symptoms returning through the use prophylactic psychotropic medication. This is achieved through the use of outpatient commitment where a patient may be detained in hospital if they fail to take the medication doctors have prescribed them.[38]: 16
Some countries have general legislation allowing for any treatment deemed necessary if an individual is unable to consent to a treatment due to lack of capacity.[1][2]: 108
Forms

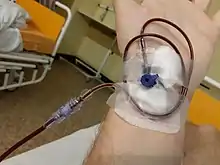
Chemical restraint, such as forcible injection with the antipsychotic haloperidol or benzodiazepine sedative midazolam, may be used to sedate a patient who is agitated.[39]: 624 [40]: 152 In some countries, antipsychotics and sedatives can be forcibly administered to those who are committed, using intramuscular depot injection.[41] Those with anorexia nervosa may receive force-feeding.[42][43]
Those with infectious diseases such as tuberculosis can be detained and isolated.[4]
Japan requires transgender people to undergo sterilization to have their gender formally recognized.[44][45] In the Czech Republic, men convicted of sex offenses are in practice given the choice of long-term detention or castration.[46]: 346 Brazil,[47] Bulgaria,[48] Costa Rica,[49] Croatia,[48] Czechia,[48] France,[48] Hungary,[49] Indonesia,[50] Italy,[48] Poland,[48] and Russia[51] make certain vaccinations mandatory.
Coercion in voluntary mental health treatment
.JPG.webp)
Individuals may be forced to undergo mental health treatment legally-speaking "voluntarily" under the threat of involuntary treatment.[38]: 98 Many individuals who legally would be viewed as receiving mental health treatment voluntarily believe that they have no choice in the matter.[lower-alpha 1] Studies show that 51%, 35% and 29% of mental health patients have experienced some form of informal coercion in the US, England and Switzerland respectively.[38]: 100
Once voluntarily within a mental health hospital, rules, process, and information-asymmetry (a healthcare providers know more how the hospital functions than a patient) can be used to achieve compliance from a person in voluntary treatment. To prevent someone from leaving voluntarily, staff may use stalling tactics made possible by the fact that all doors are locked. For example, the person may be referred to a member of staff who is rarely on the ward, or made to wait until after lunch or a meeting, behaving as if a person in voluntary treatment does not have the right to leave without permission. When the person is able to talk about leaving, the staff may use vague language to imply that the person is required to stay, relying on the fact that people in voluntary treatment do not understand their legal status.[lower-alpha 2]
Szmukler and Appelbaum constructed a hierarchy of types of coercion in mental health care, ranging from persuasion to interpersonal leverage, inducements, threats and compulsory treatment. Here persuasion refers to argument through reason. Forms of coercion that do not use legal compulsion are referred to as informal coercion or leverage.[38]: 98 Interpersonal leverage may arise from the desire to please health workers with whom a relationship has formed. Threats may revolve around a health worker helping or hindering the receipt of government benefits.[54]
Non-voluntary treatment
In certain limited circumstance a patient may have capacity but be unable to consent to treatment at a time when a decision is necessary, in such cases surgery may be performed on a patient without consent.[55]: 1 A patient may issue an advance healthcare directive specifying how they would like to be treated if they are unable to consent to treatment. In the UK, a healthcare worker does not need to follow an advanced directive but they will influence decisions.[55]: 5 Alternatively, a surrogate decision-maker such as a relative, friend or healthcare professional may make decisions on a patients behalf if a patient is unable to.[56]: 810
Competent adults
The faith of Jehovah's Witnesses forbids blood transfusion. Courts in the United States have consistently upheld the right of competent adults to decline blood transfusion even when it would be life-saving, though there have been exceptions where the death of a patient could leave a child orphaned.[57]: 255
In the United States, courts have ordered pregnant women to involuntarily undergo caesarean section, intrauterine transfusion, and enforced bed rest.[58]: 188 There are cases of clinicians threatening pregnant patients with removal of child custody or withdrawal of care if they decline treatment.[58]: 192 In the UK, courts are unable to force treatment on pregnant women who are deemed to have capacity, however as of 2016 there were no cases of still pregnant woman being deemed to have capacity by a court.[59]: 40
Children

Parents or medical doctors may make decision about the treatment of children, a principle known as parens patriae.[60]: 5 In the United States, doctors are responsible for providing a good standard of care for patients who are children which can lead them to make decisions at odds with the parents wishes. Parents have less autonomy to make decisions about their children's care than adult patients have over their own care.[60]: 5 Treatment may take place even if a child or adolescent disagree with treatment, though the wishes of child patient are taken more into account the more burdensome treatment is and the worse the prognosis.[60]: 8
If a child does not assent to treatment they may be physically held while a procedure or anaesthesia is carried out.[61]: 162 For some procedures a child may be distracted to allow for treatment.[61]: 159
In Italy, court orders have been used to give children of Jehovah's Witnesses life-saving blood transfusion that were refused by their parents.[62]: 102
Prevalence
There is a lot of variation in the rate of involuntary commitment between countries. A review in Europe in 2004 found a thirty-fold difference in the rate of psychiatric commitment between countries, with the median rate being 74 per hundred thousand people. It is estimated that 38% of people who are involuntarily committed experience another form of compulsion such as seclusion or forced medication.[63]: 2
Effects
A 2014 Cochrane systematic review found that compulsory outpatient treatment of those with severe mental health disorders "results in no significant difference in service use, social functioning or quality of life compared with standard voluntary care."[64] A 2006 review found that as many as 48% of respondents did not agree with their treatment, though a majority of people retrospectively agreed that involuntary medication had been in their best interest.[65]
A review in 2011 looked at people's experience of coercion in mental health care. It found common themes of feeling violated, disrespected, and not being heard, commonly conceptualized as being dehumanized through isolation. A minority of narratives from people who had been treated involuntarily talked about the necessity of treatment in retrospect.[lower-alpha 3] Studies suggest that coercion in mental health care has a long-lasting psychological effect on individuals leading to reduced engagement and poorer social outcomes, but that this may be reduced by clinicians' knowledge of the effects of coercion.[38] A systematic review and meta synthesis from 2020, that combined the experiences of stakeholders (service-users, informal carers such as family members, and mental health professionals), identified experiences of power imbalances among the stakeholders. The review found that these power imbalances hindered the respect for the service users' rights, will, and preferences.[67]
Ethics
In medical ethics, involuntary treatment is conceptualized as a form of parens patriae whereby the state takes on the responsibilities of incompetent adults on the basis of the duty to protect and the duty of beneficence (the duty of the state to repair the random harms of nature). The duty to protect is reflected in utilitarianism and communitarianism philosophy, though psychiatrist Paul Chodoff asserted a responsibility to "chasten" this responsibility in light of the political abuse of psychiatry in the Soviet Union.[68]: 82 This duty to protect has been criticized on the grounds that psychiatrists are not effective at predicting violence, and tend to overestimate the risk.[68]: 89
The obligatory dangerousness criterion is a principle that has been applied to some mental health law that holds that parens patriae should only be applied if an individual is a danger to themselves or others.[69]
Paul Ricœur distinguishes two forms of self, the idem, a short term experience of the self, and the ipse, a longer term persistent experience of the self. In mental illness, the autonomy of the ipse can be undermined by the autonomy of the idem, so involuntary mental health treatment can trade one form of autonomy for another.[68]: 90
Sociology
Medical sociology seeks to understand the social processes underlying decisions made in medicine.
Sociologist Jeremy Dixon, speaking in the context of the United Kingdom, argues that assessment and monitoring of risk is a core part of mental health practice[70]: 126 but that this risk is often in conflict with broadly-defined goals of recovery including living a satisfying life.[70]: 129 He argues that this focus on risk causes mental health professionals to make decisions defensively based on reputational damage if there were to be any inquiry and that multidisciplinary approaches are used for this purpose.[70]: 134 He cites research showing how mental health professionals may seek to shift the burden of responsibility onto individuals themselves (noting different clinical decisions for those with personality disorders compared to those with psychotic disorders because they are viewed as more responsible for their behaviours), or shift responsibility onto other public health services.[70]: 134 Risk assessments themselves are rarely shared with patients.[70]: 135
Proponents and detractors
Proponents
Supporters of involuntary treatment include organizations such as the National Alliance on Mental Illness (NAMI), the American Psychiatric Association, and the Treatment Advocacy Center.[71]
Detractors
A number of civil and human rights activists, Anti-psychiatry groups, medical and academic organizations, researchers, and members of the psychiatric survivors movement vigorously oppose involuntary treatment on human rights grounds or on grounds of effectiveness and medical appropriateness, particularly with respect to involuntary administration of mind altering substances, ECT, and psychosurgery. Some criticism has been made regarding cost, as well as of conflicts of interest with the pharmaceutical industry. Critics, such as the New York Civil Liberties Union, have denounced the strong racial and socioeconomic biases in forced treatment orders.[72]
Special rapporteurs of the United Nations (Catalina Devandas Aguilar and Dainius Puras[73]) consider it as an infringement of the dignity of those subjected to it, with severe consequences for their physical and mental integrity and call on concerned states to put an end to respect individual's autonomy.

Involuntary treatment is compared to torture[8][73] on at least two special reports of the UN, one noting "forced psychiatric interventions, when committed against persons with psychosocial disabilities, satisfies both intent and purpose required under the article 1 of the Convention against Torture, notwithstanding claims of “good intentions” by medical professionals.". However, jurisdiction of some countries (e.g. France) requires intended harm (see : punitive psychiatry) to classify it as such and would classify involuntary treatment, rather as a degrading treatment, if recognize as it.
Amnesty international,[14] Human Rights Watch[9] opposes involuntary treatment.
Laws internationally
United States
Mentally competent patients have a general right to refuse medical treatment.[74][75][76]
All states in the U.S. allow for some form of involuntary treatment for mental illness or erratic behavior for short periods of time under emergency conditions, although criteria vary. Further involuntary treatment outside clear and pressing emergencies where there is asserted to be a threat to public safety usually requires a court order, and all states currently have some process in place to allow this. Since the late 1990s, a growing number of states have adopted Assisted Outpatient Commitment (AOC) laws.[77]
Under assisted outpatient commitment, people committed involuntarily can live outside the psychiatric hospital, sometimes under strict conditions including reporting to mandatory psychiatric appointments, taking psychiatric drugs in the presence of a nursing team, and testing medication blood levels. Forty-five states presently allow for outpatient commitment.[78]
In 1975, the U.S. Supreme Court ruled in O'Connor v. Donaldson that involuntary hospitalization and/or treatment violates an individual's civil rights. The individual must be exhibiting behavior that is a danger to themselves or others and a court order must be received for more than a short (e.g. 72-hour) detention. The treatment must take place in the least restrictive setting possible. This ruling has since been watered down through jurisprudence in some respects and strengthened in other respects. Long term "warehousing", through de-institutionalization, declined in the following years, though the number of people receiving involuntary treatment has increased more recently. The statutes vary somewhat from state to state.
In 1979, the United States Court of Appeals for the First Circuit established in Rogers v. Okin that a competent person committed to a psychiatric hospital has the right to refuse treatment in non-emergency situations. The case of Rennie v. Klein established that an involuntarily committed individual has a constitutional right to refuse psychotropic medication without a court order. Rogers v. Okin established the person's right to make treatment decisions so long as they are still presumed competent.
Additional U.S. Supreme Court decisions have added more restraints, and some expansions or effective sanctioning, to involuntary commitment and treatment. Foucha v. Louisiana established the unconstitutionality of the continued commitment of an insanity acquittee who was not suffering from a mental illness. In Jackson v. Indiana the court ruled that a person adjudicated incompetent could not be indefinitely committed. In Perry v. Louisiana the court struck down the forcible medication of a prisoner for the purposes of rendering him competent to be executed. In Riggins v. Nevada the court ruled that a defendant had the right to refuse psychiatric medication while he was on trial, given to mitigate his psychiatric symptoms. Sell v. United States imposed stringent limits on the right of a lower court to order the forcible administration of antipsychotic medication to a criminal defendant who had been determined to be incompetent to stand trial for the sole purpose of making them competent and able to be tried. In Washington v. Harper the Supreme Court upheld the involuntary medication of correctional facility inmates only under certain conditions as determined by established policy and procedures.[79]
Europe
| Country | During involuntary commitment | During outpatient commitment (community treatment order) |
|---|---|---|
| France [80] | Yes | Yes |
| UK [81] | Yes | Yes (after being recalled to hospital) |
| Germany [82] | Yes | Yes |
| Switzerland[83] | No in Geneva, not specified or yes for other cantons | |
| Italy [84][85] | Yes | Yes (7 days renewable) |
| Austria [86] | (no neuroleptic depot injection) | (no neuroleptic depot injection) |
| The Netherlands [87] | Yes (law passed recently) | Yes (at home) |
| Ireland | no outpatient commitment |
See also
Related concepts
- Coerced abstinence
- Political abuse of psychiatry (also known as "political psychiatry" and as "punitive psychiatry")
- Social control
- Specific jurisdictions' provisions for a temporary detention order for the purpose of mental-health evaluation and possible further voluntary or involuntary commitment:
- United States of America:
- California: 5150 (involuntary psychiatric hold) and Laura's Law (providing for court-ordered outpatient treatment)
- Lanterman–Petris–Short Act, codifying the conditions for and of involuntary commitment in California
- Florida: Baker Act and Marchman Act
Notable activists
- Giorgio Antonucci (elimination)
- Thomas Szasz (elimination)
- Robert Whitaker (reduction)
- E. Fuller Torrey (expansion)
- DJ Jaffe (expansion)
Advocacy organizations
- Mental Health America (reduction/modification)
- Mad in America (reduction/elimination)
- PsychRights (reduction/elimination)
- Anti-psychiatry, also known as the "anti-psychiatric movement" (reduction/elimination)
- Citizens Commission on Human Rights (reduction/elimination; founded as a joint effort of the anti-psychiatric Church of Scientology and libertarian mental-health-rights advocate Thomas Szasz)
- MindFreedom International (reduction/elimination)
- Treatment Advocacy Center (expansion)
- Mental Illness Policy (expansion)
- NAMI (expansion)
Notes
- "A significant proportion of voluntarily admitted service userscan experience the same level of perceived coercion as that experienced by involuntarily admitted service users. It needs to be ensured that if any service user, whether voluntary or involuntary, experiences treatment pressures or coercion, that there is sufficient oversight of the practice to ensure that individual's rights are respected."[52]
- See section 6.1 entitled "stalling" in.[53] From this section: "[T]he patient's mistaken belief that she cannot leave the hospital facilitates the staff's efforts to stall her. Most importantly, uncertainties regarding formal status make it possible for clinicians to phrase persuasive statements in strategic ways. At times, they might use words that connote coercion where coercion is not formally used. At other times, they might use words of cooperation when formal coercion is in fact applied. Similarly, particular symptoms of the patient, such as a temporary inability to concentrate, might serve as a resource for the staff in managing information in order to accomplish compliance."
- See table 1 of:[66] "The aspects of care leading to the experience of coercion were broad, but all involved the forcing of "treatment" onto patients against their will. The themes from these articles highlight feelings of violation, disrespect, and not being heard by their clinicians. The most common conceptualization was that of being dehumanized through a loss of normal human interaction and isolation. Using a wide range of thematic analyses, we found that these themes emerged in each article for a range of treatment interventions; this finding was robust. Positive themes were mentioned in three of the five articles from a minority of patients. These tended to emerge in retrospect, well after a patient's hospitalization, and focused on the need or rationale for treatment. These positive themes tended to reflect the social norms and explanations for compulsory care's leading to coercion, rather than the emotive or subjective responses elicited by such care."
References
- Davidson G, Brophy L, Campbell J, Farrell SJ, Gooding P, O'Brien AM (1 January 2016). "An international comparison of legal frameworks for supported and substitute decision-making in mental health services". International Journal of Law and Psychiatry. 44: 30–40. doi:10.1016/j.ijlp.2015.08.029. hdl:10379/11074. PMID 26318975. S2CID 6564501.
- Kim SY (2010). Evaluation of Capacity to Consent to Treatment and Research. Oxford University Press, USA. ISBN 978-0-19-532295-8.
- "Mental capacity and mental illness". Mental capacity and mental illness. Retrieved 19 December 2021.
- Schlossberg, David L. (20 June 2017). Tuberculosis and Nontuberculous Mycobacterial Infections. John Wiley & Sons. ISBN 978-1-55581-985-9.
- Sheridan Rains, Luke; Zenina, Tatiana; Dias, Marisa Casanova; Jones, Rebecca; Jeffreys, Stephen; Branthonne-Foster, Stella; Lloyd-Evans, Brynmor; Johnson, Sonia (2019). "Variations in patterns of involuntary hospitalisation and in legal frameworks: an international comparative study". The Lancet Psychiatry. 6 (5): 403–417. doi:10.1016/S2215-0366(19)30090-2. PMC 6475657. PMID 30954479.
- Coker, Richard; Thomas, Marianna; Lock, Karen; Martin, Robyn (2007). "Detention and the Evolving Threat of Tuberculosis: Evidence, Ethics, and Law". Journal of Law, Medicine & Ethics. 35 (4): 609–615. doi:10.1111/j.1748-720X.2007.00184.x. ISSN 1073-1105. PMID 18076512. S2CID 19924571.
- Patel P (14 July 2017). "Forced sterilization of women as discrimination". Public Health Reviews. 38 (1): 15. doi:10.1186/s40985-017-0060-9. PMC 5809857. PMID 29450087.
- Sullivan J (15 November 2002). "State will admit sterilization past". Portland Oregonian. Archived from the original on 7 January 2016.
- Lombardo P. "Eugenic Sterilization Laws". Eugenics Archive.
- Olsen J (29 August 1997). "Denmark to investigate its involuntary sterilization program". AP News.
- "The connection between American eugenics and Nazi Germany, James Watson :: DNA Learning Center". Archived from the original on 21 February 2014. Retrieved 5 February 2014. |"The connection between American eugenics and Nazi Germany" James Watson speaks about Nazi eugenics
- Strous RD (January 2006). "Nazi euthanasia of the mentally ill at Hadamar". The American Journal of Psychiatry. 163 (1): 27. doi:10.1176/appi.ajp.163.1.27. PMID 16390885.
- Browning CR (2004). The origins of the Final Solution : the evolution of Nazi Jewish policy, September 1939-March 1942. Jürgen Matthäus. Lincoln: University of Nebraska Press. ISBN 0-8032-0392-6. OCLC 54860099.
- Young R. The "Euthanasia" of People with Disabilities in Nazi Germany: Harbinger of the "Final Solution" (Report).
- Smith G, Bartlett A, King M (February 2004). "Treatments of homosexuality in Britain since the 1950s--an oral history: the experience of patients". BMJ. 328 (7437): 427. doi:10.1136/bmj.328.427.37984.442419.EE. PMC 344257. PMID 14751920.
- Dunne P (November 2017). "Transgender Sterilisation Requirements in Europe". Medical Law Review. 25 (4): 554–581. doi:10.1093/medlaw/fwx028. PMID 28575446.
- Nelson R (14 January 2013). "Transgender People in Sweden No Longer Face Forced Sterilization". Time. ISSN 0040-781X. Retrieved 7 April 2021.
- "OVERBLIK: Transkønnedes kamp mod lovgivningen". avisen.dk (in Danish). 22 May 2018. Archived from the original on 9 August 2018. Retrieved 9 August 2018.
- "Japan says transgender people must be sterilised". The Economist. 14 March 2019. ISSN 0013-0613. Retrieved 18 March 2022.
- Faden, Ruth R.; Beauchamp, Tom L.; King, Nancy M.P. (1986). A history and theory of informed consent (Online ed.). New York: Oxford University Press. ISBN 978-0-19-5036862.
- Faden, Ruth R. (1986). A history and theory of informed consent. Tom L. Beauchamp, Nancy M. P. King. New York: Oxford University Press. ISBN 1-4237-6352-1. OCLC 228168485.
- Faden, Ruth R.; Beauchamp, Tom L.; King, Nancy M.P. (1986). A history and theory of informed consent (Online ed.). New York: Oxford University Press. ISBN 978-0-19-5036862.
- Faden, Ruth R.; Beauchamp, Tom L.; King, Nancy M.P. (1986). A history and theory of informed consent (Online ed.). New York: Oxford University Press. ISBN 978-0-19-5036862.
- "Chapter 1: Canterbury vs Spence". Health law and bioethics : cases in context. Sandra H. Johnson. New York: Aspen Publishers/Wolters Kluwer. 2009. ISBN 978-0-7355-7767-1. OCLC 294067618.
{{cite book}}: CS1 maint: others (link) - Faden, Ruth R. (1986). A history and theory of informed consent. Tom L. Beauchamp, Nancy M. P. King. New York: Oxford University Press. ISBN 1-4237-6352-1. OCLC 228168485.
- Tognotti, Eugenia (2013). "Lessons from the History of Quarantine, from Plague to Influenza A". Emerging Infectious Diseases. 19 (2): 254–259. doi:10.3201/eid1902.120312. ISSN 1080-6040. PMC 3559034. PMID 23343512.
- El Amin AN, Parra MT, Kim-Farley R, Fielding JE (June 2012). "Ethical Issues Concerning Vaccination Requirements". Public Health Reviews. 34 (1): 1–20. doi:10.1007/BF03391666. ISSN 2107-6952. S2CID 155224076.
- Lerner, Barron H. (1 January 1999). "Catching Patients: Tuberculosis and Detention in the 1990s". Chest. 115 (1): 236–241. doi:10.1378/chest.115.1.236. ISSN 0012-3692. PMID 9925090.
- Pang, Zhihong; Becerik-Gerber, Burçin; Hoque, Simi; O’Neill, Zheng; Pedrielli, Giulia; Wen, Jin; Wu, Teresa (26 October 2021). "How Work From Home Has Affected the Occupant's Well-Being in the Residential Built Environment: An International Survey Amid the Covid-19 Pandemic". ASME Journal of Engineering for Sustainable Buildings and Cities. 2 (4). doi:10.1115/1.4052640. ISSN 2642-6641. S2CID 244247777.
- Pietikäinen, Petteri (2015). Madness : a history. London. ISBN 978-0-415-71316-0. OCLC 898113408.
- British Medical Association (1992). Medicine betrayed: the participation of doctors in human rights abuses. Zed Books. p. 65. ISBN 978-1-85649-104-4.
- Veenhoven, Willem; Ewing, Winifred; Samenlevingen, Stichting (1975). Case studies on human rights and fundamental freedoms: a world survey. Martinus Nijhoff Publishers. p. 29. ISBN 978-90-247-1780-4.
- Protecting and Promoting Religious Rights in Eastern Europe and the Soviet Union: Hearing Before the Committee on Foreign Relations, United States Senate, Ninety-eighth Congress, Second Session, June 12, 1984. United States Congress Senate Committee on Foreign Relations. 1984. p. 30.
- Shah, Ruchita; Basu, Debasish (July–September 2010). "Coercion in psychiatric care: Global and Indian perspective". Indian Journal of Psychiatry. 52 (3): 203–206. doi:10.4103/0019-5545.70971. PMC 2990818. PMID 21180403.
- Stan, Lavinia (2013). Transitional Justice in Post-Communist Romania: The Politics of Memory. Cambridge University Press. ISBN 978-1-107-02053-5.
- British Medical Association (1992). Medicine betrayed: the participation of doctors in human rights abuses. Zed Books. p. 65. ISBN 978-1-85649-104-4.
- Cronin, T.; Gouda, P.; McDonald, C.; Hallahan, B. (2017). "A comparison of mental health legislation in five developed countries: a narrative review". Irish Journal of Psychological Medicine. 34 (4): 261–269. doi:10.1017/ipm.2017.48. ISSN 0790-9667. PMID 30115178. S2CID 52021078.
- Molodynski A, Rugkåsa J, Burns T (2016). Coercion in Community Mental Health Care: International Perspectives. Oxford University Press. p. 289. ISBN 978-0-19-878806-5.
- Cameron P, Little M, Mitra B, Deasy C (23 May 2019). Textbook of Adult Emergency Medicine E-Book. Elsevier Health Sciences. ISBN 978-0-7020-7625-1.
- McKnight R, Geddes J (15 May 2019). Psychiatry. Oxford University Press. ISBN 978-0-19-875400-8.
- Smith JP, Herber OR (June 2015). "Ethical issues experienced by mental health nurses in the administration of antipsychotic depot and long-acting intramuscular injections: a qualitative study". International Journal of Mental Health Nursing. 24 (3): 222–230. doi:10.1111/inm.12105. PMID 25394562.
- Túry F, Szalai T, Szumska I (August 2019). "Compulsory treatment in eating disorders: Control, provocation, and the coercion paradox". Journal of Clinical Psychology. 75 (8): 1444–1454. doi:10.1002/jclp.22783. PMID 31004507.
- "Report to the Czech Governmenton the visit to the Czech Republic carried out by the European Committee for the Prevention of Torture and Inhuman or Degrading Treatment or Punishment". p. 15.
- "Japan: New Momentum to Reform Transgender Law". Human Rights Watch. 25 May 2021. Retrieved 4 January 2022.
- "Japan: Compelled Sterilization of Transgender People". Human Rights Watch. 19 March 2019. Retrieved 4 January 2022.
- Lišková K, Bělehradová A (July 2019). "'We Won't Ban Castrating Pervs Despite What Europe Might Think!': Czech Medical Sexology and the Practice of Therapeutic Castration". Medical History. 63 (3): 330–351. doi:10.1017/mdh.2019.30. PMC 7329228. PMID 31208483.
- "Vacinação: quais são as vacinas, para quê servem, por que vacinar, mitos". www.saude.gov.br (in Brazilian Portuguese). Archived from the original on 8 October 2019. Retrieved 8 October 2019.
- "Vaccine Scheduler | ECDC". vaccine-schedule.ecdc.europa.eu. Archived from the original on 2 September 2019. Retrieved 8 October 2019.
- "Factbox: Countries making COVID-19 vaccines mandatory". Reuters. 15 November 2021. Archived from the original on 18 November 2021. Retrieved 18 November 2021.
- "Peraturan Menteri Kesehatan Republik Indonesia Nomor 12 Tahun 2017 Tentang Penyelanggaraan Imunisasi" (PDF) (in Indonesian). Kemenkes. 6 February 2017. Archived (PDF) from the original on 27 November 2019. Retrieved 4 December 2019.
- Grigoryan A (9 May 2019). "Russia: Government Expanding Vaccination for Measles Amid Outbreak in Neighboring Countries | Global Legal Monitor". www.loc.gov. Archived from the original on 20 February 2020. Retrieved 6 November 2019.
- O'Donoghue B, Roche E, Shannon S, Lyne J, Madigan K, Feeney L (January 2014). "Perceived coercion in voluntary hospital admission". Psychiatry Research. 215 (1): 120–126. doi:10.1016/j.psychres.2013.10.016. PMID 24210740. S2CID 42451989.
- Sjöström S (January 2006). "Invocation of coercion context in compliance communication -- power dynamics in psychiatric care". International Journal of Law and Psychiatry. 29 (1): 36–47. doi:10.1016/j.ijlp.2005.06.001. PMID 16309742.
- Szmukler G, Appelbaum PS (January 2008). "Treatment pressures, leverage, coercion, and compulsion in mental health care". Journal of Mental Health. 17 (3): 233–244. doi:10.1080/09638230802052203. S2CID 144254330.
- Jerjes W, Mahil J, Upile T (September 2011). "English law for the surgeon I: consent, capacity and competence". Head & Neck Oncology. 3 (1): 41. doi:10.1186/1758-3284-3-41. PMC 3184094. PMID 21923926.
- Shah SG, Farrow A, Robinson I (December 2009). "The representation of healthcare end users' perspectives by surrogates in healthcare decisions: a literature review". Scandinavian Journal of Caring Sciences. 23 (4): 809–819. doi:10.1111/j.1471-6712.2008.00674.x. PMID 19740114.
- McCormick TR (September 2008). "Ethical Issues Inherent to Jehovah's Witnesses". Perioperative Nursing Clinics. 3 (3): 253–258. doi:10.1016/j.cpen.2008.04.007.
- DeBruin D, Faith Marshall M (2021). "Coercive Interventions in Pregnancy: Law and Ethics". Journal of Health Care Law and Policy.
- Halliday S (5 May 2016). Autonomy and Pregnancy (0 ed.). Routledge. doi:10.4324/9781843147206. ISBN 978-1-135-32993-8.
- Katz AL, Webb SA (August 2016). "Informed Consent in Decision-Making in Pediatric Practice". Pediatrics. 138 (2): e20161485. doi:10.1542/peds.2016-1485. PMID 27456510. S2CID 7951515.
- Bray L, Snodin J, Carter B (June 2015). "Holding and restraining children for clinical procedures within an acute care setting: an ethical consideration of the evidence" (PDF). Nursing Inquiry. 22 (2): 157–167. doi:10.1111/nin.12074. PMID 25053126.
- Conti A, Capasso E, Casella C, Fedeli P, Salzano FA, Policino F, et al. (5 April 2018). "Blood Transfusion in Children: The Refusal of Jehovah's Witness Parents'". Open Medicine. 13 (1): 101–104. doi:10.1515/med-2018-0016. PMC 5900417. PMID 29666843.
- Sashidharan SP, Mezzina R, Puras D (December 2019). "Reducing coercion in mental healthcare". Epidemiology and Psychiatric Sciences. 28 (6): 605–612. doi:10.1017/S2045796019000350. PMC 7032511. PMID 31284895.
- Kisely SR, Campbell LA, O'Reilly R (March 2017). "Compulsory community and involuntary outpatient treatment for people with severe mental disorders". The Cochrane Database of Systematic Reviews. 3 (6): CD004408. doi:10.1002/14651858.CD004408.pub5. PMC 6464695. PMID 28303578.
- Katsakou C, Priebe S (October 2006). "Outcomes of involuntary hospital admission--a review". Acta Psychiatrica Scandinavica. 114 (4): 232–241. doi:10.1111/j.1600-0447.2006.00823.x. PMID 16968360. S2CID 20677644.
- Newton-Howes G, Mullen R (May 2011). "Coercion in psychiatric care: systematic review of correlates and themes". Psychiatric Services. 62 (5): 465–470. doi:10.1176/ps.62.5.pss6205_0465. PMID 21532070.
- Sugiura K, Pertega E, Holmberg C (24 November 2020). "Experiences of involuntary psychiatric admission decision-making: a systematic review and meta-synthesis of the perspectives of service users, informal carers, and professionals". International Journal of Law and Psychiatry. 73: 101645. doi:10.1016/j.ijlp.2020.101645. PMID 33246221. S2CID 227190332.
- Robertson M, Walter G (26 September 2013). Ethics and Mental Health: The Patient, Profession and Community. CRC Press. ISBN 978-1-4441-6865-5.
- Appelbaum PS (1997). "Almost a revolution: an international perspective on the law of involuntary commitment". The Journal of the American Academy of Psychiatry and the Law. 25 (2): 135–147. PMID 9213286.
- Chamberlain JM (19 November 2015). Medicine, Risk, Discourse and Power. Routledge. ISBN 978-1-317-33196-4.
- Shdaimah C, O'Reilly N. "Understanding US debates surrounding standards in involuntary inpatient psychiatric commitment through the Maryland experience". Social Work in Mental Health.
- "Implementation of Kendra's Law is Severely Biased" (PDF). New York Lawyers for the Public Interest, Inc. 7 April 2005. Archived from the original (PDF) on 28 June 2007.
- Recommandations de bonnes pratiques de la Haute Autorité de Santé de février 2017 : Isolement et contention en psychiatrie générale
- "The right to refuse treatment: a model act". American Journal of Public Health. 73 (8): 918–921. August 1983. doi:10.2105/AJPH.73.8.918. PMC 1651109. PMID 6869647.
- Kanaboshi N (1 July 2006). "Competent Persons' Constitutional Right to Refuse Medical Treatment in the U.S. and Japan: Application to Japanese Law". Penn State International Law Review. 25 (1): 5.
- "Cruzan v. Director, Missouri Department of Health, (88-1503), 497 U.S. 261 (1990)". www.law.cornell.edu.
- Perlin ML (2003). "Therapeutic jurisprudence and outpatient commitment law: Kendra's Law and case study". Psychology, Public Policy, and Law. 9 (1–2): 183–208. doi:10.1037/1076-8971.9.1-2.183. PMID 16700141.
- "Browse by State".
- "Washington et al., Petitioners v. Walter Harper". Retrieved 10 October 2007.
- "Article L3213-1". Code de la santé publique. Republic of France.
- "Consent to treatment". Mind.
- Taube F (21 January 2013). "Bundestag passes bill on involuntary treatment". Deutsche Welle.
- Morandi S, Burns T (18 December 2013). "Involuntary outpatient treatment for mental health problems in Switzerland: A literature review". International Journal of Social Psychiatry. 60 (7): 695–702. doi:10.1177/0020764013513439. ISSN 0020-7640. PMID 24351963. S2CID 43580285.
- "Legge 13 maggio 1978, n. 180 "Accertamenti e trattamenti sanitari volontari e obbligatori"" (PDF). Government of Italy.
- "Scheda pratica - Trattamento sanitario obbligatorio: ricorso contro provvedimento del sindaco". Ministero della giustizia.
- Salize HJ, Dressing H, Peitz M (15 May 2002). "Compulsory Admission and Involuntary Treatment of Mentally Ill Patients – Legislation and Practice in EU-Member States" (PDF). European Union.
- de Waardt DA, van der Heijden FM, Rugkåsa J, Mulder CL (February 2020). "Compulsory treatment in patients' homes in the Netherlands: what do mental health professionals think of this?". BMC Psychiatry. 20 (1): 80. doi:10.1186/s12888-020-02501-7. PMC 7041256. PMID 32093641.