Splenic injury
A splenic injury, which includes a ruptured spleen, is any injury to the spleen. The rupture of a normal spleen can be caused by trauma, such as a traffic collision.
| Splenic injury | |
|---|---|
 | |
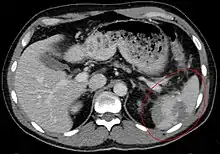
| Spleen ruptured by trauma | |
| Specialty | Emergency medicine |
Signs and symptoms
In minor injuries with little bleeding, there may be abdominal pain, tenderness in the epigastrium and pain in the left flank. Often there is a sharp pain in the left shoulder, known as Kehr's sign. In larger injuries with more extensive bleeding, signs of hypovolemic shock are most prominent. This might include a rapid pulse, low blood pressure, rapid breathing, paleness, and anxiety.
Causes
The most common cause of a ruptured spleen is blunt abdominal trauma, such as in traffic collisions or sports accidents. Direct, penetrating injuries, for example, stab or gunshot wounds are rare.
Non-traumatic causes are less common. These include infectious diseases, medical procedures such as colonoscopy, haematological diseases, medications, and pregnancy.[1]
In less than one percent of cases of infectious mononucleosis splenic rupture may occur.[2]
Diagnosis
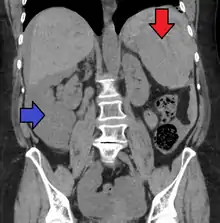
Splenic rupture is usually evaluated by FAST ultrasound of the abdomen.[3] Generally this is not specific to splenic injury; however, it is useful to determine the presence of free floating blood in the peritoneum.[3] A diagnostic peritoneal lavage, while not ideal, may be used to evaluate the presence of internal bleeding a person who is hemodynamically unstable.[4] The FAST exam typically serves to evaluate the need to perform a CT scan.[4] Computed tomography with IV contrast is the preferred imaging study as it can provide high quality images of the full peritoneal cavity.[3]
Organ injury scale
American Association for the Surgery of Trauma Organ Injury Scaling: Splenic Injury Grading[5]
| Grade | Subcapsular hematoma | Laceration |
|---|---|---|
| I | <10% surface area | <1 cm parenchymal depth |
| II | 10–50% surface area | 1–3 cm parenchymal depth |
| III | >50% surface area or expanding | >3-cm parenchymal depth |
| IV | Major devascularization (>25% of spleen) | |
| V | Completely shattered spleen |
Treatment
Because a splenic rupture permits large amounts of blood to leak into the abdominal cavity, it can result in shock and death. Generally a nonoperative approach is chosen in those who are hemodynamically stable with non-worsening symptoms.[5][6] During this period of nonoperative management strict bed rest between 24 and 72 hours with careful monitoring along with a CT 7 days after the injury.[5]
If an individual's spleen is enlarged, as is frequent in mononucleosis, most physicians will advise against activities (such as contact sports) where injury to the abdomen could be catastrophic.[7]
Patients whose spleens have been removed via a splenectomy must receive immunizations to help prevent infections such as pneumonia. This helps to replace the lost function of this organ.
See also
References
- Aubrey-Bassler, F.; Sowers, N. (2012). "613 cases of splenic rupture without risk factors or previously diagnosed disease: A systematic review". BMC Emergency Medicine. 12: 11. doi:10.1186/1471-227X-12-11. PMC 3532171. PMID 22889306.

- Handin, Robert I.; Lux, Samuel E.; Stossel, Thomas P. (2003). Blood: Principles and Practice of Hematology. Lippincott Williams & Wilkins. p. 641. ISBN 9780781719933.
- Mattox 2012, p. 566
- Trunkey 2008, p. 401
- Uranues, Prof Selman; Kilic, Yusuf A. (2008-07-30). "Injuries to the Spleen". European Journal of Trauma and Emergency Surgery. 34 (4): 355–361. doi:10.1007/s00068-008-8102-0. ISSN 1863-9933. PMID 26815812. S2CID 8808584.
- Mattox 2012, p. 570
- "About Mono (Infectious Mononucleosis) | CDC". www.cdc.gov. 2021-03-17. Retrieved 2022-07-17.
Bibliography
- Feliciano, David V.; Mattox, Kenneth L.; Moore, Ernest J. (2012). Trauma, Seventh Edition (Trauma (Moore)). McGraw-Hill Professional. ISBN 978-0-07-166351-9.
- Trunkey, Donald (2008). Current Therapy of Trauma and Surgical Critical Care (1st ed.). Philadelphia: Mosby. ISBN 978-0-323-04418-9.