Sprain
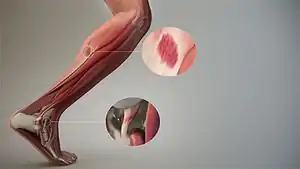
A sprain, also known as a torn ligament, is an acute soft tissue injury of the ligaments within a joint, often caused by a sudden movement abruptly forcing the joint to exceed its functional range of motion. Ligaments are tough, inelastic fibers made of collagen that connect two or more bones to form a joint and are important for joint stability and proprioception, which is the body's sense of limb position and movement.[1] Sprains can occur at any joint but most commonly occur in the ankle, knee, or wrist.[2] An equivalent injury to a muscle or tendon is known as a strain.
| Sprain | |
|---|---|
| Other names | Torn ligament, distorsio |
 | |
| A sprained ankle with bruising and swelling | |
| Specialty | Sports medicine, physical medicine & rehabilitation, orthopedics, family medicine, emergency medicine |
| Symptoms | Pain, swelling, bruising, joint instability, limited range of motion of the injured joint |
| Duration | Mild cases - few days to six weeks Severe cases - few weeks to months |
| Causes | Trauma, sports injuries, overuse, environmental hazards |
| Risk factors | Environmental factors, age, poor training or sports gear |
| Diagnostic method | Physical exam, joint x-ray |
| Differential diagnosis | Strain, fracture |
| Prevention | Frequent stretching and conditioning, bracing at risk joints during exercise |
| Treatment | Rest, ice, compression, elevation, NSAIDs |
| Medication | Non-steroidal anti-inflammatory drugs (NSAIDs) |
| Prognosis | Mild injuries resolve well on their own. Severe injuries likely require surgery and physical therapy. |
The majority of sprains are mild, causing minor swelling and bruising that can be resolved with conservative treatment, typically summarized as RICE: rest, ice, compression, elevation. However, severe sprains involve complete tears, ruptures, or fractures, often leading to joint instability, severe pain, and decreased functional ability. These sprains require surgical fixation, prolonged immobilization, and physical therapy.[3]
Signs and symptoms
- Pain
- Swelling
- Bruising or hematoma caused by broken blood vessels within the injured ligament
- Joint instability[4]
- Difficulty with bearing weight
- Decreased functional ability or range of motion of the injured joint[5]
- Ligament rupture may cause a cracking or popping sound at the time of injury[6]
Knowing the signs and symptoms of a sprain can be helpful in differentiating the injury from a strain or fracture. Strains typically present with pain, cramping, muscle spasm, and muscle weakness, and fractures typically present with bone tenderness, especially when bearing weight.[7]
Causes
Acute sprains typically occur when the joint is abruptly forced beyond its functional range of motion, often in the setting of trauma or sports injuries. Chronic sprains are caused by repetitive movements leading to overuse.
Mechanism
Ligaments are collagen fibers that connect bones together, providing passive stabilization to a joint. These fibers can be found in various organizational patterns (parallel, oblique, spiral, etc.) depending on the function of the joint involved. Ligaments can be extra-capsular (located outside the joint capsule), capsular (continuation of the joint capsule), or intra-articular (located within a joint capsule).[1] The location has important implications for healing as blood flow to intra-articular ligaments is diminished compared to extra-capsular or capsular ligaments.[8]
Collagen fibers have about a 4% elastic zone where fibers stretch out with increased load on the joint. However, exceeding this elastic limit causes a rupture of fibers, leading to a sprain. It is important to recognize that ligaments adapt to training by increasing the cross-sectional area of fibers.[9] When a ligament is immobilized, the ligament has been shown to rapidly weaken. Normal daily activity is important for maintaining about 80–90% of the mechanical properties of a ligament.[1]
Risk factors
- Fatigue and overuse[1]
- High-intensity contact sports
- Environmental factors
- Poor conditioning or equipment[6]
- Age and genetic predisposition to ligament injuries[10]
- Lack of stretching or "warming up", which when performed properly increases blood flow and joint flexibility[11]
.jpg.webp)
Diagnosis
Sprains can often be diagnosed clinically based on the patient's signs and symptoms, mechanism of injury, and physical examination. However, x-rays can be obtained to help identify fractures, especially in cases of tenderness or bone pain at the injured site.[12] In some instances, particularly if the healing process is prolonged or a more serious injury is suspected, magnetic resonance imaging (MRI) is performed to look at the surrounding soft tissue and ligaments.[13]
Classification
- First degree sprain (mild) – There is minor stretching and structural damage to the ligament, leading to mild swelling and bruising. Patients typically present without joint instability or decreased range of motion of the joint.
- Second degree sprain (moderate) – There is a partial tear of the affected ligament. Patients typically experience moderate swelling, tenderness, and some instability of the joint. There may be some difficulty bearing weight on the affected joint.[14]
- Third degree sprain (severe) – There is a complete rupture or tear of the ligament, sometimes avulsing a piece of bone. Patients typically experience severe joint instability, pain, bruising, swelling, and inability to apply weight to the joint.[15]
Joints involved
Although any joint can experience a sprain, some of the more common injuries include the following:[3]
- Ankle - Sprains most commonly occur at the ankle and can take longer to heal than ankle bone fractures. Most sprained ankles usually occur in the lateral ligaments on the outside of the ankle. Common causes include walking on uneven surfaces or during contact sports.[16] See sprained ankle or high ankle sprain for more details.
- Inversion Ankle Sprain - injury that occurs when ankle rolls inward
- Eversion Ankle Sprain - injury that occurs when ankle rolls outward
- Toes
- Knee - Sprains commonly occur at the knee, especially following intense pivoting on a planted leg during contact sports (American football, football, basketball, pole vaulting, softball, baseball and some styles of martial arts).[18]
- Anterior cruciate ligament (ACL) injury
- Posterior cruciate ligament (PCL) injury
- Medial collateral ligament (MCL) injury
- Lateral collateral ligament (LCL) injury
- Superior Tibiofibular Joint Sprain - typically caused by a twisting injury to the joint connecting the tibia (shinbone) and fibula
- Patellar dislocation
- Fingers and wrists - Wrist sprains commonly occur, especially during a fall on an outstretched hand.
- Gamekeeper's thumb (Skier's thumb) - forceful grabbing that leads to an injury to the ulnar collateral ligament (UCL) at the metacarpophalangeal (MCP) joint of the thumb, historically found in Scottish gamekeepers[19]
- Spine
- Neck sprain at the cervical vertebrae
- Whiplash (Traumatic Cervical Spine Syndrome) - forced hyperextension and flexion of the neck, classically found in rear-end auto accidents[20]
- Back sprain - Back sprains are one of the most common medical complaints, often caused by poor lifting mechanics and weak core muscles.
Treatment
Treatment of sprains usually involves incorporating conservative measures to reduce the signs and symptoms of sprains, surgery to repair severe tears or ruptures, and rehabilitation to restore function to the injured joint. Although most sprains can be managed without surgery, severe injuries may require tendon grafting or ligament repair based on the individual's circumstances.[21] The amount of rehabilitation and time needed for recovery will depend on the severity of the sprain.[22]
Treating Sprains
Depending on the mechanism of injury, joint involvement, and severity, most sprains can be treated using conservative measures following the acronym RICE within the first 24 hours of sustaining an injury.[23] However, it is important to recognize that treatments should be individualized depending on the patient's particular injury and symptoms.[24] Over-the-counter medications such as non-steroidal anti-inflammatory drugs (NSAIDs) can help relieve pain, and topical NSAIDs can be as effective as medications taken by mouth.[25]
- Protect: The injured site should be protected and immobilized, as there is an increased risk of recurrent injury to the affected ligaments.[26]
- Rest: The joint affected should be immobilized and bearing weight should be minimized. For example, walking should be limited in cases of sprained ankles.[27]
- Ice: Ice should be applied immediately to the sprain to reduce swelling and pain.[28] Ice can be applied 3–4 times a day for 10–15 minutes at a time or until the swelling subsides and can be combined with a wrapping for support.[27] Ice can also be used to numb pain but should only be applied for a short period of time (less than twenty minutes) for this purpose.[29] Prolonged ice exposure can reduce blood flow to the injured area and slow the healing process.[30]
- Compression: Dressings, bandages, or wraps should be used to immobilize the sprain and provide support. When wrapping the injury, more pressure should be applied to the distal end of the injury and decrease in the direction of the heart. This helps circulate the blood from the extremities to the heart. Careful management of swelling through cold compression therapy is critical to the healing process by preventing further pooling of fluid in the sprained area. However, compression should not impede circulation of the limb.[27]
- Elevation: Keeping the sprained joint elevated (in relation to the rest of the body) can minimize swelling.[27]
Other non-operative therapies including the continuous passive motion machine (moves joint without patient exertion) and cryocuff (type of cold compress that is activated similarly to a blood pressure cuff) have been effective in reducing swelling and improving range of motion.[31] Recent studies has shown that traction is just as effective as the RICE technique in treating ankle sprains in pediatric patients.[32]
Functional rehabilitation
The components of an effective rehabilitation program for all sprain injuries include increasing the range of motion of the affected joint and progressive muscle strengthening exercises.[33] After implementing conservative measures to reduce swelling and pain, mobilizing the limb within 48–72 hours following injury has been shown to promote healing by stimulating growth factors in musculoskeletal tissues linked to cellular division and matrix remodeling.[22]
Prolonged immobilization can delay the healing of a sprain, as it usually leads to muscle atrophy and weakness.[34] Although prolonged immobilization can have a negative effect on recovery, a study in 1996 suggest that the use of bracing can improve healing by alleviating pain and stabilizing the injury to prevent further damage to the ligament or re-injury.[35] When using a brace, it is necessary to ensure adequate blood flow to the extremity.[36] Ultimately, the goal of functional rehabilitation is to return the patient to full daily activities while minimizing the risk of re-injury.
References
- Bahr, Roald; Alfredson, Håkan; Järvinen, Markku; Järvinen, Tero; Khan, Karim; Kjaer, Michael; Matheson, Gordon; Maehlum, Sverre (2012-06-22), Bahr, Roald (ed.), "Types and Causes of Injuries", The IOC Manual of Sports Injuries, Wiley-Blackwell, pp. 1–24, doi:10.1002/9781118467947.ch1, ISBN 978-1-118-46794-7
- Hartshorne, Henry. "Sprained Joints". The Home Cyclopedia Of Health And Medicine. Retrieved 16 February 2010.
- "Ligament Sprain". Physiopedia. Retrieved 2020-04-13.
- Nancy Garrick, Deputy Director (2017-04-10). "Sprains and Strains". National Institute of Arthritis and Musculoskeletal and Skin Diseases. Retrieved 2020-04-14.
- "Sprains and Strains". medlineplus.gov. Retrieved 2020-04-14.
- "Sprains - Symptoms and causes". Mayo Clinic. Retrieved 2020-04-14.
- "Strains and Sprains Signs, Symptoms, Diagnosis and Treatment Information on MedicineNet.com". MedicineNet. Retrieved 2020-04-20.
- Frank, C. B. (June 2004). "Ligament structure, physiology and function". Journal of Musculoskeletal & Neuronal Interactions. 4 (2): 199–201. ISSN 1108-7161. PMID 15615126.
- Doschak, M. R.; Zernicke, R. F. (March 2005). "Structure, function and adaptation of bone-tendon and bone-ligament complexes". Journal of Musculoskeletal & Neuronal Interactions. 5 (1): 35–40. ISSN 1108-7161. PMID 15788869.
- Longo, Umile Giuseppe; Loppini, Mattia; Margiotti, Katia; Salvatore, Giuseppe; Berton, Alessandra; Khan, Wasim S.; Denaro, Nicola Maffulli and Vincenzo (2014-12-31). "Unravelling the Genetic Susceptibility to Develop Ligament and Tendon Injuries". Current Stem Cell Research & Therapy. 10 (1): 56–63. doi:10.2174/1574888x09666140710112535. PMID 25012736. Retrieved 2020-04-20.
- Woods, Krista; Bishop, Phillip; Jones, Eric (2007-12-01). "Warm-Up and Stretching in the Prevention of Muscular Injury". Sports Medicine. 37 (12): 1089–1099. doi:10.2165/00007256-200737120-00006. ISSN 1179-2035. PMID 18027995. S2CID 27159577.
- Vuurberg, Gwendolyn; Hoorntje, Alexander; Wink, Lauren M.; Doelen, Brent F. W. van der; Bekerom, Michel P. van den; Dekker, Rienk; Dijk, C. Niek van; Krips, Rover; Loogman, Masja C. M.; Ridderikhof, Milan L.; Smithuis, Frank F. (2018-08-01). "Diagnosis, treatment and prevention of ankle sprains: update of an evidence-based clinical guideline". British Journal of Sports Medicine. 52 (15): 956. doi:10.1136/bjsports-2017-098106. ISSN 0306-3674. PMID 29514819.
- Strains and sprains information Mayo Clinic. Retrieved on 2010-01-26
- Publishing, Harvard Health (17 May 2019). "Sprain (Overview)". Harvard Health. Retrieved 2020-04-20.
- "Sprains, Strains and Other Soft-Tissue Injuries - OrthoInfo - AAOS". www.orthoinfo.org. Retrieved 2020-04-14.
- Shier D, Butler J, Lewis R (2007). Hole's Human Anatomy & Physiology (11th ed.). McGraw Hill / Irwin. pp. 157, 160. ISBN 978-0-07-330555-4.
- "Turf Toe - OrthoInfo - AAOS". www.orthoinfo.org. Retrieved 2020-04-24.
- Publishing, Harvard Health (5 April 2019). "Knee Sprain". Harvard Health. Retrieved 2020-04-20.
- Hung, Chen-Yu; Varacallo, Matthew; Chang, Ke-Vin (2020), "Gamekeepers Thumb (Skiers, Ulnar Collateral Ligament Tear)", StatPearls, StatPearls Publishing, PMID 29763146, retrieved 2020-04-24
- Tanaka, Nobuhiro; Atesok, Kivanc; Nakanishi, Kazuyoshi; Kamei, Naosuke; Nakamae, Toshio; Kotaka, Shinji; Adachi, Nobuo (2018-02-28). "Pathology and Treatment of Traumatic Cervical Spine Syndrome: Whiplash Injury". Advances in Orthopedics. 2018: 4765050. doi:10.1155/2018/4765050. ISSN 2090-3464. PMC 5851023. PMID 29682354.
- Petersen, Wolf; Rembitzki, Ingo Volker; Koppenburg, Andreas Gösele; Ellermann, Andre; Liebau, Christian; Brüggemann, Gerd Peter; Best, Raymond (August 2013). "Treatment of acute ankle ligament injuries: a systematic review". Archives of Orthopaedic and Trauma Surgery. 133 (8): 1129–1141. doi:10.1007/s00402-013-1742-5. ISSN 0936-8051. PMC 3718986. PMID 23712708.
- Publishing, Harvard Health (8 February 2007). "Recovering from an ankle sprain". Harvard Health. Retrieved 2020-04-21.
- MedicalMnemonics.com: 235
- van den Bekerom, Michel P.J; Struijs, Peter A.A; Blankevoort, Leendert; Welling, Lieke; van Dijk, C. Niek; Kerkhoffs, Gino M.M.J (August 2012). "What Is the Evidence for Rest, Ice, Compression, and Elevation Therapy in the Treatment of Ankle Sprains in Adults?". Journal of Athletic Training. 47 (4): 435–443. doi:10.4085/1062-6050-47.4.14. ISSN 1062-6050. PMC 3396304. PMID 22889660.
- Derry S, Moore RA, Gaskell H, McIntyre M, Wiffen PJ (June 2015). "Topical NSAIDs for acute musculoskeletal pain in adults". The Cochrane Database of Systematic Reviews. 6 (6): CD007402. doi:10.1002/14651858.CD007402.pub3. PMC 6426435. PMID 26068955.
- Bleakley CM, O'Connor SR, Tully MA, Rocke LG, Macauley DC, Bradbury I, Keegan S, McDonough SM (10 May 2010). "Effect of accelerated rehabilitation on function after ankle sprain: randomised controlled trial". BMJ. 340: c1964. doi:10.1136/bmj.c1964. PMID 20457737.
- "Sprained Ankle". American Academy of Orthopaedic Surgeons. March 2005. Retrieved 2008-04-01.
- Hubbard, Tricia J.; Denegar, Craig R. (2004). "Does Cryotherapy Improve Outcomes With Soft Tissue Injury?". Journal of Athletic Training. 39 (3): 278–279. ISSN 1062-6050. PMC 522152. PMID 15496998.
- Cramer H, Ostermann T, Dobos G (February 2018). "Injuries and other adverse events associated with yoga practice: A systematic review of epidemiological studies". Journal of Science and Medicine in Sport. 21 (2): 147–154. doi:10.1016/j.jsams.2017.08.026. PMID 28958637.
- Singh, Daniel P.; Barani Lonbani, Zohreh; Woodruff, Maria A.; Parker, Tony J.; Steck, Roland; Peake, Jonathan M. (2017-03-07). "Effects of Topical Icing on Inflammation, Angiogenesis, Revascularization, and Myofiber Regeneration in Skeletal Muscle Following Contusion Injury". Frontiers in Physiology. 8: 93. doi:10.3389/fphys.2017.00093. ISSN 1664-042X. PMC 5339266. PMID 28326040.
- Liao, Chun-De; Tsauo, Jau-Yih; Huang, Shih-Wei; Chen, Hung-Chou; Chiu, Yen-Shuo; Liou, Tsan-Hon (April 2019). "Preoperative range of motion and applications of continuous passive motion predict outcomes after knee arthroplasty in patients with arthritis". Knee Surgery, Sports Traumatology, Arthroscopy. 27 (4): 1259–1269. doi:10.1007/s00167-018-5257-z. ISSN 1433-7347. PMID 30523369. S2CID 54446697.
- Iammarino, Kathryn; Marrie, James; Selhorst, Mitchell; Lowes, Linda P. (February 2018). "Efficacy of the Stretch Band Ankle Traction Technique in the Treatment of Pediatric Patients with Acute Ankle Sprains: A Randomized Control Trial". International Journal of Sports Physical Therapy. 13 (1): 1–11. doi:10.26603/ijspt20180001. ISSN 2159-2896. PMC 5808004. PMID 29484236.
- Keene, David J; Williams, Mark A; Segar, Anand H; Byrne, Christopher; Lamb, Sarah E (2016-02-25). "Immobilisation versus early ankle movement for treating acute lateral ankle ligament injuries in adults". Cochrane Database of Systematic Reviews. doi:10.1002/14651858.cd012101. ISSN 1465-1858.
- Mattacola, Carl G.; Dwyer, Maureen K. (2002). "Rehabilitation of the Ankle After Acute Sprain or Chronic Instability". Journal of Athletic Training. 37 (4): 413–429. ISSN 1062-6050. PMC 164373. PMID 12937563.
- familydoctor.org editorial staff (2010-12-01) [Created:1996-01-01]. "Ankle Sprains: Healing and Preventing Injury". American Academy of Family Physicians.
- Hsu H, Siwiec RM (2019), "Forearm Splinting", StatPearls, StatPearls Publishing, PMID 29763155, retrieved 2019-03-12
External links
- Questions and Answers about Sprains and Strains - US National Institute of Arthritis and Musculoskeletal and Skin Diseases