Triple-A syndrome
Triple-A syndrome or AAA syndrome is a rare autosomal recessive congenital disorder. In most cases, there is no family history of AAA syndrome.[2] The syndrome was first identified by Jeremy Allgrove and colleagues in 1978, since then just over 100 cases have been reported.[3] The syndrome, is called triple aaa due to the manifestation of the illness which include achalasia (a dysfunction of the esophagus), addisonianism (adrenal insufficiency of primary type), and alacrima (insufficiency of tears). Alacrima is usually the earliest manifestation.[4] Neurodegeneration or atrophy of the nerve cells and autonomic dysfunction may be seen in the disorder, therefore some have suggested the disorder be called 4A syndrome.[5] It is a progressive disorder that can take years to develop the full-blown clinical picture.[6] The disorder also has variability and heterogeneity in presentation.[7]
| Triple A syndrome | |
|---|---|
| Other names | Achalasia–addisonianism–alacrima syndrome or Allgrove syndrome[1] |
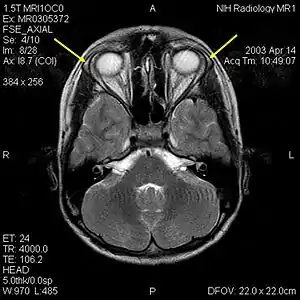 | |
| MRI of the brain of 12-year-old boy with triple-A syndrome showing hypoplastic lacrimal glands (yellow arrows) | |
| Specialty | Endocrinology |
Presentation
Individuals affected by AAA have adrenal insufficiency/Addison's disease due to ACTH resistance, alacrima (absence of tear secretion), and achalasia (a failure of a ring of muscle fibers in the lower part of the esophagus to relax) called the lower esophageal sphincter at the cardia (very upper portion of the stomach) The esophagus is the tube that carries food from the mouth to the stomach. Achalasia delays food going to the stomach and causes dilation of the thoracic esophagus. There may also be signs of autonomic dysfunction with AAA, such as pupillary abnormalities, an abnormal reaction to intradermal histamine, abnormal sweating, orthostatic hypotension (low blood pressure with standing), and disturbances of the heart rate.[8] Unexplained Hypoglycemia (low blood sugar) is often mentioned as an early sign.[6] The disorder has also been associated with mild mental retardation.[6] The syndrome is highly variable. However, one of the most common findings in all patients are the lack of tears. Lack of tears with crying is often mentioned in hindsight after the diagnosis has been made.[7] AAA Syndrome may be diagnosed in early childhood or in adolescence. The disorder is typically managed by treating the symptoms with hormone replacement for adrenal insufficiency, lubricating drops for the eyes and managing low blood sugars.[9]
Cause
Triple-A syndrome is associated with mutations in the AAAS gene which encodes a protein known as ALADIN (ALacrima Achalasia adrenal Insufficiency Neurologic disorder).[10][11][12] In 2000, Huebner et al. mapped the syndrome to a 6 cM interval on human chromosome 12q13 near the type II keratin gene cluster.[13] Since inheritance and gene for the association is known, early diagnosis can allow genetic counseling.[4] Furthermore, genotypic heterogeneity has also been documented suggesting that there may be other genes involved in this genetic disorder as well as unknown environmental factors that result in the phenotypic expression of the disease.[7]
ALADIN protein is a component of the nuclear pore complex, situated toward its cytoplasmic side. Mutant ALADIN remains mis-localized in the cytoplasm[14] and causes selective failure of nuclear protein import and hypersensitivity to oxidative stress.[15] Mutant ALADIN also causes decreased nuclear import of aprataxin, a repair protein for DNA single-strand breaks, and DNA ligase I.[15] These decreases in DNA repair proteins may allow accumulation of DNA damage that trigger cell death.[7]
Nucleoporin ALADIN participates in spindle assembly. ALADIN is employed in specific meiotic stages, including spindle assembly, and spindle positioning.[16] Female mice homozygously null for ALADIN are sterile.[16]
Diagnosis
The diagnosis of this condition involves examination by a health provider. Clinical signs may lead to the diagnosis such as the lack of tears and digestive issues, such as acid reflux disease in infancy as well as symptoms of adrenal insufficiency such as frequent bouts of low blood sugars are highly suggestive of the disorder.[7][5][9] Achalasia may be seen on plain X-rays and include an absence of fundal gas shadow, widened mediastinum and an air fluid level in mediastinum is also seen. The gold standard for confirming achalasia is a 24 hours manometry of oesophagus.This is a test that measures the pressure inside the esophagus. The test demonstrates non-relaxation of lower esophageal sphincter, increased tone of esophageal sphincter, atonic esophagus. Bird-beak sign and rat-tail sign can be appreciated on barium swallow.[17][18][19] Lack of tears or alacrima is caused by the lack of production of lacrimal glands or ducts and defects in the nerves of the lacrimal gland caused by a dysfunction in the autonomic nervous system.[20] The diagnosis is confirmed with genetic testing as well as clinical features.[9]
Treatment
There is no definitive cure for this syndrome, because many of the mechanisms implicated have not yet been identified. The available treatments address only some of the symptoms. Lubricating drops and emulsions are used to remedy the absence of tear secretion. Achalasia can be treated with surgical intervention resulting in improved passage of food and drink into the stomach. Corticosteroids, such as hydrocortisone, are prescribed to solve the adrenal insufficiency.[21] Early diagnosis may prevent morbidity and improve growth in children due to early treatment of adrenal insufficiency.[9]
See also
References
- Online Mendelian Inheritance in Man (OMIM): 231550
- Dusek T, Korsic M, Koehler K, Perkovic Z, Huebner A, Korsic M (2006). "A novel AAAS gene mutation (p.R194X) in a patient with triple A syndrome". Hormone Research. 65 (4): 171–176. doi:10.1159/000092003. PMID 16543750. S2CID 36128858.
- Gazarian M, Cowell CT, Bonney M, Grigor WG (January 1995). "The "4A" syndrome: adrenocortical insufficiency associated with achalasia, alacrima, autonomic and other neurological abnormalities". European Journal of Pediatrics. 154 (1): 18–23. doi:10.1007/BF01972967. PMID 7895750. S2CID 8904441.
- Bharadia L, Kalla M, Sharma SK, Charan R, Gupta JB, Khan F (2005). "Triple A syndrome". Indian Journal of Gastroenterology. 24 (5): 217–218. PMID 16361769.
- Tibussek D, Ghosh S, Huebner A, Schaper J, Mayatepek E, Koehler K (January 2018). ""Crying without tears" as an early diagnostic sign-post of triple A (Allgrove) syndrome: two case reports". BMC Pediatrics. 18 (1): 6. doi:10.1186/s12887-017-0973-y. PMC 5769402. PMID 29334914.
- Prpic I, Huebner A, Persic M, Handschug K, Pavletic M (May 2003). "Triple A syndrome: genotype-phenotype assessment". Clinical Genetics. 63 (5): 415–417. doi:10.1034/j.1399-0004.2003.00070.x. PMID 12752575. S2CID 19250948.
- Brooks BP, Kleta R, Stuart C, Tuchman M, Jeong A, Stergiopoulos SG, et al. (September 2005). "Genotypic heterogeneity and clinical phenotype in triple A syndrome: a review of the NIH experience 2000-2005". Clinical Genetics. 68 (3): 215–221. doi:10.1111/j.1399-0004.2005.00482.x. PMID 16098009. S2CID 20404052.
- Brooks BP, Kleta R, Stuart C, Tuchman M, Jeong A, Stergiopoulos SG, et al. (September 2005). "Genotypic heterogeneity and clinical phenotype in triple A syndrome: a review of the NIH experience 2000-2005". Clinical Genetics. 68 (3): 215–221. doi:10.1111/j.1399-0004.2005.00482.x. PMID 16098009. S2CID 20404052.
- "Triple A syndrome | Genetic and Rare Diseases Information Center (GARD) – an NCATS Program". rarediseases.info.nih.gov. Retrieved 2022-04-20.
- Huebner A, Kaindl AM, Knobeloch KP, Petzold H, Mann P, Koehler K (November 2004). "The triple A syndrome is due to mutations in ALADIN, a novel member of the nuclear pore complex". Endocrine Research. 30 (4): 891–899. doi:10.1081/ERC-200044138. PMID 15666842. S2CID 31047487.
- Salmaggi A, Zirilli L, Pantaleoni C, De Joanna G, Del Sorbo F, Koehler K, et al. (2008). "Late-onset triple A syndrome: a risk of overlooked or delayed diagnosis and management". Hormone Research. 70 (6): 364–372. doi:10.1159/000161867. PMID 18953174. S2CID 8097415.
- "Triple A Syndrome". Genetics Home Reference. February 2010. Retrieved 10 May 2020.
- Huebner A, Yoon SJ, Ozkinay F, Hilscher C, Lee H, Clark AJ, Handschug K (November 2000). "Triple A syndrome--clinical aspects and molecular genetics". Endocrine Research. 26 (4): 751–759. doi:10.3109/07435800009048596. PMID 11196451. S2CID 42579320.
- Krumbholz M, Koehler K, Huebner A (April 2006). "Cellular localization of 17 natural mutant variants of ALADIN protein in triple A syndrome - shedding light on an unexpected splice mutation". Biochemistry and Cell Biology. 84 (2): 243–249. doi:10.1139/o05-198. PMID 16609705.
- Hirano M, Furiya Y, Asai H, Yasui A, Ueno S (February 2006). "ALADINI482S causes selective failure of nuclear protein import and hypersensitivity to oxidative stress in triple A syndrome". Proceedings of the National Academy of Sciences of the United States of America. 103 (7): 2298–2303. Bibcode:2006PNAS..103.2298H. doi:10.1073/pnas.0505598103. PMC 1413683. PMID 16467144.
- Carvalhal S, Stevense M, Koehler K, Naumann R, Huebner A, Jessberger R, Griffis ER (September 2017). "ALADIN is required for the production of fertile mouse oocytes". Molecular Biology of the Cell. 28 (19): 2470–2478. doi:10.1091/mbc.E16-03-0158. PMC 5597320. PMID 28768824.
- Wallace IR, Hunter SJ (August 2012). "AAA syndrome--adrenal insufficiency, alacrima and achalasia". QJM. 105 (8): 803–804. doi:10.1093/qjmed/hcr145. PMID 21865313.
- Gaiani F, Gismondi P, Minelli R, Casadio G, de'Angelis N, Fornaroli F, et al. (May 2020). "Case report of a familial triple: a syndrome and review of the literature". Medicine. 99 (22): e20474. doi:10.1097/MD.0000000000020474. PMID 32481456.
- Yadav P, Kumar D, Bohra GK, Garg MK (May 2020). "Triple A syndrome (Allgrove syndrome) - A journey from clinical symptoms to a syndrome". Journal of Family Medicine and Primary Care. 9 (5): 2531–2534. doi:10.4103/jfmpc.jfmpc_237_20. PMC 7380807. PMID 32754538.
- Adams J, Schaaf CP (July 2018). "Diagnosis and genetics of alacrima". Clinical Genetics. 94 (1): 54–60. doi:10.1111/cge.13173. PMID 29120068. S2CID 32409479.
- Nicolino M (April 2013). "Triple A syndrome". Orphanet. Retrieved 31 August 2020.
External links
- Allgrove (AAA) Syndrome at eMedicine
- OMIM: 231550 Achalasia Addisonianism Alacrimia syndrome; Triple A syndrome at NIH's Office of Rare Diseases