Cytokine
Cytokines are a broad and loose category of small proteins (~5–25 kDa[1]) important in cell signaling. Cytokines are peptides and cannot cross the lipid bilayer of cells to enter the cytoplasm. Cytokines have been shown to be involved in autocrine, paracrine and endocrine signaling as immunomodulating agents.

Cytokines include chemokines, interferons, interleukins, lymphokines, and tumour necrosis factors, but generally not hormones or growth factors (despite some overlap in the terminology). Cytokines are produced by a broad range of cells, including immune cells like macrophages, B lymphocytes, T lymphocytes and mast cells, as well as endothelial cells, fibroblasts, and various stromal cells; a given cytokine may be produced by more than one type of cell.[2][3] They act through cell surface receptors and are especially important in the immune system; cytokines modulate the balance between humoral and cell-based immune responses, and they regulate the maturation, growth, and responsiveness of particular cell populations. Some cytokines enhance or inhibit the action of other cytokines in complex ways. They are different from hormones, which are also important cell signaling molecules. Hormones circulate in higher concentrations, and tend to be made by specific kinds of cells. Cytokines are important in health and disease, specifically in host immune responses to infection, inflammation, trauma, sepsis, cancer, and reproduction.
The word comes from the ancient Greek language: cyto, from Greek κύτος, kytos, 'cavity, cell' + kines, from Greek κίνησις, kinēsis, 'movement'.
Discovery
Interferon-alpha, an interferon type I, was identified in 1957 as a protein that interfered with viral replication.[4] The activity of interferon-gamma (the sole member of the interferon type II class) was described in 1965; this was the first identified lymphocyte-derived mediator.[5] Macrophage migration inhibitory factor (MIF) was identified simultaneously in 1966 by John David and Barry Bloom.[6][7]
In 1969, Dudley Dumonde proposed the term "lymphokine" to describe proteins secreted from lymphocytes and later, proteins derived from macrophages and monocytes in culture were called "monokines".[8] In 1974, pathologist Stanley Cohen, M.D. (not to be confused with the Nobel laureate) published an article describing the production of MIF in virus-infected allantoic membrane and kidney cells, showing its production is not limited to immune cells. This led to his proposal of the term cytokine.[9] Ogawa described the early acting growth factors, intermediate acting growth factors and late acting growth factors.[10]
Difference from hormones
Classic hormones circulate in aqueous solution in nanomolar (10-9 M) concentrations that usually vary by less than one order of magnitude. In contrast, some cytokines (such as IL-6) circulate in picomolar (10-12 M) concentrations that can increase up to 1,000 times during trauma or infection. The widespread distribution of cellular sources for cytokines may be a feature that differentiates them from hormones. Virtually all nucleated cells, but especially endo/epithelial cells and resident macrophages (many near the interface with the external environment) are potent producers of IL-1, IL-6, and TNF-α.[11] In contrast, classic hormones, such as insulin, are secreted from discrete glands such as the pancreas.[12] The current terminology refers to cytokines as immunomodulating agents.
A contributing factor to the difficulty of distinguishing cytokines from hormones is that some immunomodulating effects of cytokines are systemic (i.e., affecting the whole organism) rather than local. For instance, to accurately utilize hormone terminology, cytokines may be autocrine or paracrine in nature, and chemotaxis, chemokinesis and endocrine as a pyrogen. Essentially, cytokines are not limited to their immunomodulatory status as molecules.
Nomenclature
Cytokines have been classed as lymphokines, interleukins, and chemokines, based on their presumed function, cell of secretion, or target of action. Because cytokines are characterised by considerable redundancy and pleiotropism, such distinctions, allowing for exceptions, are obsolete.
- The term interleukin was initially used by researchers for those cytokines whose presumed targets are principally white blood cells (leukocytes). It is now used largely for designation of newer cytokine molecules and bears little relation to their presumed function. The vast majority of these are produced by T-helper cells.
- Lymphokines: produced by lymphocytes
- Monokines: produced exclusively by monocytes
- Interferons: involved in antiviral responses
- Colony stimulating factors: support the growth of cells in semisolid media
- Chemokines: mediate chemoattraction (chemotaxis) between cells.
Classification
Structural
Structural homogeneity has been able to partially distinguish between cytokines that do not demonstrate a considerable degree of redundancy so that they can be classified into four types:
- The four-α-helix bundle family (InterPro: IPR009079): member cytokines have three-dimensional structures with a bundle of four α-helices. This family, in turn, is divided into three sub-families:
- the IL-2 subfamily. This is the largest family. It contains several non-immunological cytokines including erythropoietin (EPO) and thrombopoietin (TPO).[13] They can be grouped into long-chain and short-chain cytokines by topology.[14] Some members share the common gamma chain as part of their receptor.[15]
- the interferon (IFN) subfamily.
- the IL-10 subfamily.
- The IL-1 family, which primarily includes IL-1 and IL-18.
- The cysteine knot cytokines (IPR029034) include members of the transforming growth factor beta superfamily, including TGF-β1, TGF-β2 and TGF-β3.
- The IL-17 family, which has yet to be completely characterized, though member cytokines have a specific effect in promoting proliferation of T-cells that cause cytotoxic effects.
Functional
A classification that proves more useful in clinical and experimental practice outside of structural biology divides immunological cytokines into those that enhance cellular immune responses, type 1 (TNFα, IFN-γ, etc.), and those that enhance antibody responses, type 2 (TGF-β, IL-4, IL-10, IL-13, etc.). A key focus of interest has been that cytokines in one of these two sub-sets tend to inhibit the effects of those in the other. Dysregulation of this tendency is under intensive study for its possible role in the pathogenesis of autoimmune disorders. Several inflammatory cytokines are induced by oxidative stress.[16][17] The fact that cytokines themselves trigger the release of other cytokines [18][19][20] and also lead to increased oxidative stress makes them important in chronic inflammation, as well as other immunoresponses, such as fever and acute phase proteins of the liver (IL-1,6,12, IFN-a). Cytokines also play a role in anti-inflammatory pathways and are a possible therapeutic treatment for pathological pain from inflammation or peripheral nerve injury.[21] There are both pro-inflammatory and anti-inflammatory cytokines that regulate this pathway.
Receptors
In recent years, the cytokine receptors have come to demand the attention of more investigators than cytokines themselves, partly because of their remarkable characteristics and partly because a deficiency of cytokine receptors has now been directly linked to certain debilitating immunodeficiency states. In this regard, and also because the redundancy and pleomorphism of cytokines are, in fact, a consequence of their homologous receptors, many authorities think that a classification of cytokine receptors would be more clinically and experimentally useful.
A classification of cytokine receptors based on their three-dimensional structure has, therefore, been attempted. Such a classification, though seemingly cumbersome, provides several unique perspectives for attractive pharmacotherapeutic targets.
- Immunoglobulin (Ig) superfamily, which are ubiquitously present throughout several cells and tissues of the vertebrate body, and share structural homology with immunoglobulins (antibodies), cell adhesion molecules, and even some cytokines. Examples: IL-1 receptor types.
- Hemopoietic Growth Factor (type 1) family, whose members have certain conserved motifs in their extracellular amino-acid domain. The IL-2 receptor belongs to this chain, whose γ-chain (common to several other cytokines) deficiency is directly responsible for the x-linked form of Severe Combined Immunodeficiency (X-SCID).
- Interferon (type 2) family, whose members are receptors for IFN β and γ.
- Tumor necrosis factors (TNF) (type 3) family, whose members share a cysteine-rich common extracellular binding domain, and includes several other non-cytokine ligands like CD40, CD27 and CD30, besides the ligands on which the family is named.
- Seven transmembrane helix family, the ubiquitous receptor type of the animal kingdom. All G protein-coupled receptors (for hormones and neurotransmitters) belong to this family. Chemokine receptors, two of which act as binding proteins for HIV (CD4 and CCR5), also belong to this family.
- Interleukin-17 receptor (IL-17R) family, which shows little homology with any other cytokine receptor family. Structural motifs conserved between members of this family include: an extracellular fibronectin III-like domain, a transmembrane domain and a cytoplasmic SERIF domain. The known members of this family are as follows: IL-17RA, IL-17RB, IL-17RC, IL17RD and IL-17RE.[22]
Cellular effects
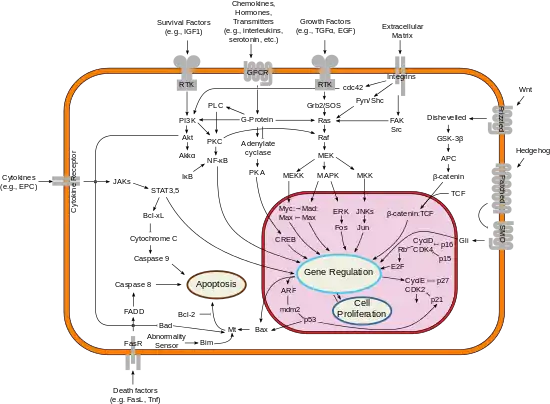
Each cytokine has a matching cell-surface receptor. Subsequent cascades of intracellular signaling then alter cell functions. This may include the upregulation and/or downregulation of several genes and their transcription factors, resulting in the production of other cytokines, an increase in the number of surface receptors for other molecules, or the suppression of their own effect by feedback inhibition. The effect of a particular cytokine on a given cell depends on the cytokine, its extracellular abundance, the presence and abundance of the complementary receptor on the cell surface, and downstream signals activated by receptor binding; these last two factors can vary by cell type. Cytokines are characterized by considerable redundancy, in that many cytokines appear to share similar functions. It seems to be a paradox that cytokines binding to antibodies have a stronger immune effect than the cytokine alone. This may lead to lower therapeutic doses.
It has been shown that inflammatory cytokines cause an IL-10-dependent inhibition of[23] T-cell expansion and function by up-regulating PD-1 levels on monocytes, which leads to IL-10 production by monocytes after binding of PD-1 by PD-L.[23] Adverse reactions to cytokines are characterized by local inflammation and/or ulceration at the injection sites. Occasionally such reactions are seen with more widespread papular eruptions.[24]
Roles in health and disease
Cytokines are involved in several developmental processes during embryonic development.[25][nb 1][26][nb 2] Cytokines are released from the blastocyst, and are also expressed in the endometrium, and have critical roles in the stages of zona hatching, and implantation.[27] Cytokines are crucial for fighting off infections and in other immune responses.[28] However, they can become dysregulated and pathological in inflammation, trauma, sepsis,[28] and hemorrhagic stroke.[29] Dysregulated cytokine secretion in the aged population can lead to inflammaging, and render these individuals more vulnerable to age-related diseases like neurodegenerative diseases and type 2 diabetes.[30]
Adverse effects
Adverse effects of cytokines have been linked to many disease states and conditions ranging from schizophrenia, major depression[31] and Alzheimer's disease[32] to cancer.[33] T regulatory cells (Tregs) and related-cytokines are effectively engaged in the process of tumor immune escape and functionally inhibit immune response against the tumor. Forkhead box protein 3 (Foxp3) as a transcription factor is an essential molecular marker of Treg cells. Foxp3 polymorphism (rs3761548) might be involved in cancer progression like gastric cancer through influencing Tregs function and the secretion of immunomodulatory cytokines such as IL-10, IL-35, and TGF-β.[34] Normal tissue integrity is preserved by feedback interactions between diverse cell types mediated by adhesion molecules and secreted cytokines; disruption of normal feedback mechanisms in cancer threatens tissue integrity.[35]
Over-secretion of cytokines can trigger a dangerous cytokine storm syndrome. Cytokine storms may have been the cause of severe adverse events during a clinical trial of TGN1412. Cytokine storms are also suspected to be the main cause of death in the 1918 "Spanish Flu" pandemic. Deaths were weighted more heavily towards people with healthy immune systems, because of their ability to produce stronger immune responses, with dramatic increases in cytokine levels. Another example of cytokine storm is seen in acute pancreatitis. Cytokines are integral and implicated in all angles of the cascade, resulting in the systemic inflammatory response syndrome and multi-organ failure associated with this intra-abdominal catastrophe.[36] In the COVID-19 pandemic, some deaths from COVID-19 have been attributable to cytokine release storms.[37][38][39] Current data suggest cytokine storms may be the source of extensive lung tissue damage and dysfunctional coagulation in COVID-19 infections.[40]
Medical use as drugs
Some cytokines have been developed into protein therapeutics using recombinant DNA technology.[41] Recombinant cytokines being used as drugs as of 2014 include:[42]
- Bone morphogenetic protein (BMP), used to treat bone-related conditions
- Erythropoietin (EPO), used to treat anemia
- Granulocyte colony-stimulating factor (G-CSF), used to treat neutropenia in cancer patients
- Granulocyte macrophage colony-stimulating factor (GM-CSF), used to treat neutropenia and fungal infections in cancer patients
- Interferon alfa, used to treat hepatitis C and multiple sclerosis
- Interferon beta, used to treat multiple sclerosis
- Interleukin 2 (IL-2), used to treat cancer.
- Interleukin 11 (IL-11), used to treat thrombocytopenia in cancer patients.
- Interferon gamma is used to treat chronic granulomatous disease[43] and osteopetrosis[44]
See also
- Adipokines
- Apoptosis
- Cytokine redundancy
- Cytokine release syndrome
- Cytokine secretion assay
- ELISA assays
- Myokine
- Signal transduction
- Thymic stromal lymphopoietin
- Virokine
Notes
- Saito explains "much evidence has suggested that cytokines and chemokines play a very important role in the reproduction, i.e. embryo implantation, endometrial development, and trophoblast growth and differentiation by modulating the immune and endocrine systems."(15)
- Chen explains the regulatory activity of LIF in human and murine embryos: "In conclusion, human preimplantation embryos express LIF and LIF-R mRNA. The expression of these transcripts indicates that preimplantation embryos may be responsive to LIF originating either from the surrounding environment or from the embryos themselves and exerting its function in a paracrine or autocrine manner."(719)
References
- Janeway's Immunobiology. Garland Science. 2017. p. 107. ISBN 978-0-8153-4551-0.
- Lackie J (2010). "Cytokines". A Dictionary of Biomedicine. Oxford University Press. ISBN 978-0-19-954935-1.
- "Cytokine". Stedman's Medical Dictionary (28th ed.). Wolters Kluwer Health, Lippincott Williams & Wilkins. 2006. ISBN 978-0-7817-6450-6.
- Isaacs A, Lindenmann J (September 1957). "Virus interference. I. The interferon". Proc. R. Soc. Lond. B Biol. Sci. 147 (927): 258–67. Bibcode:1957RSPSB.147..258I. doi:10.1098/rspb.1957.0048. PMID 13465720. S2CID 202574492.
- Wheelock EF (July 1965). "Interferon-Like Virus-Inhibitor Induced in Human Leukocytes by Phytohemagglutinin". Science. 149 (3681): 310–11. Bibcode:1965Sci...149..310W. doi:10.1126/science.149.3681.310. PMID 17838106. S2CID 1366348.
- Bloom BR, Bennett B (July 1966). "Mechanism of a reaction in vitro associated with delayed-type hypersensitivity". Science. 153 (3731): 80–82. Bibcode:1966Sci...153...80B. doi:10.1126/science.153.3731.80. PMID 5938421. S2CID 43168526.
- David JR (July 1966). "Delayed hypersensitivity in vitro: its mediation by cell-free substances formed by lymphoid cell-antigen interaction". Proc. Natl. Acad. Sci. U.S.A. 56 (1): 72–77. Bibcode:1966PNAS...56...72D. doi:10.1073/pnas.56.1.72. PMC 285677. PMID 5229858.
- Dumonde DC, Wolstencroft RA, Panayi GS, Matthew M, Morley J, Howson WT (October 1969). ""Lymphokines": non-antibody mediators of cellular immunity generated by lymphocyte activation". Nature. 224 (5214): 38–42. Bibcode:1969Natur.224...38D. doi:10.1038/224038a0. PMID 5822903. S2CID 4172811.
- Cohen S, Bigazzi PE, Yoshida T (April 1974). "Commentary. Similarities of T cell function in cell-mediated immunity and antibody production". Cell. Immunol. 12 (1): 150–59. doi:10.1016/0008-8749(74)90066-5. PMID 4156495.
- Ogawa, M (1993). "Differentiation and proliferation of hematopoetic stem cells". Blood. 81 (11): 2844–53. doi:10.1182/blood.V81.11.2844.2844. PMID 8499622.
- Boyle JJ (January 2005). "Macrophage activation in atherosclerosis: pathogenesis and pharmacology of plaque rupture". Current Vascular Pharmacology. 3 (1): 63–8. CiteSeerX 10.1.1.324.9948. doi:10.2174/1570161052773861. PMID 15638783.
- Cannon JG (December 2000). "Inflammatory Cytokines in Nonpathological States". News in Physiological Sciences. 15 (6): 298–303. doi:10.1152/physiologyonline.2000.15.6.298. PMID 11390930.
- Leonard WJ (December 2001). "Cytokines and immunodeficiency diseases". Nature Reviews. Immunology. 1 (3): 200–8. doi:10.1038/35105066. PMID 11905829. S2CID 5466985.
- Rozwarski DA, Gronenborn AM, Clore GM, Bazan JF, Bohm A, Wlodawer A, et al. (March 1994). "Structural comparisons among the short-chain helical cytokines". Structure. 2 (3): 159–73. doi:10.1016/s0969-2126(00)00018-6. PMID 8069631.
- Reche PA (April 2019). "The tertiary structure of γc cytokines dictates receptor sharing". Cytokine. 116: 161–168. doi:10.1016/j.cyto.2019.01.007. PMID 30716660. S2CID 73449371.
- Vlahopoulos S, Boldogh I, Casola A, Brasier AR (September 1999). "Nuclear factor-kappaB-dependent induction of interleukin-8 gene expression by tumor necrosis factor alpha: evidence for an antioxidant sensitive activating pathway distinct from nuclear translocation". Blood. 94 (6): 1878–89. doi:10.1182/blood.V94.6.1878.418k03_1878_1889. PMID 10477716. S2CID 25974629.
- David F, Farley J, Huang H, Lavoie JP, Laverty S (April 2007). "Cytokine and chemokine gene expression of IL-1beta stimulated equine articular chondrocytes". Vet Surg. 36 (3): 221–27. doi:10.1111/j.1532-950X.2007.00253.x. PMID 17461946.
- Chokkalingam V, Tel J, Wimmers F, Liu X, Semenov S, Thiele J, Figdor CG, Huck WT (December 2013). "Probing cellular heterogeneity in cytokine-secreting immune cells using droplet-based microfluidics". Lab Chip. 13 (24): 4740–44. doi:10.1039/c3lc50945a. PMID 24185478.
- Carpenter LR, Moy JN, Roebuck KA (March 2002). "Respiratory syncytial virus and TNF alpha induction of chemokine gene expression involves differential activation of Rel A and NF-kappa B1". BMC Infect. Dis. 2: 5. doi:10.1186/1471-2334-2-5. PMC 102322. PMID 11922866.
- Tian B, Nowak DE, Brasier AR (September 2005). "A TNF-induced gene expression program under oscillatory NF-kappaB control". BMC Genomics. 6: 137. doi:10.1186/1471-2164-6-137. PMC 1262712. PMID 16191192.
- Zhang JM, An J (2007). "Cytokines, inflammation, and pain". Int Anesthesiol Clin. 45 (2): 27–37. doi:10.1097/AIA.0b013e318034194e. PMC 2785020. PMID 17426506.
- Gaffen SL (August 2009). "Structure and signalling in the IL-17 receptor family". Nat. Rev. Immunol. 9 (8): 556–67. doi:10.1038/nri2586. PMC 2821718. PMID 19575028.
- Said EA, Dupuy FP, Trautmann L, Zhang Y, Shi Y, El-Far M, et al. (April 2010). "Programmed death-1-induced interleukin-10 production by monocytes impairs CD4+ T cell activation during HIV infection". Nature Medicine. 16 (4): 452–9. doi:10.1038/nm.2106. PMC 4229134. PMID 20208540.
- James, William; Berger, Timothy; Elston, Dirk (2005). Andrews' Diseases of the Skin: Clinical Dermatology. (10th ed.). Saunders. ISBN 0-7216-2921-0.
- Saito S (2001). "Cytokine cross-talk between mother and the embryo/placenta". J. Reprod. Immunol. 52 (1–2): 15–33. doi:10.1016/S0165-0378(01)00112-7. PMID 11600175.
- Chen HF, Shew JY, Ho HN, Hsu WL, Yang YS (October 1999). "Expression of leukemia inhibitory factor and its receptor in preimplantation embryos". Fertil. Steril. 72 (4): 713–19. doi:10.1016/S0015-0282(99)00306-4. PMID 10521116.
- Seshagiri, Polani B.; Vani, Venkatappa; Madhulika, Pathak (March 2016). "Cytokines and Blastocyst Hatching". American Journal of Reproductive Immunology. pp. 208–217. doi:10.1111/aji.12464. Retrieved 2 November 2022.
- Dinarello CA (August 2000). "Proinflammatory cytokines". Chest. 118 (2): 503–08. doi:10.1378/chest.118.2.503. PMID 10936147.
- Zhu H, Wang Z, Yu J, et al. (March 2019). "Role and mechanisms of cytokines in the secondary brain injury after intracerebral hemorrhage". Prog. Neurobiol. 178: 101610. doi:10.1016/j.pneurobio.2019.03.003. PMID 30923023. S2CID 85495400.
- Franceschi, C.; Bonafè, M.; Valensin, S.; Olivieri, F.; De Luca, M.; Ottaviani, E.; De Benedictis, G. (June 2000). "Inflamm-aging. An evolutionary perspective on immunosenescence". Annals of the New York Academy of Sciences. 908 (1): 244–254. Bibcode:2000NYASA.908..244F. doi:10.1111/j.1749-6632.2000.tb06651.x. ISSN 0077-8923. PMID 10911963. S2CID 1843716.
- Dowlati Y, Herrmann N, Swardfager W, Liu H, Sham L, Reim EK, Lanctôt KL (March 2010). "A meta-analysis of cytokines in major depression". Biol. Psychiatry. 67 (5): 446–57. doi:10.1016/j.biopsych.2009.09.033. PMID 20015486. S2CID 230209.
- Swardfager W, Lanctôt K, Rothenburg L, Wong A, Cappell J, Herrmann N (November 2010). "A meta-analysis of cytokines in Alzheimer's disease". Biol. Psychiatry. 68 (10): 930–41. doi:10.1016/j.biopsych.2010.06.012. PMID 20692646. S2CID 6544784.
- Locksley RM, Killeen N, Lenardo MJ (February 2001). "The TNF and TNF receptor superfamilies: integrating mammalian biology". Cell. 104 (4): 487–501. doi:10.1016/S0092-8674(01)00237-9. PMID 11239407. S2CID 7657797.
- Ezzeddini R, Somi MH, Taghikhani M, Moaddab SY, Masnadi Shirazi K, Shirmohammadi M, Eftekharsadat AT, Sadighi Moghaddam B, Salek Farrokhi A (February 2021). "Association of Foxp3 rs3761548 polymorphism with cytokines concentration in gastric adenocarcinoma patients". Cytokine. 138: 155351. doi:10.1016/j.cyto.2020.155351. ISSN 1043-4666. PMID 33127257. S2CID 226218796.
- Vlahopoulos SA, Cen O, Hengen N, Agan J, Moschovi M, Critselis E, Adamaki M, Bacopoulou F, Copland JA, Boldogh I, Karin M, Chrousos GP (August 2015). "Dynamic aberrant NF-κB spurs tumorigenesis: a new model encompassing the microenvironment". Cytokine Growth Factor Rev. 26 (4): 389–403. doi:10.1016/j.cytogfr.2015.06.001. PMC 4526340. PMID 26119834.
- Makhija R, Kingsnorth AN (2002). "Cytokine storm in acute pancreatitis". Journal of Hepato-Biliary-Pancreatic Surgery. 9 (4): 401–10. doi:10.1007/s005340200049. PMID 12483260.
- Cron, Randy; Chatham, W. Winn (12 March 2020). "How doctors can potentially significantly reduce the number of deaths from Covid-19". Vox. Retrieved 14 March 2020.
- Ruan Q, Yang K, Wang W, Jiang L, Song J (May 2020). "Clinical predictors of mortality due to COVID-19 based on an analysis of data of 150 patients from Wuhan, China". Intensive Care Medicine. 46 (5): 846–848. doi:10.1007/s00134-020-05991-x. PMC 7080116. PMID 32125452.
- Mehta P, McAuley DF, Brown M, Sanchez E, Tattersall RS, Manson JJ (March 2020). "COVID-19: consider cytokine storm syndromes and immunosuppression". Lancet. 395 (10229): 1033–1034. doi:10.1016/S0140-6736(20)30628-0. PMC 7270045. PMID 32192578.
- Cascella M, Rajnik M, Cuomo A, et al. (4 October 2020). "Features, Evaluation, and Treatment of Coronavirus". StatPearls Publishing. PMID 32150360. Retrieved 4 December 2020.
{{cite journal}}: Cite journal requires|journal=(help) - Anne S De Root, David W Scott (November 2007). "Immunogenicity of protein therapeutics". Trends in Immunology. 28 (11): 482–490. doi:10.1016/j.it.2007.07.011. PMID 17964218.
{{cite journal}}: CS1 maint: uses authors parameter (link) - Dimitrov DS (2012). "Therapeutic Proteins". Methods in Molecular Biology. Vol. 899. pp. 1–26. doi:10.1007/978-1-61779-921-1_1. ISBN 978-1-61779-920-4. PMC 6988726. PMID 22735943.
{{cite book}}: Missing or empty|title=(help) - Woodman RC, Erickson RW, Rae J, Jaffe HS, Curnutte JT (March 1992). "Prolonged recombinant interferon-gamma therapy in chronic granulomatous disease: evidence against enhanced neutrophil oxidase activity". Blood. 79 (6): 1558–62. doi:10.1182/blood.v79.6.1558.bloodjournal7961558. PMID 1312372.
- Key LL, Rodriguiz RM, Willi SM, Wright NM, Hatcher HC, Eyre DR, Cure JK, Griffin PP, Ries WL (June 1995). "Long-term treatment of osteopetrosis with recombinant human interferon gamma". N. Engl. J. Med. 332 (24): 1594–99. doi:10.1056/NEJM199506153322402. PMID 7753137.