Amblyopia
Amblyopia, also called lazy eye, is a disorder of sight in which the brain fails to fully process input from one eye and over time favors the other eye.[1] It results in decreased vision in an eye that typically appears normal in other aspects. [1] Amblyopia is the most common cause of decreased vision in a single eye among children and younger adults.[1]
| Amblyopia | |
|---|---|
| Other names | Lazy eye[1] |
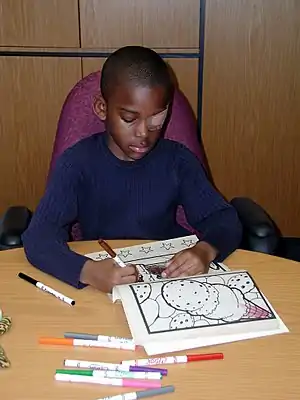 | |
| A child wearing an adhesive eyepatch to correct amblyopia | |
| Pronunciation |
|
| Specialty | Ophthalmology, optometry |
| Symptoms | Decreased vision |
| Usual onset | Before age five[2] |
| Causes | Poor alignment of the eyes, eye being irregularly shaped such that focusing is difficult, one eye being more nearsighted or farsighted, clouding of the lens[1] |
| Diagnostic method | Vision testing[1] |
| Differential diagnosis | Brainstem disorders, optic nerve disorder, eye diseases[3] |
| Treatment | Glasses, eyepatch[1][2][4] |
| Frequency | ~2% of adults[5] |
The cause of amblyopia can be any condition that interferes with focusing during early childhood.[1][6] This can occur from poor alignment of the eyes (strabismic), an eye being irregularly shaped such that focusing is difficult, one eye being more nearsighted or farsighted than the other (refractive), or clouding of the lens of an eye (deprivational).[1] After the underlying cause is addressed, vision is not restored right away, as the mechanism also involves the brain.[6][7] Amblyopia can be difficult to detect, so vision testing is recommended for all children around the ages of four to five.[2]
Early detection improves treatment success.[2] Glasses may be all the treatment needed for some children.[2][4] If this is not sufficient, treatments which encourage or force the child to use the weaker eye are used.[1] This is done by either using a patch or putting atropine in the stronger eye.[1][8] Without treatment, amblyopia typically persists.[1] Treatment in adulthood is usually much less effective.[1]
Amblyopia begins by the age of five.[2] In adults, the disorder is estimated to affect 1–5% of the population.[5] While treatment improves vision, it does not typically restore it to normal in the affected eye.[2] Amblyopia was first described in the 1600s.[9] The condition may make people ineligible to be pilots or police officers.[2] The word amblyopia is from Greek ἀμβλύς amblys, meaning "blunt", and ὤψ ōps, meaning "sight".[10]
Signs and symptoms
Many people with amblyopia, especially those who only have a mild form, are not aware they have the condition until tested at older ages, since the vision in their stronger eye is normal. People with amblyopia typically have poor stereo vision, since it requires both eyes. They further may have, on the affected eye, poor pattern recognition, poor visual acuity, and low sensitivity to contrast and motion.[11]
Amblyopia is characterized by several functional abnormalities in spatial vision, including reductions in visual acuity, contrast sensitivity function, and vernier acuity, as well as spatial distortion, abnormal spatial interactions, and impaired contour detection. In addition, individuals with amblyopia have binocular abnormalities such as impaired stereoacuity (stereoscopic acuity) and abnormal binocular summation.[12] Also, central vision in amblyopes is more crowded than central vision in normal observers.[13]
These deficits are usually specific to the amblyopic eye. Subclinical deficits of the "better" eye have also been demonstrated.[14]
People with amblyopia also have problems of binocular vision such as limited stereoscopic depth perception and usually have difficulty seeing the three-dimensional images in hidden stereoscopic displays such as autostereograms.[15] Perception of depth, from monocular cues such as size, perspective, and motion parallax remains normal.
Cause
Amblyopia has three main causes:
- Strabismic: by strabismus (misaligned eyes)
- Refractive: by anisometropia (difference of a certain degree of nearsightedness, farsightedness, or astigmatism), or by significant amount of equal refractive error in both eyes
- Deprivational: by deprivation of vision early in life by vision-obstructing disorders such as congenital cataract[16]
Strabismus
Strabismus, sometimes also incorrectly called lazy eye, is a condition in which the eyes are misaligned.[17] Strabismus usually results in normal vision in the preferred sighting (or "fellow") eye (the eye that the person prefers to use), but may cause abnormal vision in the deviating or strabismic eye due to the difference between the images projecting to the brain from the two eyes.[18] Adult-onset strabismus usually causes double vision (diplopia), since the two eyes are not fixed on the same object. Children's brains are more neuroplastic, so can more easily adapt by suppressing images from one of the eyes, eliminating the double vision. This plastic response of the brain, interrupts the brain's normal development, resulting in the amblyopia. Recent evidence points to a cause of infantile strabismus lying with the input to the visual cortex.[19]
Those with strabismic amblyopia tend to show ocular motion deficits when reading, even when they use the nonamblyopic eye. In particular, they tend to make more saccades per line than persons with normal stereo vision, and to have a reduced reading speed, especially when reading a text with small font size.[20][21]
Strabismic amblyopia is treated by clarifying the visual image with glasses, or encouraging use of the amblyopic eye with an eyepatch over the dominant eye or pharmacologic penalization of the better eye. Penalization usually consists of applying atropine drops to temporarily paralyze the accommodation reflex, leading to the blurring of vision in the good eye. It also dilates the pupil. This helps to prevent the bullying and teasing associated with wearing a patch, although sometimes application of the eye drops is challenging. The ocular alignment itself may be treated with surgical or nonsurgical methods, depending on the type and severity of the strabismus.[22]
Refractive
Refractive amblyopia may result from anisometropia (unequal refractive error between the two eyes).[23][24] Anisometropia exists when there is a difference in the power between the two eyes. The eye which provides the brain with a clearer image typically becomes the dominant eye. The image in the other eye is blurred, which results in abnormal development of one half of the visual system. Refractive amblyopia is usually less severe than strabismic amblyopia and is commonly missed by primary care physicians because of its less dramatic appearance and lack of obvious physical manifestation, such as with strabismus.[25] Given that the refractive correction of anisometropia by means of spectacles typically leads to different image magnification for the two eyes, which may in turn prevent binocular vision, a refractive correction using contact lenses is to be considered. Also pediatric refractive surgery is a treatment option, in particular if conventional approaches have failed due to aniseikonia or lack of compliance or both.[26]
Frequently, amblyopia is associated with a combination of anisometropia and strabismus. In some cases, the vision between the eyes can differ to the point where one eye has twice average vision while the other eye is completely blind.
Deprivation and occlusion
Deprivation amblyopia (amblyopia ex anopsia) results when the ocular media become opaque, such as is the case with congenital cataract or corneal haziness.[27] These opacities prevent adequate visual input from reaching the eye, and disrupt development. If not treated in a timely fashion, amblyopia may persist even after the cause of the opacity is removed. Sometimes, drooping of the eyelid (ptosis) or some other problem causes the upper eyelid to physically occlude a child's vision, which may cause amblyopia quickly. Occlusion amblyopia may be a complication of a hemangioma that blocks some or all of the eye. Other possible causes of deprivation and occlusion amblyopia include obstruction in the vitreous and aphakia.[28] Deprivation amblyopia accounts for less than 3% of all individuals affected by amblyopia.[28]
Pathophysiology
Amblyopia is a developmental problem in the brain, not any intrinsic, organic neurological problem in the eyeball (although organic problems can lead to amblyopia which can continue to exist after the organic problem has resolved by medical intervention).[29] The part of the brain receiving images from the affected eye is not stimulated properly and does not develop to its full visual potential. This has been confirmed by direct brain examination. David H. Hubel and Torsten Wiesel won the Nobel Prize in Physiology or Medicine in 1981 for their work in showing the extent of the damage to ocular dominance columns produced in kittens by sufficient visual deprivation during the so-called "critical period". The maximum "critical period" in humans is from birth to two years old.[30]
Diagnosis
Amblyopia is diagnosed by identifying low visual acuity in one or both eyes, out of proportion to the structural abnormality of the eye and excluding other visual disorders as causes for the lowered visual acuity. It can be defined as an interocular difference of two lines or more in acuity (e.g. on Snellen chart) when the eye optics are maximally corrected.[31] In young children, visual acuity is difficult to measure and can be estimated by observing the reactions of the patient when one eye is covered, including observing the patient's ability to follow objects with one eye.
Stereotests like the Lang stereotest are not reliable exclusion tests for amblyopia. A person who passes the Lang stereotest test is unlikely to have strabismic amblyopia, but could nonetheless have refractive or deprivational amblyopia.[32] Binocular retinal birefringence scanning may be able to identify, already in very young children, amblyopia that is associated with strabismus, microstrabismus, or reduced fixation accuracy. Diagnosis and treatment of amblyopia as early as possible is necessary to keep the vision loss to a minimum. Screening for amblyopia is recommended in all people between three and five years of age.[33]
Treatment
Treatment of strabismic or anisometropic amblyopia consists of correcting the optical deficit (wearing the necessary spectacle prescription) and often forcing use of the amblyopic eye, by patching the good eye, or instilling topical atropine in the good eye, or both.[17]: 130 [34] Atropine appears to result in similar outcomes to patching.[35][36] If there is overpatching or overpenalizing the good eye when treating amblyopia, "reverse amblyopia" can result.[22][37] Eye patching is usually done on a part-time schedule of about 4–6 hours a day. Treatment is continued as long as vision improves. It is not worthwhile continuing to patch for more than 6 months if no improvement continues.[38]
Deprivation amblyopia is treated by removing the opacity as soon as possible followed by patching or penalizing the good eye to encourage the use of the amblyopic eye.[22] The earlier the treatment is initiated, the easier and faster the treatment is and the less psychologically damaging. Also, the chance of achieving 20/20 vision is greater if treatment is initiated early.[39]
One of the German public health insurance providers, Barmer, has changed its policy to cover, as of 1 April 2014, the cost of software for amblyopic children whose condition did not improve through patching. The app offers dedicated eye exercises that the patient performs while wearing an eyepatch.[40]
Evidence for vision therapy is unclear as of 2011.[41]
Epidemiology
Amblyopia occurs in between 2 and 5% of the population in Western countries.[31][45] In the UK, 90% of visual health appointments in the child concern amblyopia.[46]
Depending on the chosen criterion for diagnosis, between 1 and 4% of the children have amblyopia.[47]
Research
A 2009 study,[48] widely reported in the popular press,[49] has suggested that repetitive transcranial magnetic stimulation may temporarily improve contrast sensitivity and spatial resolution in the affected eye of adults with amblyopia. This approach is still under development,[50] and the results await verification by other researchers. Comparable results may be achieved using different types of brain stimulation,[51] such as anodal transcranial direct current stimulation[52] and theta burst rTMS.[53]
A 2013 study concluded that converging evidence indicates decorrelated binocular experience plays a pivotal role in the genesis of amblyopia and the associated residual deficits.[54] Another study of 2013[55] suggests that playing a version of the popular game Tetris that is modified such that each eye sees separate components of the game may also help to treat this condition in adults.[56] Furthermore, the effects of this kind of therapy may be further enhanced by noninvasive brain stimulation[51] as shown by a recent study using anodal tDCS.[57]
A 2014 Cochrane review sought to determine the effectiveness of occlusion treatment on patients with sensory deprivation amblyopia, but no trials were found eligible to be included in the review.[28] However, good outcomes from occlusion treatment for sensory deprivation amblyopia likely rely on compliance with the treatment.
References
- "Facts About Amblyopia". National Eye Institute. September 2013. Archived from the original on 27 July 2016. Retrieved 27 July 2016.
- Jefferis JM, Connor AJ, Clarke MP (November 2015). "Amblyopia". BMJ. 351: h5811. doi:10.1136/bmj.h5811. PMID 26563241. S2CID 220101666.
- Ferri FF (2010). Ferri's differential diagnosis: a practical guide to the differential diagnosis of symptoms, signs, and clinical disorders (2nd ed.). Philadelphia, PA: Elsevier/Mosby. p. Chapter A. ISBN 978-0-323-07699-9.
- Maconachie GD, Gottlob I (December 2015). "The challenges of amblyopia treatment". Biomedical Journal. 38 (6): 510–6. doi:10.1016/j.bj.2015.06.001. PMC 6138377. PMID 27013450.
- Webber AL, Wood J (November 2005). "Amblyopia: prevalence, natural history, functional effects and treatment". Clinical & Experimental Optometry. 88 (6): 365–75. doi:10.1111/j.1444-0938.2005.tb05102.x. PMID 16329744. S2CID 39141527.
- Schwartz MW (2002). The 5-minute pediatric consult (3rd ed.). Philadelphia: Lippincott Williams & Wilkins. p. 110. ISBN 978-0-7817-3539-1.
- Levi DM (November 2013). "Linking assumptions in amblyopia". Visual Neuroscience. 30 (5–6): 277–87. doi:10.1017/S0952523813000023. PMC 5533593. PMID 23879956.
- "Amblyopia (Lazy Eye)". National Eye Institute. 2 July 2019. Retrieved 31 January 2020.
Putting special eye drops in the stronger eye. A once-a-day drop of the drug atropine can temporarily blur near vision, which forces the brain to use the other eye. For some kids, this treatment works as well as an eye patch, and some parents find it easier to use (for example, because young children may try to pull off eye patches).
- Bianchi PE, Ricciardelli G, Bianchi A, Arbanini A, Fazzi E (2016). "Chapter 2: Visual Development in Childhood". In Fazzi E, Bianchi PE (eds.). Visual Impairments and Developmental Disorders: From diagnosis to rehabilitation Mariani Foundation Paediatric Neurology. John Libbey Eurotext. ISBN 978-2-7420-1482-8. Archived from the original on 8 September 2017. Retrieved 27 July 2016.
- "Online Etymology Dictionary". www.etymonline.com. Archived from the original on 8 September 2017. Retrieved 5 May 2017.
- Hess RF, Mansouri B, Dakin SC, Allen HA (May 2006). "Integration of local motion is normal in amblyopia". Journal of the Optical Society of America A. 23 (5): 986–92. Bibcode:2006JOSAA..23..986H. doi:10.1364/JOSAA.23.000986. PMID 16642175.
- Polat U, Ma-Naim T, Belkin M, Sagi D (April 2004). "Improving vision in adult amblyopia by perceptual learning". Proceedings of the National Academy of Sciences of the United States of America. 101 (17): 6692–7. Bibcode:2004PNAS..101.6692P. doi:10.1073/pnas.0401200101. PMC 404107. PMID 15096608.
- Levi, Dennis M.; Song, Shuang; Pelli, Denis G. (2007). "Amblyopic reading is crowded". Journal of Vision. 7 (2): 21.1–17. doi:10.1167/7.2.21. ISSN 1534-7362. PMID 18217836.
- Simons K (2005). "Amblyopia characterization, treatment, and prophylaxis". Survey of Ophthalmology. 50 (2): 123–66. doi:10.1016/j.survophthal.2004.12.005. PMID 15749306.
- Tyler CW (2004). Tasman W, Jaeger EA (eds.). Binocular Vision In, Duane's Foundations of Clinical Ophthalmology. Vol. 2. Philadelphia: J.B. Lippincott Co.
- Mohammadpour, M; Shaabani, A; Sahraian, A; Momenaei, B; Tayebi, F; Bayat, R; Mirshahi, R (June 2019). "Updates on managements of pediatric cataract". Journal of Current Ophthalmology. 31 (2): 118–126. doi:10.1016/j.joco.2018.11.005. PMC 6611931. PMID 31317088.
- Wright KW, Spiegel PH, Thompson LS (2006). Handbook of Pediatric Strabismus and Amblyopia. New York, New York: Springer. ISBN 978-0-387-27924-4.
- Levi DM (March 2006). "Visual processing in amblyopia: human studies". Strabismus. 14 (1): 11–9. doi:10.1080/09273970500536243. PMID 16513566. S2CID 29190763.
- Tychsen L (August 2012). "The cause of infantile strabismus lies upstairs in the cerebral cortex, not downstairs in the brainstem". Archives of Ophthalmology. 130 (8): 1060–1. doi:10.1001/archophthalmol.2012.1481. PMID 22893080.
- Kanonidou E, Gottlob I, Proudlock FA (January 2014). "The effect of font size on reading performance in strabismic amblyopia: an eye movement investigation". Investigative Ophthalmology & Visual Science. 55 (1): 451–9. doi:10.1167/iovs.13-13257. PMID 24370829.
- Kanonidou E, Proudlock FA, Gottlob I (July 2010). "Reading strategies in mild to moderate strabismic amblyopia: an eye movement investigation". Investigative Ophthalmology & Visual Science. 51 (7): 3502–8. doi:10.1167/iovs.09-4236. PMID 20207968.
- Holmes JM, Repka MX, Kraker RT, Clarke MP (March 2006). "The treatment of amblyopia". Strabismus. 14 (1): 37–42. doi:10.1080/09273970500536227. PMID 16513568. S2CID 31165871.
- Rutstein RF, Corliss D (April 1999). "Relationship between Anisometropia, Amblyopia, and Binocularity". Optometry & Vision Science. 76 (4): 229–33. doi:10.1097/00006324-199904000-00026. PMID 10333185.
- Weakley DR (January 2001). "The association between nonstrabismic anisometropia, amblyopia, and subnormal binocularity". Ophthalmology. 108 (1): 163–71. doi:10.1016/s0161-6420(00)00425-5. PMID 11150283.
- Simon JW, Kaw P (August 2001). "Commonly missed diagnoses in the childhood eye examination". American Family Physician. 64 (4): 623–8. PMID 11529261. Archived from the original on 12 September 2005. Retrieved 28 August 2005.
- Astle WF, Rahmat J, Ingram AD, Huang PT (December 2007). "Laser-assisted subepithelial keratectomy for anisometropic amblyopia in children: outcomes at 1 year". Journal of Cataract and Refractive Surgery. 33 (12): 2028–34. doi:10.1016/j.jcrs.2007.07.024. PMID 18053899. S2CID 1886316.
- Angell LK, Robb RM, Berson FG (December 1981). "Visual prognosis in patients with ruptures in Descemet's membrane due to forceps injuries". Archives of Ophthalmology. 99 (12): 2137–9. doi:10.1001/archopht.1981.03930021013004. PMID 7305711.
- Antonio-Santos, Aileen; Vedula, S. Swaroop; Hatt, Sarah R.; Powell, Christine (23 March 2020). "Occlusion for stimulus deprivation amblyopia". The Cochrane Database of Systematic Reviews. 3: CD005136. doi:10.1002/14651858.CD005136.pub4. ISSN 1469-493X. PMC 7089638. PMID 32203629.
- McKee SP, Levi DM, Movshon JA (2003). "The pattern of visual deficits in amblyopia". Journal of Vision. 3 (5): 380–405. doi:10.1167/3.5.5. PMID 12875634.
- Cooper J, Cooper R. "All About Strabismus". Optometrists Network. Retrieved 9 March 2008.
- Wright WK (2006). Handbook of Pediatric Strabismus and Amblyopia. New-York: Springer. pp. 103–137.
- Schiefer U, Wilhelm H, Hart W (11 September 2007). Clinical Neuro-Ophthalmology: A Practical Guide. Springer Science & Business Media. p. 16. ISBN 978-3-540-32708-0. Archived from the original on 8 September 2017.
- Grossman DC, Curry SJ, Owens DK, Barry MJ, Davidson KW, Doubeni CA, et al. (September 2017). "Vision Screening in Children Aged 6 Months to 5 Years: US Preventive Services Task Force Recommendation Statement". JAMA. 318 (9): 836–844. doi:10.1001/jama.2017.11260. PMID 28873168. S2CID 205084845.
- Coats DK and Paysse EA. Overview of amblyopia UpToDate. Last updated: Sep 25, 2014
- "A patch or eye drops are similarly effective for the treatment of "lazy eye" in children". NIHR Evidence (Plain English summary). National Institute for Health and Care Research. 5 December 2019. doi:10.3310/signal-000849. S2CID 243130859.
- Li T, Qureshi R, Taylor K (2019). "Conventional occlusion versus pharmacologic penalization for amblyopia". Cochrane Database Syst Rev. 8 (8): CD006460. doi:10.1002/14651858.CD006460.pub3. PMC 6713317. PMID 31461545.
- Amblyopia NEI Health Information Archived 11 September 2005 at the Wayback Machine
- Cunningham ET, Riordan-Eva P (17 May 2011). Vaughan & Asbury's general ophthalmology (18th ed.). McGraw-Hill Medical. ISBN 978-0071634205.
- Williams C, Northstone K, Harrad RA, Sparrow JM, Harvey I (June 2002). "Amblyopia treatment outcomes after screening before or at age 3 years: follow up from randomised trial". BMJ. 324 (7353): 1549. doi:10.1136/bmj.324.7353.1549. PMC 116606. PMID 12089090.
- "App auf Rezept: Barmer bezahlt internetbasierte Behandlung" [Prescription app: Barmer pays for internet-based treatment]. www.aerztezeitung.de (in German). 28 March 2014. Archived from the original on 29 March 2014. Retrieved 29 March 2014.
- West, S; Williams, C (30 June 2011). "Amblyopia". BMJ Clinical Evidence. 2011. PMC 3275294. PMID 21714945.
- Zhou Y, Huang C, Xu P, Tao L, Qiu Z, Li X, Lu ZL (March 2006). "Perceptual learning improves contrast sensitivity and visual acuity in adults with anisometropic amblyopia". Vision Research. 46 (5): 739–50. doi:10.1016/j.visres.2005.07.031. PMID 16153674. S2CID 1290214.
- Astle AT, Webb BS, McGraw PV (November 2011). "Can perceptual learning be used to treat amblyopia beyond the critical period of visual development?". Ophthalmic & Physiological Optics. 31 (6): 564–73. doi:10.1111/j.1475-1313.2011.00873.x. PMC 3428831. PMID 21981034.
- Levi DM (June 2012). "Prentice award lecture 2011: removing the brakes on plasticity in the amblyopic brain". Optometry and Vision Science. 89 (6): 827–38. doi:10.1097/OPX.0b013e318257a187. PMC 3369432. PMID 22581119.
- Elflein HM, Fresenius S, Lamparter J, Pitz S, Pfeiffer N, Binder H, Wild P, Mirshahi A (May 2015). "The prevalence of amblyopia in Germany: data from the prospective, population-based Gutenberg Health Study". Deutsches Ärzteblatt International. 112 (19): 338–44. doi:10.3238/arztebl.2015.0338. PMC 4458790. PMID 26043421.
- Stewart CE, Fielder AR, Stephens DA, Moseley MJ (August 2002). "Design of the Monitored Occlusion Treatment of Amblyopia Study (MOTAS)". The British Journal of Ophthalmology. 86 (8): 915–9. doi:10.1136/bjo.86.8.915. PMC 1771248. PMID 12140215.
- Birch EE (March 2013). "Amblyopia and binocular vision". Progress in Retinal and Eye Research. 33: 67–84. doi:10.1016/j.preteyeres.2012.11.001. PMC 3577063. PMID 23201436.
- Thompson B, Mansouri B, Koski L, Hess RF (July 2008). "Brain plasticity in the adult: modulation of function in amblyopia with rTMS". Current Biology. 18 (14): 1067–71. doi:10.1016/j.cub.2008.06.052. PMID 18635353. S2CID 14808576.
- Seabrook A. "Magnetic Pulses To Brain Help 'Lazy Eye'". National Public Radio. Archived from the original on 8 January 2009.
- Hess RF, Thompson B (February 2013). "New insights into amblyopia: binocular therapy and noninvasive brain stimulation". Journal of AAPOS. 17 (1): 89–93. doi:10.1016/j.jaapos.2012.10.018. PMID 23352385.
- Hess RF, Thompson B, Baker DH (March 2014). "Binocular vision in amblyopia: structure, suppression and plasticity" (PDF). Ophthalmic & Physiological Optics. 34 (2): 146–62. doi:10.1111/opo.12123. PMID 24588532. S2CID 22584125.
- Spiegel DP, Byblow WD, Hess RF, Thompson B (October 2013). "Anodal transcranial direct current stimulation transiently improves contrast sensitivity and normalizes visual cortex activation in individuals with amblyopia". Neurorehabilitation and Neural Repair. 27 (8): 760–9. doi:10.1177/1545968313491006. PMID 23774122. S2CID 38437179.
- Clavagnier S, Thompson B, Hess RF (November 2013). "Long lasting effects of daily theta burst rTMS sessions in the human amblyopic cortex". Brain Stimulation. 6 (6): 860–7. doi:10.1016/j.brs.2013.04.002. PMID 23664756. S2CID 36592293.
- Birch EE (March 2013). "Amblyopia and binocular vision". Progress in Retinal and Eye Research (Review). 33: 67–84. doi:10.1016/j.preteyeres.2012.11.001. PMC 3577063. PMID 23201436.
- Li J, Thompson B, Deng D, Chan LY, Yu M, Hess RF (April 2013). "Dichoptic training enables the adult amblyopic brain to learn". Current Biology. 23 (8): R308-9. doi:10.1016/j.cub.2013.01.059. PMID 23618662.
- Nordqvist J (23 April 2013). "Tetris Video Game Helps Treat Lazy Eye". Medical News Today (MNT). Archived from the original on 29 May 2013.
- Spiegel DP, Li J, Hess RF, Byblow WD, Deng D, Yu M, Thompson B (October 2013). "Transcranial direct current stimulation enhances recovery of stereopsis in adults with amblyopia". Neurotherapeutics. 10 (4): 831–9. doi:10.1007/s13311-013-0200-y. PMC 3805870. PMID 23857313.
Further reading
- Birch EE (March 2013). "Amblyopia and binocular vision". Progress in Retinal and Eye Research (review). 33: 67–84. doi:10.1016/j.preteyeres.2012.11.001. PMC 3577063. PMID 23201436.
- Daw, Nigel W. (2014). Visual Development (Third ed.). Springer. ISBN 978-1461490586.
- Chapter What is Amblyopia? pp. 123–145, doi:10.1007/978-1-4614-9059-3_8,
- Chapter Treatment of Amblyopia pp. 167–180, doi:10.1007/978-1-4614-9059-3_10.
- Stewart CE, Moseley MJ, Fielder AR (September 2011). "Amblyopia therapy: an update". Strabismus. 19 (3): 91–8. doi:10.3109/09273972.2011.600421. PMID 21870912. S2CID 38988992.
- Sengpiel F (September 2014). "Plasticity of the visual cortex and treatment of amblyopia". Current Biology (review). 24 (18): R936–R940. doi:10.1016/j.cub.2014.05.063. PMID 25247373.
- Hamm LM, Black J, Dai S, Thompson B (2014). "Global processing in amblyopia: a review". Frontiers in Psychology (review). 5: 583. doi:10.3389/fpsyg.2014.00583. PMC 4060804. PMID 24987383.
External links
- National Eye Institute (NEI) Resource Guide
- Lazy Eye Site from the National Health Service, UK
- Look After Your Eyes - patient information on Amblyopia or 'lazy eye' by College of Optometrists