Anticonvulsant
Anticonvulsants (also known as antiepileptic drugs or recently as antiseizure drugs) are a diverse group of pharmacological agents used in the treatment of epileptic seizures.[1] Anticonvulsants are also increasingly being used in the treatment of bipolar disorder[2][3] and borderline personality disorder,[4] since many seem to act as mood stabilizers, and for the treatment of neuropathic pain.[5] Anticonvulsants suppress the excessive rapid firing of neurons during seizures.[6] Anticonvulsants also prevent the spread of the seizure within the brain.[7]
| Anticonvulsant | |
|---|---|
| Drug class | |
| Class identifiers | |
| Synonyms | Antiepileptic drugs, antiseizure drugs |
| Use | Epilepsy |
| ATC code | N03 |
| Biological target | Brain |
| In Wikidata | |
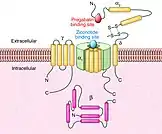
Conventional antiepileptic drugs may block sodium channels or enhance γ-aminobutyric acid (GABA) function. Several antiepileptic drugs have multiple or uncertain mechanisms of action.[8] Next to the voltage-gated sodium channels and components of the GABA system, their targets include GABAA receptors, the GAT-1 GABA transporter, and GABA transaminase.[9] Additional targets include voltage-gated calcium channels, SV2A, and α2δ.[10][11] By blocking sodium or calcium channels, antiepileptic drugs reduce the release of excitatory glutamate, whose release is considered to be elevated in epilepsy, but also that of GABA.[12] This is probably a side effect or even the actual mechanism of action for some antiepileptic drugs, since GABA can itself, directly or indirectly, act proconvulsively.[12] Another potential target of antiepileptic drugs is the peroxisome proliferator-activated receptor alpha.[13][14][15][16][17][18][19]
Some anticonvulsants have shown antiepileptogenic effects in animal models of epilepsy.[20] That is, they either prevent the development of epilepsy or can halt or reverse the progression of epilepsy. However, no drug has been shown in human trials to prevent epileptogenesis (the development of epilepsy in an individual at risk, such as after a head injury).[21]
Terminology
Anticonvulsants are more accurately called antiepileptic drugs (abbreviated "AEDs"), and are often referred to as antiseizure drugs because they provide symptomatic treatment only and have not been demonstrated to alter the course of epilepsy.
Approval
The usual method of achieving approval for a drug is to show it is effective when compared against placebo, or that it is more effective than an existing drug. In monotherapy (where only one drug is taken) it is considered unethical by most to conduct a trial with placebo on a new drug of uncertain efficacy. This is because untreated epilepsy leaves the patient at significant risk of death. Therefore, almost all new epilepsy drugs are initially approved only as adjunctive (add-on) therapies. Patients whose epilepsy is currently uncontrolled by their medication (i.e., it is refractory to treatment) are selected to see if supplementing the medication with the new drug leads to an improvement in seizure control. Any reduction in the frequency of seizures is compared against a placebo.[21] The lack of superiority over existing treatment, combined with lacking placebo-controlled trials, means that few modern drugs have earned FDA approval as initial monotherapy. In contrast, Europe only requires equivalence to existing treatments and has approved many more. Despite their lack of FDA approval, the American Academy of Neurology and the American Epilepsy Society still recommend a number of these new drugs as initial monotherapy.[21]
Drugs
In the following list, the dates in parentheses are the earliest approved use of the drug.
Aldehydes
- Paraldehyde (1882). One of the earliest anticonvulsants. It is still used to treat status epilepticus, particularly where there are no resuscitation facilities.[22][23]
Aromatic allylic alcohols
Barbiturates
Barbiturates are drugs that act as central nervous system (CNS) depressants, and by virtue of this they produce a wide spectrum of effects, from mild sedation to anesthesia. The following are classified as anticonvulsants:
- Phenobarbital (1912). See also the related drug primidone.
- Methylphenobarbital (1935). Known as mephobarbital in the US. No longer marketed in the UK.
- Barbexaclone (1982). Only available in some European countries.
Phenobarbital was the main anticonvulsant from 1912 until the development of phenytoin in 1938. Today, phenobarbital is rarely used to treat epilepsy in new patients since there are other effective drugs that are less sedating. Phenobarbital sodium injection can be used to stop acute convulsions or status epilepticus, but a benzodiazepine such as lorazepam, diazepam or midazolam is usually tried first. Other barbiturates only have an anticonvulsant effect at anaesthetic doses.
Benzodiazepines
The benzodiazepines are a class of drugs with hypnotic, anxiolytic, anticonvulsive, amnestic and muscle relaxant properties. Benzodiazepines act as a central nervous system depressant. The relative strength of each of these properties in any given benzodiazepine varies greatly and influences the indications for which it is prescribed. Long-term use can be problematic due to the development of tolerance to the anticonvulsant effects and dependency.[28][29][30][31] Of many drugs in this class, only a few are used to treat epilepsy:
- Clobazam (1979). Notably, used on a short-term basis around menstruation in women with catamenial epilepsy.
- Clonazepam (1974).
- Clorazepate (1972).
The following benzodiazepines are used to treat status epilepticus:
- Diazepam (1963). Can be given rectally by trained care-givers.
- Midazolam (N/A). Increasingly being used as an alternative to diazepam. This water-soluble drug is squirted into the side of the mouth but not swallowed. It is rapidly absorbed by the buccal mucosa.
- Lorazepam (1972). Given by injection in hospital.
Nitrazepam, temazepam, and especially nimetazepam are powerful anticonvulsant agents, however their use is rare due to an increased incidence of side effects and strong sedative and motor-impairing properties.
Bromides
- Potassium bromide (1857). The earliest effective treatment for epilepsy. There would not be a better drug until phenobarbital in 1912. It is still used as an anticonvulsant for dogs and cats but is no longer used in humans.
Carbamates
Carboxamides

The following are carboxamides:
- Carbamazepine (1963). A popular anticonvulsant that is available in generic formulations.
- Oxcarbazepine (1990). A derivative of carbamazepine that has similar efficacy and is better tolerated and is also available generically.
- Eslicarbazepine acetate (2009).
Fatty acids
The following are fatty-acids:
- The valproates — valproic acid, sodium valproate, and divalproex sodium (1967).
- Vigabatrin (1989).
- Progabide (1987).
- Tiagabine (1996).
Vigabatrin and progabide are also analogs of GABA.
Fructose derivatives
- Topiramate (1995).
Gabapentinoids
Gabapentinoids are used in, epilepsy, neuropathic pain, fibromyalgia, restless leg syndrome, opioid withdrawal and generalized anxiety disorder (GAD). Gabapentinoids block Voltage gated Calcium channels, mainly the N-Type, and P/Q type calcium channels. The following are Gabapentinoids:
- Pregabalin (2004)
- Mirogabalin (2019) (Japan only)
- Gabapentin (1993)
- Gabapentin Encarbil (2011).
- Gabapentin Extended Release (Gralise) (1996).
Gabapentinoids are analogs of GABA, but they do not act on GABA. They have analgesic anticonvulsant and anxiolytic effects.
Hydantoins
The following are hydantoins:
- Ethotoin (1957).
- Phenytoin (1938).
- Mephenytoin.
- Fosphenytoin (1996).
Oxazolidinediones
The following are oxazolidinediones:
- Paramethadione.
- Trimethadione (1946).
- Ethadione.
Propionates
- Beclamide.
Pyrimidinediones
- Primidone (1952).
Pyrrolidines
- Brivaracetam (2016).
- Etiracetam.
- Levetiracetam (1999).
- Seletracetam.
Sulfonamides
- Acetazolamide (1953).
- Sultiame.
- Methazolamide.
- Zonisamide (2000).
Triazines
- Lamotrigine (1990).
Ureas
- Pheneturide.
- Phenacemide.
Valproylamides
- Valpromide.
- Valnoctamide.
Other
- Perampanel.
- Stiripentol.[26]
- Pyridoxine (1939).
Non-pharmaceutical anticonvulsants
The ketogenic diet and vagus nerve stimulation are alternative treatments for epilepsy without the involvement of pharmaceuticals. However, both of them can cause severe adverse effects. The adverse effects of vagus nerve stimulation are more severe, and its efficacy is questionable in comparison to medications or the ketogenic diet.
Treatment guidelines
According to guidelines by the American Academy of Neurology and American Epilepsy Society,[35] mainly based on a major article review in 2004,[36] patients with newly diagnosed epilepsy who require treatment can be initiated on standard anticonvulsants such as carbamazepine, phenytoin, valproic acid/valproate semisodium, phenobarbital, or on the newer anticonvulsants gabapentin, lamotrigine, oxcarbazepine or topiramate. The choice of anticonvulsants depends on individual patient characteristics.[35] Both newer and older drugs are generally equally effective in new onset epilepsy.[35] The newer drugs tend to have fewer side effects.[35] For newly diagnosed partial or mixed seizures, there is evidence for using gabapentin, lamotrigine, oxcarbazepine or topiramate as monotherapy.[35] Lamotrigine can be included in the options for children with newly diagnosed absence seizures.[35]
History
The first anticonvulsant was bromide, suggested in 1857 by the British gynecologist Charles Locock who used it to treat women with "hysterical epilepsy" (probably catamenial epilepsy). Bromides are effective against epilepsy, and also cause impotence, which is not related to its anti-epileptic effects. Bromide also suffered from the way it affected behaviour, introducing the idea of the "epileptic personality" which was actually a result of medication. Phenobarbital was first used in 1912 for both its sedative and antiepileptic properties. By the 1930s, the development of animal models in epilepsy research led to the development of phenytoin by Tracy Putnam and H. Houston Merritt, which had the distinct advantage of treating epileptic seizures with less sedation.[37] By the 1970s, a National Institutes of Health initiative, the Anticonvulsant Screening Program, headed by J. Kiffin Penry, served as a mechanism for drawing the interest and abilities of pharmaceutical companies in the development of new anticonvulsant medications.
Marketing approval history
The following table lists anticonvulsant drugs together with the date their marketing was approved in the US, UK and France. Data for the UK and France are incomplete. In recent years, the European Medicines Agency has approved drugs throughout the European Union. Some of the drugs are no longer marketed.
| Drug | Brand | US | UK | France |
|---|---|---|---|---|
| acetazolamide | Diamox | 27 July 1953[38] | 1988[39] | |
| brivaracetam | Briviact | 18 February 2016[40][41] | ||
| carbamazepine | Tegretol | 15 July 1974[42][43] | 1965[39] | 1963[44] |
| cenobamate | Xcopri | 21 November 2019 | ||
| clobazam | Onfi/Frisium | 21 October 2011[45][46] | 1979[39] | |
| clonazepam | Klonopin/Rivotril | 4 June 1975[47] | 1974[39] | |
| diazepam | Valium | 15 November 1963[48] | ||
| divalproex sodium | Depakote | 10 March 1983[49] | ||
| eslicarbazepine | Aptiom | 11 August 2013[50][51] | ||
| ethosuximide | Zarontin | 2 November 1960[52] | 1955[39] | 1962[44] |
| ethotoin | Peganone | 22 April 1957[53] | ||
| everolimus | Afinitor/Votubia | 30 January 2009[54] | ||
| felbamate | Felbatol | 29 July 1993[55] | ||
| fosphenytoin | Cerebyx | 5 August 1996[56] | ||
| gabapentin | Neurontin | 30 December 1993[57] | May 1993[39][44] | October 1994[44] |
| lacosamide | Vimpat | 28 October 2008[58] | ||
| lamotrigine | Lamictal | 27 December 1994[59] | October 1991[39][44] | May 1995[44] |
| levetiracetam | Keppra | 30 November 1999[60] | 29 September 2000[39][61] | 29 September 2000[61] |
| mephenytoin | Mesantoin | 23 October 1946[62] | ||
| metharbital | Gemonil | 1952[63][64] | ||
| methsuximide | Celontin | 8 February 1957[65] | ||
| methazolamide | Neptazane | 26 January 1959[66] | ||
| oxcarbazepine | Trileptal | 14 January 2000[67] | 2000[39] | |
| phenobarbital | 1912[39] | 1920[44] | ||
| phenytoin | Dilantin/Epanutin | 1938[44][68] | 1938[39] | 1941[44] |
| piracetam | Nootropil | Data needed | ||
| phensuximide | Milontin | 1953[69][70] | ||
| pregabalin | Lyrica | 30 December 2004[71] | 6 July 2004[39][72] | 6 July 2004[72] |
| primidone | Mysoline | 8 March 1954[73] | 1952[39] | 1953[44] |
| rufinamide | Banzel/Inovelon | 14 November 2008[74][75] | ||
| sodium valproate | Epilim | December 1977[44] | June 1967[44] | |
| stiripentol | Diacomit | 20 August 2018[76][77] | January 2007[26] | January 2007[26] |
| tiagabine | Gabitril | 30 September 1997[78][79] | 1998[39] | November 1997[44] |
| topiramate | Topamax | 24 December 1996[80] | 1995[39] | |
| trimethadione | Tridione | 25 January 1946[81] | ||
| valproic acid | Depakene/Convulex | 28 February 1978[82] | 1993[39] | |
| vigabatrin | Sabril | 21 August 2009[83] | 1989[39] | |
| zonisamide | Zonegran | 27 March 2000[84] | 10 March 2005[39][85] | 10 March 2005[85] |
Pregnancy
During pregnancy, the metabolism of several anticonvulsants is affected. There may be an increase in the clearance and resultant decrease in the blood concentration of lamotrigine, phenytoin, and to a lesser extent carbamazepine, and possibly decreases the level of levetiracetam and the active oxcarbazepine metabolite, the monohydroxy derivative.[86] Therefore, these drugs should be monitored during use in pregnancy.[86]
Many of the common used medications, such as valproate, phenytoin, carbamazepine, phenobarbitol, gabapentin have been reported to cause increased risk of birth defects.[87] Among anticonvulsants, levetiracetam and lamotrigine seem to carry the lowest risk of causing birth defects. The risk of untreated epilepsy is believed to be greater than the risk of adverse effects caused by these medications, necessitating continuation of antiepileptic treatment.
Valproic acid, and its derivatives such as sodium valproate and divalproex sodium, causes cognitive deficit in the child, with an increased dose causing decreased intelligence quotient.[88] On the other hand, evidence is conflicting for carbamazepine regarding any increased risk of congenital physical anomalies or neurodevelopmental disorders by intrauterine exposure.[88] Similarly, children exposed lamotrigine or phenytoin in the womb do not seem to differ in their skills compared to those who were exposed to carbamazepine.[88]
There is inadequate evidence to determine if newborns of women with epilepsy taking anticonvulsants have a substantially increased risk of hemorrhagic disease of the newborn.[86]
Regarding breastfeeding, some anticonvulsants probably pass into breast milk in clinically significant amounts, including primidone and levetiracetam.[86] On the other hand, valproate, phenobarbital, phenytoin, and carbamazepine probably are not transferred into breast milk in clinically important amounts.[86]
Data from studies conducted on women taking antiepileptic drugs for non-epileptic reasons, including depression and bipolar disorder, show that if high doses of the drugs are taken during the first trimester of pregnancy then there is the potential of an increased risk of congenital malformations.[89]
Pregnancy planning is being explored as a method that could decrease the risk of possible birth defects. Since the first trimester is the most susceptible period for fetal development, planning a routine antiepileptic drug dose that is safer for the first trimester could be beneficial to prevent pregnancy complications.[90]
In animal models, several anticonvulsant drugs have been demonstrated to induce neuronal apoptosis in the developing brain.[91][92][93][94][95]
References
- Al-Otaibi, Faisal (1 September 2019). "An overview of structurally diversified anticonvulsant agents". Acta Pharmaceutica (Zagreb, Croatia). Walter de Gruyter GmbH. 69 (3): 321–344. doi:10.2478/acph-2019-0023. ISSN 1846-9558. PMID 31259739.
- Joshi, A; Bow, A; Agius, M (2019). "Pharmacological Therapies in Bipolar Disorder: a Review of Current Treatment Options". Psychiatria Danubina. 31 (Suppl 3): 595–603. ISSN 0353-5053. PMID 31488797.
- Keck, Paul E. Jr.; McElroy, Susan L.; Strakowski, Stephen M. (1998). "Anticonvulsants and antipsychotics in the treatment of bipolar disorder". The Journal of Clinical Psychiatry. 59 (Suppl 6): 74–82. PMID 9674940.
- American Psychiatric Association, and American Psychiatric Association. Work Group on Borderline Personality Disorder. Practice guideline for the treatment of patients with borderline personality disorder. American Psychiatric Pub, 2001.
- Rogawski, Michael A.; Löscher, Wolfgang (2004). "The neurobiology of antiepileptic drugs". Nature Reviews Neuroscience. 5 (7): 553–564. doi:10.1038/nrn1430. PMID 15208697. S2CID 2201038.
- McLean, M J; Macdonald, R L (June 1986). "Sodium valproate, but not ethosuximide, produces use- and voltage-dependent limitation of high frequency repetitive firing of action potentials of mouse central neurons in cell culture". Journal of Pharmacology and Experimental Therapeutics. 237 (3): 1001–1011. PMID 3086538.
- Harden, C. L. (1 May 1994). "New antiepileptic drugs". Neurology. 44 (5): 787–95. doi:10.1212/WNL.44.5.787. PMID 8190276. S2CID 75925846.
- "Archived copy" (PDF). Archived from the original (PDF) on 3 November 2013. Retrieved 28 January 2013.
{{cite web}}: CS1 maint: archived copy as title (link) - Rogawski MA, Löscher W (July 2004). "The neurobiology of antiepileptic drugs". Nature Reviews Neuroscience. 5 (7): 553–64. doi:10.1038/nrn1430. PMID 15208697. S2CID 2201038.
- Rogawski MA, Bazil CW (July 2008). "New molecular targets for antiepileptic drugs: alpha(2)delta, SV2A, and K(v)7/KCNQ/M potassium channels". Curr Neurol Neurosci Rep. 8 (4): 345–52. doi:10.1007/s11910-008-0053-7. PMC 2587091. PMID 18590620.
- Meldrum BS, Rogawski MA (January 2007). "Molecular targets for antiepileptic drug development". Neurotherapeutics. 4 (1): 18–61. doi:10.1016/j.nurt.2006.11.010. PMC 1852436. PMID 17199015.
- Kammerer, M.; Rassner, M. P.; Freiman, T. M.; Feuerstein, T. J. (2 May 2011). "Effects of antiepileptic drugs on GABA release from rat and human neocortical synaptosomes". Naunyn-Schmiedeberg's Archives of Pharmacology. 384 (1): 47–57. doi:10.1007/s00210-011-0636-8. PMID 21533993. S2CID 1388805.
- Puligheddu M, Pillolla G, Melis M, Lecca S, Marrosu F, De Montis MG, et al. (2013). Charpier S (ed.). "PPAR-alpha agonists as novel antiepileptic drugs: preclinical findings". PLOS ONE. 8 (5): e64541. Bibcode:2013PLoSO...864541P. doi:10.1371/journal.pone.0064541. PMC 3664607. PMID 23724059.
- Citraro R, et al. (2013). "Antiepileptic action of N-palmitoylethanolamine through CB1 and PPAR-α receptor activation in a genetic model of absence epilepsy". Neuropharmacology. 69: 115–26. doi:10.1016/j.neuropharm.2012.11.017. PMID 23206503. S2CID 27701532.
- Porta, N.; Vallée, L.; Lecointe, C.; Bouchaert, E.; Staels, B.; Bordet, R.; Auvin, S. (2009). "Fenofibrate, a peroxisome proliferator-activated receptor-alpha agonist, exerts anticonvulsive properties". Epilepsia. 50 (4): 943–8. doi:10.1111/j.1528-1167.2008.01901.x. PMID 19054409. S2CID 6796135.
- Lampen A, Carlberg C, Nau H (2001). "Peroxisome proliferator-activated receptor delta is a specific sensor for teratogenic valproic acid derivatives". Eur J Pharmacol. 431 (1): 25–33. doi:10.1016/S0014-2999(01)01423-6. PMID 11716839.
- Maguire JH, Murthy AR, Hall IH (1985). "Hypolipidemic activity of antiepileptic 5-phenylhydantoins in mice". Eur J Pharmacol. 117 (1): 135–8. doi:10.1016/0014-2999(85)90483-2. PMID 4085542.
- Hall IH, Patrick MA, Maguire JH (1990). "Hypolipidemic activity in rodents of phenobarbital and related derivatives". Archiv der Pharmazie. 323 (9): 579–86. doi:10.1002/ardp.19903230905. PMID 2288480. S2CID 46002731.
- Frigerio F, Chaffard G, Berwaer M, Maechler P (2006). "The antiepileptic drug topiramate preserves metabolism-secretion coupling in insulin secreting cells chronically exposed to the fatty acid oleate". Biochem Pharmacol. 72 (8): 965–73. doi:10.1016/j.bcp.2006.07.013. PMID 16934763.
- Kaminski, R. M.; Rogawski, M. A.; Klitgaard, H (2014). "The potential of antiseizure drugs and agents that act on novel molecular targets as antiepileptogenic treatments". Neurotherapeutics. 11 (2): 385–400. doi:10.1007/s13311-014-0266-1. PMC 3996125. PMID 24671870.
- Abou-Khalil BW (2007). "Comparative Monotherapy Trials and the Clinical Treatment of Epilepsy". Epilepsy Currents. 7 (5): 127–9. doi:10.1111/j.1535-7511.2007.00198.x. PMC 2043140. PMID 17998971.
- Browne TR. Paraldehyde, chlormethiazole, and lidocaine for treatment of status epilepticus. In: Delgado-Escueta AV, Wasterlain CG, Treiman DM, Porter RJ, eds. Status Epilepticus. Mechanisms of Brain Damage and Treatment (Advances in Neurology, Vol 34). New York, Raven Press 1983: 509–517
- Ramsay RE (1989). "Pharmacokinetics and clinical use of parenteral phenytoin, phenobarbital, and paraldehyde". Epilepsia. 30 (Suppl 2): S1–S3. doi:10.1111/j.1528-1157.1989.tb05818.x. PMID 2767008. S2CID 44798815.
- Plosker, GL (November 2012). "Stiripentol : in severe myoclonic epilepsy of infancy (dravet syndrome)". CNS Drugs. 26 (11): 993–1001. doi:10.1007/s40263-012-0004-3. PMID 23018548.
- "Public summary of positive opinion for orpphan opinion for orphan designation of stiripentol for the treatment of severe myoclonic epilepsy in infancy" (PDF). European Medicines Agency. 30 July 2007. Retrieved 19 May 2013.
Doc.Ref.: EMEA/COMP/269/04
- "Diacomit EPAR". European Medicines Agency. Retrieved 8 November 2020.
- "Diacomit- stiripentol capsule Diacomit- stiripentol powder, for suspension". DailyMed. 15 May 2020. Retrieved 8 November 2020.
- Browne TR (May 1976). "Clonazepam. A review of a new anticonvulsant drug". Arch Neurol. 33 (5): 326–32. doi:10.1001/archneur.1976.00500050012003. PMID 817697.
- Isojärvi, JI; Tokola RA (December 1998). "Benzodiazepines in the treatment of epilepsy in people with intellectual disability". J Intellect Disabil Res. 42 (1): 80–92. PMID 10030438.
- Tomson, T; Svanborg, E; Wedlund, JE (May–June 1986). "Nonconvulsive status epilepticus". Epilepsia. 27 (3): 276–85. doi:10.1111/j.1528-1157.1986.tb03540.x. PMID 3698940. S2CID 26694857.
- Djurić, M; Marjanović B; Zamurović D (May–June 2001). "[West syndrome--new therapeutic approach]". Srp Arh Celok Lek. 129 (1): 72–7. PMID 15637997.
- Sankar, editors John M. Pellock, Blaise F.D. Bourgeois, W. Edwin Dodson; associate editors, Douglas R. Nordli, Jr., Raman (2008). Pediatric epilepsy : diagnosis and therapy (3rd ed., updated and new. ed.). New York: Demos Medical Pub. ISBN 978-1-933864-16-7.
{{cite book}}:|first=has generic name (help) - French, J; Smith, M; Faught, E; Brown, L (12 May 1999). "Practice advisory: The use of felbamate in the treatment of patients with intractable epilepsy: report of the Quality Standards Subcommittee of the American Academy of Neurology and the American Epilepsy Society". Neurology. 52 (8): 1540–5. doi:10.1212/WNL.52.8.1540. PMID 10331676.
- "Felbamate". MedlinePlus : U.S. National Library of Medicine. Retrieved 19 May 2013.
- AAN Guideline Summary for Clinicians – Efficacy and Tolerability of the New Antiepileptic Drugs, I: Treatment of New Onset Epilepsy Archived 24 February 2011 at the Wayback Machine Retrieved on 29 June 2010
- French JA, Kanner AM, Bautista J, et al. (May 2004). "Efficacy and tolerability of the new antiepileptic drugs, I: Treatment of new-onset epilepsy: report of the TTA and QSS Subcommittees of the American Academy of Neurology and the American Epilepsy Society" (PDF). Epilepsia. 45 (5): 401–9. doi:10.1111/j.0013-9580.2004.06204.x. hdl:2027.42/65231. PMID 15101821. S2CID 12259676.
- Eadie MJ, Bladin PF (2001). "A Disease Once Sacred: a History of the Medical Understanding of Epilepsy".
{{cite journal}}: Cite journal requires|journal=(help) - "New Drug Application (NDA) 008943". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- Epilepsy Action: Druglist. Retrieved on 1 November 2007.
- "New Drug Application (NDA) 205836". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "Drug Approval Package: Briviact (brivaracetam)". U.S. Food and Drug Administration (FDA). 30 March 2016. Archived from the original on 22 November 2019. Retrieved 21 November 2019.
- "New Drug Application (NDA) 016608". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019. (Initial approval on 11 March 1968 was for trigeminal neuralgia.)
- Schain, Richard J. (1 March 1978). "Pediatrics—Epitomes of Progress: Carbamazepine (Tegretol) in the Treatment of Epilepsy". Western Journal of Medicine. 128 (3): 231–232. PMC 1238063. PMID 18748164.
- Loiseau, Pierre Jean-Marie (June 1999). "Clinical Experience with New Antiepileptic Drugs: Antiepileptic Drugs in Europe". Epilepsia. 40 (Suppl 6): S3–8. doi:10.1111/j.1528-1157.1999.tb00925.x. PMID 10530675. S2CID 29638422.
- "New Drug Application (NDA) 202067". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "Drug Approval Package: Onfi NDA #202067". U.S. Food and Drug Administration (FDA). 20 August 2013. Archived from the original on 22 November 2019. Retrieved 21 November 2019.
- "New Drug Application (NDA) 017533". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 013263". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 018723". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 022416". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "Drug Approval Package: Brand Name (Generic Name) NDA #". U.S. Food and Drug Administration (FDA). 20 December 2013. Archived from the original on 22 November 2019. Retrieved 21 November 2019.
- "New Drug Application (NDA) 012380". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 010841". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 022334". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 020189". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 020450". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 020235". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 022253". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 020241". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 021035". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- EPAR: Keppra. Archived 19 June 2009 at the Wayback Machine Retrieved on 1 November 2007.
- "New Drug Application (NDA) 006008". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 008322". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- Dodson, W. Edwin; Giuliano Avanzini; Shorvon, Simon D.; Fish, David R.; Emilio Perucca (2004). The treatment of epilepsy. Oxford: Blackwell Science. xxviii. ISBN 978-0-632-06046-7.
- "New Drug Application (NDA) 010596". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 011721". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 021014". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 008762". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019. (Marketed in 1938, approved 1953)
- "New Drug Application (NDA) 008855". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- Kutt, Henn; Resor, Stanley R. (1992). The Medical treatment of epilepsy. New York: Dekker. p. 385. ISBN 978-0-8247-8549-9. (first usage)
- "New Drug Application (NDA) 021446". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- EPAR: Lyrica Archived 21 June 2009 at the Wayback Machine Retrieved on 1 November 2007.
- "New Drug Application (NDA) 009170". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 021911". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "Drug Approval Package: Banzel (Rufinamide) NDA #021911". U.S. Food and Drug Administration (FDA). 30 May 2012. Archived from the original on 22 November 2019. Retrieved 21 November 2019.
- "New Drug Application (NDA) 206709". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "Drug Approval Package: Diacomit (stiripentol)". U.S. Food and Drug Administration (FDA). 7 September 2018. Archived from the original on 22 November 2019. Retrieved 21 November 2019.
- "New Drug Application (NDA) 020646". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "NDA: 020646". DrugPatentWatch. Retrieved 19 May 2013.
- "New Drug Application (NDA) 020505". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 005856". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 018081". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 020427". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- "New Drug Application (NDA) 020789". Drugs@FDA. U.S. Food and Drug Administration (FDA). Retrieved 21 November 2019.
- EPAR: Zonegran. Archived 13 July 2009 at the Wayback Machine Retrieved on 1 November 2007
- Harden CL, Pennell PB, Koppel BS, et al. (May 2009). "Management issues for women with epilepsy—focus on pregnancy (an evidence-based review): III. Vitamin K, folic acid, blood levels, and breast-feeding: Report of the Quality Standards Subcommittee and Therapeutics and Technology Assessment Subcommittee of the American Academy of Neurology and the American Epilepsy Society". Epilepsia. 50 (5): 1247–55. doi:10.1111/j.1528-1167.2009.02130.x. PMID 19507305. S2CID 221731995.
- Weston, Jennifer; Bromley, Rebecca; Jackson, Cerian F.; Adab, Naghme; Clayton-Smith, Jill; Greenhalgh, Janette; Hounsome, Juliet; McKay, Andrew J.; Tudur Smith, Catrin (7 November 2016). "Monotherapy treatment of epilepsy in pregnancy: congenital malformation outcomes in the child". The Cochrane Database of Systematic Reviews. 11: CD010224. doi:10.1002/14651858.CD010224.pub2. ISSN 1469-493X. PMC 6465055. PMID 27819746.
- Bromley, Rebecca; Weston, Jennifer; Adab, Naghme; Greenhalgh, Janette; Sanniti, Anna; McKay, Andrew J; Tudur Smith, Catrin; Marson, Anthony G (2014). "Treatment for epilepsy in pregnancy: neurodevelopmental outcomes in the child". Reviews. 2020 (10): CD010236. doi:10.1002/14651858.CD010236.pub2. PMC 7390020. PMID 25354543.
- Jazayeri, Dana; Graham, Janet; Hitchcock, Alison; O'Brien, Terence J.; Vajda, Frank J.E. (2018). "Outcomes of pregnancies in women taking antiepileptic drugs for non-epilepsy indications". Seizure. 56: 111–114. doi:10.1016/j.seizure.2018.02.009. ISSN 1059-1311. PMID 29471258.
- George, Ilena C. (2017). "Practice Current: How do you treat epilepsy in pregnancy?". Neurology: Clinical Practice. 7 (4): 363–371. doi:10.1212/cpj.0000000000000387. ISSN 2163-0402. PMC 5648199. PMID 29185530.
- Bittigau P, Sifringer M, Genz K, et al. (May 2002). "Antiepileptic drugs and apoptotic neurodegenereation in the developing brain". Proceedings of the National Academy of Sciences of the United States of America. 99 (23): 15089–94. Bibcode:2002PNAS...9915089B. doi:10.1073/pnas.222550499. PMC 137548. PMID 12417760.
- Manthey D, Asimiadou S, et al. (June 2005). "Sulthiame but not levetiracetam exerts neurotoxic effect in the developing rat brain". Exp Neurol. 193 (2): 497–503. doi:10.1016/j.expneurol.2005.01.006. PMID 15869952. S2CID 1493015.
- Katz I, Kim J, et al. (August 2007). "Effects of lamotrigine alone and in combination with MK-801, phenobarbital, or phenytoin on cell death in the neonatal rat brain". J Pharmacol Exp Ther. 322 (2): 494–500. doi:10.1124/jpet.107.123133. PMID 17483293. S2CID 12741109.
- Kim J, Kondratyev A, Gale K (October 2007). "Antiepileptic drug-induced neuronal cell death in the immature brain: effects of carbamazepine, topiramate, and levetiracetam as monotherapy versus polytherapy". J Pharmacol Exp Ther. 323 (1): 165–73. doi:10.1124/jpet.107.126250. PMC 2789311. PMID 17636003.
- Forcelli PA, Kim J, et al. (December 2011). "Pattern of antiepileptic drug-induced cell death in limbic regions of the neonatal rat brain". Epilepsia. 52 (12): e207–11. doi:10.1111/j.1528-1167.2011.03297.x. PMC 3230752. PMID 22050285.
Further reading
- Anti epileptic activity of novel substituted fluorothiazole derivatives by Devid Chutia, RGUHS
External links
- eMedicine: Antiepileptic Drugs: an overview
- NINDS: Anticonvulsant Screening Program Archived 11 March 2007 at the Wayback Machine
- Use of Anticonvulsants in Pharmacotherapy of Bronchial Asthma
- MDNG: Anticonvulsants and Bone Health
- Miami Children's Brain Institute – Anticonvulsants
- Drug Reference for FDA Approved Epilepsy Drugs
- Epilepsy Action: UK Anti-Epileptic Drugs List