Bone density
Bone density, or bone mineral density, is the amount of bone mineral in bone tissue. The concept is of mass of mineral per volume of bone (relating to density in the physics sense), although clinically it is measured by proxy according to optical density per square centimetre of bone surface upon imaging.[1] Bone density measurement is used in clinical medicine as an indirect indicator of osteoporosis and fracture risk. It is measured by a procedure called densitometry, often performed in the radiology or nuclear medicine departments of hospitals or clinics. The measurement is painless and non-invasive and involves low radiation exposure. Measurements are most commonly made over the lumbar spine and over the upper part of the hip.[2] The forearm may be scanned if the hip and lumbar spine are not accessible.
There is a statistical association between poor bone density and higher probability of fracture. Fractures of the legs and pelvis due to falls are a significant public health problem, especially in elderly women, leading to much medical cost, inability to live independently and even risk of death.[3] Bone density measurements are used to screen people for osteoporosis risk and to identify those who might benefit from measures to improve bone strength.
Testing
Bone density tests are not recommended for people without risk factors for weak bones,[4][5] which is more likely to result in unnecessary treatment rather than discovery of a true problem.[5]
Indications for testing
The risk factors for low bone density and primary considerations for a bone density test include:
- females age 65 or older.[5]
- males age 70 or older.[5]
- people over age 50 with:
- individuals with vertebral abnormalities.[6]
- individuals receiving, or planning to receive, long-term glucocorticoid (steroid) therapy.[6]
- individuals with primary hyperparathyroidism.[6]
- individuals being monitored to assess the response or efficacy of an approved osteoporosis drug therapy.[6]
- when androgen deprivation therapy is being planned for prostate cancer.
- individuals with a history of eating disorders.[6]
Other considerations that are related to risk of low bone density and the need for a test include smoking habits, drinking habits, the long-term use of corticosteroid drugs, and a vitamin D deficiency.[5]
Conditions found
A bone density test may detect osteoporosis or osteopenia.[5] The usual response to either of these indications is consultation with a physician.[5]
Test result terms
Results of the test are often reported in three terms:
Types of tests
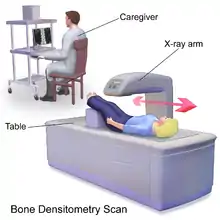
While there are many different types of bone mineral density tests, all are non-invasive. Most tests differ according to which bones are measured to determine the test result.
These tests include:
- Dual-energy X-ray absorptiometry (DXA or DEXA)
- Trabecular bone score
- Dual X-ray Absorptiometry and Laser (DXL)
- Quantitative computed tomography (QCT)
- Quantitative ultrasound (QUS)
- Single photon absorptiometry (SPA)
- Dual photon absorptiometry (DPA)
- Digital X-ray radiogrammetry (DXR)
- Single energy X-ray absorptiometry (SEXA)
DXA is currently the most widely used, but quantitative ultrasound (QUS) has been described as a more cost-effective approach to measure bone density.[7] The DXA test works by measuring a specific bone or bones, usually the spine, hip, and wrist. The density of these bones is then compared with an average index based on age, sex, and size. The resulting comparison is used to determine the risk for fractures and the stage of osteoporosis (if any) in an individual.
Average bone mineral density = BMC / W [g/cm2]
- BMC = bone mineral content = g/cm
- W = width at the scanned line
Interpretation
Results are generally scored by two measures, the T-score and the Z-score. Scores indicate the amount one's bone mineral density varies from the mean. Negative scores indicate lower bone density, and positive scores indicate higher.
Less than 0.5% of patients who underwent DXA-scanning were found to have a T- or Z-score of more than +4.0, often the cause of an unusually high bone mass (HBM) and associated with mild skeletal dysplasia and the inability to float in water.[8]
T-score
The T-score is the relevant measure when screening for osteoporosis. It is the bone mineral density at the site when compared to the "young normal reference mean". It is a comparison of a patient's bone mineral density to that of a healthy 30-year-old.[9] The US standard is to use data for a 30-year-old of the same sex and ethnicity, but the WHO recommends using data for a 30-year-old white female for everyone.[10] Values for 30-year-olds are used in post-menopausal women and men over age 50 because they better predict risk of future fracture.[11] The criteria of the World Health Organization are:[12]
- Normal is a T-score of −1.0 or higher[13]
- Osteopenia is defined as between −1.0 and −2.5
- Osteoporosis is defined as −2.5 or lower, meaning a bone density that is two and a half standard deviations below the mean of a 30-year-old man/woman.
| WHO category | Age 50–64 | Age > 64 | Overall |
|---|---|---|---|
| Normal | 5.3 | 9.4 | 6.6 |
| Osteopenia | 11.4 | 19.6 | 15.7 |
| Osteoporosis | 22.4 | 46.6 | 40.6 |
Z-score
The Z-score for bone density is the comparison to the "age-matched normal" and is usually used in cases of severe osteoporosis. This is the standard score or number of standard deviations a patient's bone mineral density differs from the average for their age, sex, and ethnicity. This value is used in premenopausal women, men under the age of 50, and in children and adolescents.[11][15] It is most useful when the score is less than 2 standard deviations below this normal. In this setting, it is helpful to scrutinize for coexisting illnesses or treatments that may contribute to osteoporosis such as glucocorticoid therapy, hyperparathyroidism, or alcoholism.
Prevention
To prevent low bone density it is recommended to have sufficient calcium and vitamin D.[16][17] Sufficient calcium is defined as 1,000 mg per day, increasing to 1,200 mg for women above 50 and men above 70.[17] Sufficient vitamin D is defined as 600 IUs per day for adults 19 to 70, increasing to 800 IUs per day for those over 71.[17] Exercise, especially weight-bearing and resistance exercises are most effective for building bone. Weight-bearing exercise includes walking, jogging, dancing, and hiking. Resistance exercise is often accomplished through lifting weights.[18] Other therapies, such as estrogens (e.g., estradiol, conjugated estrogens), selective estrogen receptor modulators (e.g., raloxifene, bazedoxifene), and bisphosphonates (e.g., alendronic acid, risedronic acid), can also be used to improve or maintain bone density. Tobacco use and excessive alcohol consumption have detrimental effects on bone density.[19][17] Excessive alcohol consumption is defined as more than one standard-sized alcoholic beverage per day for women, and drinking two or more alcoholic beverages per day for men.[17]
Genetics
Bone mineral density is highly variable between individuals. While there are many environmental factors that affect bone mineral density, genetic factors play a large role as well.[20][21] Bone Mineral Density variation has been estimated to have 0.6-0.8 heritability factor, meaning that 60-80% of its variation is inherited from parents.[21] Because of the heritability of Bone Mineral Density, family history of fractures is considered as a risk factor for osteoporosis.[22] Bone Mineral Density is polygenic and many of the genetic mechanisms still remain poorly understood.[20]
Genetic Diseases Associated with Bone Mineral Density
There are several rare genetic diseases that have been associated with pathologic changes in bone mineral density. The table below summarizes these diseases:[23][22]
| Disease | Gene Affected | Inheritance | Source |
|---|---|---|---|
| Osteogenesis Imperfecta | COLIA1 | Autosomal Recessive | [23][22] |
| Osteogenesis Imperfecta | COLIA2 | Autosomal Recessive | [23][22] |
| Osteoporosis Pseudoglioma Syndrome | LRP5 | Autosomal Recessive | [22] |
| Osteopetrosis | TCIRGI | Autosomal Recessive | [22] |
| Camurati-Engelmann Disease | TGFβ-1 | Autosomal Recessive | [22] |
| Van Buchem Disease | SOST | Autosomal Recessive | [22] |
| Severe Infantile Osteopetrosis | CLCN7 | Autosomal Recessive | [22] |
References
- Bone+Density at the US National Library of Medicine Medical Subject Headings (MeSH)
- Cole RE (June 2008). "Improving clinical decisions for women at risk of osteoporosis: dual-femur bone mineral density testing". J Am Osteopath Assoc. 108 (6): 289–95. PMID 18587077.
- "Preventing Falls and Related Fractures | NIH Osteoporosis and Related Bone Diseases National Resource Center". www.bones.nih.gov. Retrieved 2021-03-12.
- American Academy of Family Physicians, presented by ABIM Foundation, "Five Things Physicians and Patients Should Question" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, American Academy of Family Physicians, archived from the original (PDF) on June 24, 2012, retrieved August 14, 2012
- Consumer Reports; American Academy of Family Physicians (May 2012), "Bone-density tests: When you need them – and when you don't" (PDF), Choosing Wisely: an initiative of the ABIM Foundation, Consumer Reports, retrieved August 14, 2012
- "Bone Mass Measurement". NOF. Archived from the original on 2008-03-07. Retrieved 2008-03-20.
- "Bone densitometry". Retrieved 2008-09-02.
- Gregson CL, Steel SA, O'Rourke KP, et al.: 'Sink or swim': an evaluation of the clinical characteristics of individuals with high bone mass. Journal Osteoporos Int./ Osteoporosis Int., 2012 Feb; 23(2): 643–654. Published online 2011 Apr 1. doi: 10.1007/s00198-011-1603-4. PMCID: PMC3261396. PMID 21455762
- "Bone Density Scan: MedlinePlus Medical Test". medlineplus.gov. Retrieved 2020-10-29.
- Unknown, Unknown (2011-07-29). "T and Z scores". University of Washington Bone Physics. Retrieved 2013-06-22.
- Richmond, Bradford (2007-11-13). "Osteoporosis and bone mineral density". American College of Radiology. Archived from the original on 2008-09-17. Retrieved 2008-05-11.
- WHO Scientific Group on the Prevention and Management of Osteoporosis (2000 : Geneva, Switzerland) (2003). "Prevention and management of osteoporosis : report of a WHO scientific group" (PDF). Retrieved 2007-05-31.
- "Bone Mass Measurement: What the Numbers Mean | NIH Osteoporosis and Related Bone Diseases National Resource Center". www.bones.nih.gov. Retrieved 2021-03-12.
- Cranney A, Jamal SA, Tsang JF, Josse RG, Leslie WD (2007). "Low bone mineral density and fracture burden in postmenopausal women". Canadian Medical Association Journal. 177 (6): 575–80. doi:10.1503/cmaj.070234. PMC 1963365. PMID 17846439.
- Bachrach LK (February 2005). "Assessing bone health in children: who to test and what does it mean?". Pediatr Endocrinol Rev. 2 Suppl 3: 332–6. PMID 16456501.
- Lawrence, Jean. "Building Stronger Bones". WebMD. Retrieved 2020-04-20.
- "How to keep your bones healthy". Mayo Clinic. Retrieved 2020-04-20.
- "Exercise for Your Bone Health | NIH Osteoporosis and Related Bone Diseases National Resource Center". www.bones.nih.gov. Retrieved 2020-11-09.
- "Smoking and Bone Health | NIH Osteoporosis and Related Bone Diseases National Resource Center". www.bones.nih.gov. Retrieved 2022-09-19.
- Yang, Tie-Lin; Shen, Hui; Liu, Anqi; Dong, Shan-Shan; Zhang, Lei; Deng, Fei-Yan; Zhao, Qi; Deng, Hong-Wen (February 2020). "A road map for understanding molecular and genetic determinants of osteoporosis". Nature Reviews Endocrinology. 16 (2): 91–103. doi:10.1038/s41574-019-0282-7. ISSN 1759-5037. PMC 6980376. PMID 31792439.
- Peacock, Munro; Turner, Charles H.; Econs, Michael J.; Foroud, Tatiana (2002-06-01). "Genetics of Osteoporosis". Endocrine Reviews. 23 (3): 303–326. doi:10.1210/edrv.23.3.0464. ISSN 0163-769X. PMID 12050122.
- Huang, Qing-Yang; Kung, Annie Wai Chee (2006-08-01). "Genetics of osteoporosis". Molecular Genetics and Metabolism. 88 (4): 295–306. doi:10.1016/j.ymgme.2006.04.009. ISSN 1096-7192. PMID 16762578.
- Marom, Ronit; Rabenhorst, Brien M.; Morello, Roy (2020-10-01). "Management of Endocrine Disease: Osteogenesis imperfecta: an update on clinical features and therapies". European Journal of Endocrinology. 183 (4): R95–R106. doi:10.1530/EJE-20-0299. ISSN 0804-4643. PMC 7694877. PMID 32621590.