Germ theory of disease
The germ theory of disease is the currently accepted scientific theory for many diseases. It states that microorganisms known as pathogens or "germs" can lead to disease. These small organisms, too small to be seen without magnification, invade humans, other animals, and other living hosts. Their growth and reproduction within their hosts can cause disease. "Germ" refers to not just a bacterium but to any type of microorganism, such as protists or fungi, or even non-living pathogens that can cause disease, such as viruses, prions, or viroids.[1] Diseases caused by pathogens are called infectious diseases. Even when a pathogen is the principal cause of a disease, environmental and hereditary factors often influence the severity of the disease, and whether a potential host individual becomes infected when exposed to the pathogen. Pathogens are disease-carrying agents that can pass from one individual to another, both in humans and animals. Infectious diseases are caused by biological agents such as pathogenic microorganisms (viruses, bacteria, and fungi) as well as parasites.

Basic forms of germ theory were proposed by Girolamo Fracastoro in 1546, and expanded upon by Marcus von Plenciz in 1762. However, such views were held in disdain in Europe, where Galen's miasma theory remained dominant among scientists and doctors.
By the early 19th century, smallpox vaccination was commonplace in Europe, though doctors were unaware of how it worked or how to extend the principle to other diseases. A transitional period began in the late 1850s with the work of Louis Pasteur. This work was later extended by Robert Koch in the 1880s. By the end of that decade, the miasma theory was struggling to compete with the germ theory of disease. Viruses were initially discovered in the 1890s. Eventually, a "golden era" of bacteriology ensued, during which the germ theory quickly led to the identification of the actual organisms that cause many diseases.[2]
Miasma theory

The miasma theory was the predominant theory of disease transmission before the germ theory took hold towards the end of the 19th century; it is no longer accepted as a correct explanation for disease by the scientific community. It held that diseases such as cholera, chlamydia infection, or the Black Death were caused by a miasma (μίασμα, Ancient Greek: "pollution"), a noxious form of "bad air" emanating from rotting organic matter.[3] Miasma was considered to be a poisonous vapor or mist filled with particles from decomposed matter (miasmata) that was identifiable by its foul smell. The theory posited that diseases were the product of environmental factors such as contaminated water, foul air, and poor hygienic conditions. Such infections, according to the theory, were not passed between individuals but would affect those within a locale that gave rise to such vapors.[4]
Development
Ancient India
In the Sushruta Samhita, the ancient Indian physician Sushruta theorized: "Leprosy, fever, consumption, diseases of the eye, and other infectious diseases spread from one person to another by sexual union, physical contact, eating together, sleeping together, sitting together, and the use of same clothes, garlands and pastes."[5][6] The book has been dated to about the sixth century BC.[lower-alpha 1][7]
Ancient Judea
The Mosaic Law, within the first five books of the Hebrew Bible, contains the earliest recorded thoughts of contagion in the spread of disease, standing in contrast with classical medical tradition and the Hippocratic writings. Specifically, it presents instructions on quarantine and washing in relation to leprosy and venereal disease.[8]
Greece and Rome
In Antiquity, the Greek historian Thucydides (c. 460 – c. 400 BC) was the first person to write, in his account of the plague of Athens, that diseases could spread from an infected person to others.[9][10]
One theory of the spread of contagious diseases that were not spread by direct contact was that they were spread by spore-like "seeds" (Latin: semina) that were present in and dispersible through the air. In his poem, De rerum natura (On the Nature of Things, c. 56 BC), the Roman poet Lucretius (c. 99 BC – c. 55 BC) stated that the world contained various "seeds", some of which could sicken a person if they were inhaled or ingested.[11][12]
The Roman statesman Marcus Terentius Varro (116–27 BC) wrote, in his Rerum rusticarum libri III (Three Books on Agriculture, 36 BC): "Precautions must also be taken in the neighborhood of swamps ... because there are bred certain minute creatures which cannot be seen by the eyes, which float in the air and enter the body through the mouth and nose and there cause serious diseases."[13]
The Greek physician Galen (AD 129 – c. 200/216) speculated in his On Initial Causes (c. 175 AD that some patients might have "seeds of fever".[11]: 4 In his On the Different Types of Fever (c. 175 AD), Galen speculated that plagues were spread by "certain seeds of plague", which were present in the air.[11]: 6 And in his Epidemics (c. 176–178 AD), Galen explained that patients might relapse during recovery from fever because some "seed of the disease" lurked in their bodies, which would cause a recurrence of the disease if the patients did not follow a physician's therapeutic regimen.[11]: 7
The Middle Ages
A basic form of contagion theory dates back to medicine in the medieval Islamic world, where it was proposed by Persian physician Ibn Sina (known as Avicenna in Europe) in The Canon of Medicine (1025), which later became the most authoritative medical textbook in Europe up until the 16th century. In Book IV of the El-Kanun, Ibn Sina discussed epidemics, outlining the classical miasma theory and attempting to blend it with his own early contagion theory. He mentioned that people can transmit disease to others by breath, noted contagion with tuberculosis, and discussed the transmission of disease through water and dirt.[14]
The concept of invisible contagion was later discussed by several Islamic scholars in the Ayyubid Sultanate who referred to them as najasat ("impure substances"). The fiqh scholar Ibn al-Haj al-Abdari (c. 1250–1336), while discussing Islamic diet and hygiene, gave warnings about how contagion can contaminate water, food, and garments, and could spread through the water supply, and may have implied contagion to be unseen particles.[15]
During the early Middle Ages, Isidore of Seville (c. 560–636) mentioned "plague-bearing seeds" (pestifera semina) in his On the Nature of Things (c. AD 613).[11]: 20 Later in 1345, Tommaso del Garbo (c. 1305–1370) of Bologna, Italy mentioned Galen's "seeds of plague" in his work Commentaria non-parum utilia in libros Galeni (Helpful commentaries on the books of Galen).[11]: 214
The Italian scholar and physician Girolamo Fracastoro proposed in 1546 in his book De Contagione et Contagiosis Morbis that epidemic diseases are caused by transferable seed-like entities (seminaria morbi) that transmit infection by direct or indirect contact, or even without contact over long distances. The diseases were categorised based on how they were transmitted, and how long they could lie dormant.
The Early Modern Period
Italian physician Francesco Redi provided early evidence against spontaneous generation. He devised an experiment in 1668 in which he used three jars. He placed a meatloaf and egg in each of the three jars. He had one of the jars open, another one tightly sealed, and the last one covered with gauze. After a few days, he observed that the meatloaf in the open jar was covered with maggots, and the jar covered with gauze had maggots on the surface of the gauze. However, the tightly sealed jar had no maggots inside or outside it. He also noticed that the maggots were found only on surfaces that were accessible by flies. From this he concluded that spontaneous generation is not a plausible theory.
Microorganisms are said to have been first directly observed in the 1670s by Anton van Leeuwenhoek, an early pioneer in microbiology, considered "the Father of Microbiology". Leeuwenhoek is said to be the first to see and describe bacteria (1674), yeast cells, the teeming life in a drop of water (such as algae), and the circulation of blood corpuscles in capillaries. The word "bacteria" didn't exist yet, so he called these microscopic living organisms "animalcules", meaning "little animals". Those "very little animalcules" he was able to isolate from different sources, such as rainwater, pond and well water, and the human mouth and intestine. Yet German Jesuit priest and scholar Athanasius Kircher may have observed such microorganisms prior to this. One of his books written in 1646 contains a chapter in Latin, which reads in translation "Concerning the wonderful structure of things in nature, investigated by Microscope", stating "who would believe that vinegar and milk abound with an innumerable multitude of worms." Kircher defined the invisible organisms found in decaying bodies, meat, milk, and secretions as "worms." His studies with the microscope led him to the belief, which he was possibly the first to hold, that disease and putrefaction (decay) were caused by the presence of invisible living bodies. In 1646, Kircher (or "Kirchner", as it is often spelled), wrote that "a number of things might be discovered in the blood of fever patients." When Rome was struck by the bubonic plague in 1656, Kircher investigated the blood of plague victims under the microscope. He noted the presence of "little worms" or "animalcules" in the blood and concluded that the disease was caused by microorganisms. He was the first to attribute infectious disease to a microscopic pathogen, inventing the germ theory of disease, which he outlined in his Scrutinium Physico-Medicum (Rome 1658).[16] Kircher's conclusion that disease was caused by microorganisms was correct, although it is likely that what he saw under the microscope were in fact red or white blood cells and not the plague agent itself. Kircher also proposed hygienic measures to prevent the spread of disease, such as isolation, quarantine, burning clothes worn by the infected, and wearing facemasks to prevent the inhalation of germs. It was Kircher who first proposed that living beings enter and exist in the blood.
In 1700, physician Nicolas Andry argued that microorganisms he called "worms" were responsible for smallpox and other diseases.[17]
In 1720, Richard Bradley theorised that the plague and "all pestilential distempers" were caused by "poisonous insects", living creatures viewable only with the help of microscopes.[18]
In 1762, the Austrian physician Marcus Antonius von Plenciz (1705–1786) published a book titled Opera medico-physica. It outlined a theory of contagion stating that specific animalcules in the soil and the air were responsible for causing specific diseases. Von Plenciz noted the distinction between diseases which are both epidemic and contagious (like measles and dysentery), and diseases which are contagious but not epidemic (like rabies and leprosy).[19] The book cites Anton van Leeuwenhoek to show how ubiquitous such animalcules are and was unique for describing the presence of germs in ulcerating wounds. Ultimately, the theory espoused by von Plenciz was not accepted by the scientific community.
Agostino Bassi, Italy
The Italian Agostino Bassi was the first person to prove that a disease was caused by a microorganism when he conducted a series of experiments between 1808 and 1813, demonstrating that a "vegetable parasite" caused a disease in silkworms known as calcinaccio which was devastating the French silk industry at the time. The "vegetable parasite" is now known to be a fungus pathogenic to insects called Beauveria bassiana (named after Bassi).
Louis-Daniel Beauperthuy, France
In 1838 French specialist in tropical medicine Louis-Daniel Beauperthuy pioneered using microscopy in relation to diseases and independently developed a theory that all infectious diseases were due to parasitic infection with "animalcules" (microorganisms). With the help of his friend M. Adele de Rosseville, he presented his theory in a formal presentation before the French Academy of Sciences in Paris. By 1853, he was convinced that malaria and yellow fever were spread by mosquitos. He even identified the particular group of mosquitos that transmit yellow fever as the "domestic species" of "striped-legged mosquito", which can be recognised as Aedes aegypti, the actual vector. He published his theory in 1854 in the Gaceta Oficial de Cumana ("Official Gazette of Cumana"). His reports were assessed by an official commission, which discarded his mosquito theory.[20]
Ignaz Semmelweis, Austria
Ignaz Semmelweis, a Hungarian obstetrician working at the Vienna General Hospital (Allgemeines Krankenhaus) in 1847, noticed the dramatically high maternal mortality from puerperal fever following births assisted by doctors and medical students. However, those attended by midwives were relatively safe. Investigating further, Semmelweis made the connection between puerperal fever and examinations of delivering women by doctors, and further realized that these physicians had usually come directly from autopsies. Asserting that puerperal fever was a contagious disease and that matter from autopsies were implicated in its development, Semmelweis made doctors wash their hands with chlorinated lime water before examining pregnant women. He then documented a sudden reduction in the mortality rate from 18% to 2.2% over a period of a year. Despite this evidence, he and his theories were rejected by most of the contemporary medical establishment.[21]
Gideon Mantell, UK
Gideon Mantell, the Sussex doctor more famous for discovering dinosaur fossils, spent time with his microscope, and speculated in his Thoughts on Animalcules (1850) that perhaps "many of the most serious maladies which afflict humanity, are produced by peculiar states of invisible animalcular life".[22]
John Snow, UK
John Snow was a skeptic of the then-dominant miasma theory. Even though the germ theory of disease pioneered by Girolamo Fracastoro had not yet achieved full development or widespread currency, Snow demonstrated a clear understanding of germ theory in his writings. He first published his theory in an 1849 essay On the Mode of Communication of Cholera, in which he correctly suggested that the fecal–oral route was the mode of communication, and that the disease replicated itself in the lower intestines. He even proposed in his 1855 edition of the work, that the structure of cholera was that of a cell.
Snow's 1849 recommendation that water be "filtered and boiled before it is used" is one of the first practical applications of germ theory in the area of public health and is the antecedent to the modern boil-water advisory. In 1855 he published a second edition of his article, documenting his more elaborate investigation of the effect of the water supply in the Soho, London epidemic of 1854.
By talking to local residents, he identified the source of the outbreak as the public water pump on Broad Street (now Broadwick Street). Although Snow's chemical and microscope examination of a water sample from the Broad Street pump did not conclusively prove its danger, his studies of the pattern of the disease were convincing enough to persuade the local council to disable the well pump by removing its handle. This action has been commonly credited as ending the outbreak, but Snow observed that the epidemic may have already been in rapid decline.[23] Snow's study was a major event in the history of public health and geography. It is regarded as one of the founding events of the science of epidemiology.
After the cholera epidemic had subsided, government officials replaced the handle on the Broad Street pump. They had responded only to the urgent threat posed to the population, and afterward, they rejected Snow's theory. To accept his proposal would have meant accepting the fecal–oral method transmission of disease, which they dismissed.[24]
Louis Pasteur, France
The more formal experiments on the relationship between germ and disease were conducted by Louis Pasteur between the years 1860 and 1864. He discovered the pathology of the puerperal fever[25] and the pyogenic vibrio in the blood, and suggested using boric acid to kill these microorganisms before and after confinement.
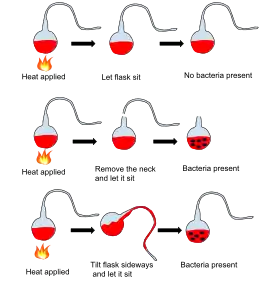
Pasteur further demonstrated between 1860 and 1864 that fermentation and the growth of microorganisms in nutrient broths did not proceed by spontaneous generation. He exposed freshly boiled broth to air in vessels that contained a filter to stop all particles passing through to the growth medium, and even with no filter at all, with air being admitted via a long tortuous tube that would not pass dust particles. Nothing grew in the broths: therefore the living organisms that grew in such broths came from outside, as spores on dust, rather than being generated within the broth.
Pasteur discovered that another serious disease of silkworms, pébrine, was caused by a microscopic organism now known as Nosema bombycis (1870). Pasteur saved France's silk industry by developing a method to screen silkworms eggs for those that were not infected, a method that is still used today to control this and other silkworm diseases.
Robert Koch, Germany
Robert Koch is known for developing four basic criteria (known as Koch's postulates) for demonstrating, in a scientifically sound manner, that a disease is caused by a particular organism. These postulates grew out of his seminal work with anthrax using purified cultures of the pathogen that had been isolated from diseased animals.
Koch's postulates were developed in the 19th century as general guidelines to identify pathogens that could be isolated with the techniques of the day.[26] Even in Koch's time, it was recognized that some infectious agents were clearly responsible for disease even though they did not fulfill all of the postulates.[27][28] Attempts to rigidly apply Koch's postulates to the diagnosis of viral diseases in the late 19th century, at a time when viruses could not be seen or isolated in culture, may have impeded the early development of the field of virology.[29][30] Currently, a number of infectious agents are accepted as the cause of disease despite their not fulfilling all of Koch's postulates.[31] Therefore, while Koch's postulates retain historical importance and continue to inform the approach to microbiologic diagnosis, fulfillment of all four postulates is not required to demonstrate causality.
Koch's postulates have also influenced scientists who examine microbial pathogenesis from a molecular point of view. In the 1980s, a molecular version of Koch's postulates was developed to guide the identification of microbial genes encoding virulence factors.[32]
Koch's postulates:
- The microorganism must be found in abundance in all organisms with the disease, but should not be found in healthy organisms.
- The microorganism must be isolated from a diseased organism and grown in pure culture.
- The cultured microorganism should cause disease when introduced into a healthy organism.
- The microorganism must be reisolated from the inoculated, diseased experimental host and identified as being identical to the original specific causative agent.
However, Koch abandoned the universalist requirement of the first postulate altogether when he discovered asymptomatic carriers of cholera[28] and, later, of typhoid fever. Asymptomatic or subclinical infection carriers are now known to be a common feature of many infectious diseases, especially viruses such as polio, herpes simplex, HIV, hepatitis C, and COVID-19. As a specific example, all doctors and virologists agree that poliovirus causes paralysis in just a few infected subjects, and the success of the polio vaccine in preventing disease supports the conviction that the poliovirus is the causative agent.
The third postulate specifies "should", not "must", because as Koch himself proved in regard to both tuberculosis and cholera,[27] not all organisms exposed to an infectious agent will acquire the infection. Noninfection may be due to such factors as general health and proper immune functioning; acquired immunity from previous exposure or vaccination; or genetic immunity, as with the resistance to malaria conferred by possessing at least one sickle cell allele.
The second postulate may also be suspended for certain microorganisms or entities that cannot (at the present time) be grown in pure culture, such as prions responsible for Creutzfeldt–Jakob disease.[33] In summary, a body of evidence that satisfies Koch's postulates is sufficient but not necessary to establish causation.
Joseph Lister, UK
In the 1870s, Joseph Lister was instrumental in developing practical applications of the germ theory of disease with respect to sanitation in medical settings and aseptic surgical techniques—partly through the use of carbolic acid (phenol) as an antiseptic.
See also
- Alexander Fleming
- Cell theory
- Epidemiology
- Germ theory denialism
- History of emerging infectious diseases
- Robert Hooke
- Rudolf Virchow
- Zymotic disease
Notes
- Other estimates of date range from 1000 BCE to 500 CE
References
- "Definition of Germ in English from the Oxford dictionary". Oxford Dictionaries. Archived from the original on 6 April 2016. Retrieved 5 April 2016.
- "Brief History During the Snow Era". ucla.edu. Archived from the original on 17 January 2017. Retrieved 1 January 2016.
- Last JM, ed. (2007), "miasma theory", A Dictionary of Public Health, Westminster College, Pennsylvania: Oxford University Press, ISBN 9780195160901
- Tsoucalas G, Spengos K, Panayiotakopoulos G, Papaioannou T, Karamanou M (15 February 2018). "Epilepsy, Theories and Treatment Inside Corpus Hippocraticum". Current Pharmaceutical Design. 23 (42): 6369–6372. doi:10.2174/1381612823666171024153144. PMID 29076418.
- Rastogi N, Rastogi RC (December 1984). "Leprosy in ancient India". International Journal of Leprosy and Other Mycobacterial Diseases. 52 (4): 541–543. PMID 6399073.
- Susruta S, Bhishagratna KL (1907–1916). An English translation of the Sushruta samhita, based on original Sanskrit text. Edited and published by Kaviraj Kunja Lal Bhishagratna. With a full and comprehensive introd., translation of different readings, notes, comparative views, index, glossary and plates. Gerstein - University of Toronto. Calcutta.
- Hoernle AF (1907). Studies in the medicine of ancient India. Gerstein - University of Toronto. Oxford : At the Clarendon Press.
- McGrew RE (1985). Encyclopedia of medical history. London: Macmillan. ISBN 978-0-333-28802-3.
- Singer, Charles and Dorothea (1917) "The scientific position of Girolamo Fracastoro [1478?–1553] with especial reference to the source, character and influence of his theory of infection," Annals of Medical History, 1 : 1–34; see p. 14.
- Thucydides with Richard Crawley, trans., History of the Peloponnesian War (London, England: J.M. Dent & Sons, Ltd., 1910), Book III, § 51, pp. 131–32. From pp. 131–32: " … there was the awful spectacle of men dying like sheep, through having caught the infection in nursing each other. This caused the greatest mortality. On the one hand, if they were afraid to visit each other, they perished from neglect; indeed many houses were emptied of their inmates for want of a nurse: on the other, if they ventured to do so, death was the consequence."
- Nutton V (January 1983). "The seeds of disease: an explanation of contagion and infection from the Greeks to the Renaissance". Medical History. 27 (1): 1–34. doi:10.1017/s0025727300042241. PMC 1139262. PMID 6339840.
- Lucretius with Rev. John S. Watson, trans., On the Nature of Things (London, England: Henry G. Bohn, 1851), Book VI, lines 1093–1130, pp. 291–92; see especially p. 292. From p. 292: "This new malady and pest, therefore, either suddenly falls into the water, or penetrates into the very corn, or into other food of men and cattle. Or even, as may be the case, the infection remains suspended in the air itself; and when, as we breathe, we inhale the air mingled with it, we must necessarily absorb those seeds of disease into our body."
- Varro MT, Storr-Best L (1912). "XII". Varro on Farming. Vol. Book 1. London, England: G. Bell and Sons, Ltd. p. 9.
- Byrne JP (2012). Encyclopedia of the Black Death. ABC-CLIO. p. 29. ISBN 9781598842531.
- Reid MH (2013). Law and Piety in Medieval Islam. Cambridge University Press. pp. 106, 114, 189–190. ISBN 9781107067110.
- "The Life and Work of Athanaseus Kircher, S.J." mjt.org. Archived from the original on 17 April 2016. Retrieved 18 April 2016.
- "The History of the Germ Theory". The British Medical Journal. 1 (1415): 312. 1888.
- Santer M (2009). "Richard Bradley: a unified, living agent theory of the cause of infectious diseases of plants, animals, and humans in the first decades of the 18th century". Perspectives in Biology and Medicine. 52 (4): 566–78. doi:10.1353/pbm.0.0124. PMID 19855125. S2CID 22544615.
- Winslow CE (1967). Conquest of Epidemic Disease: A Chapter in the History of Ideas. Hafner Publishing Co Ltd. ISBN 978-0028548807.
- Agramonte, A (2001). "The inside history of a great medical discovery. 1915". Military Medicine. 166 (9 Suppl): 68–78. doi:10.1093/milmed/166.suppl_1.68. PMID 11569397.
- Carter KC (January 1985). "Ignaz Semmelweis, Carl Mayrhofer, and the rise of germ theory". Medical History. 29 (1): 33–53. doi:10.1017/S0025727300043738. PMC 1139480. PMID 3883083.
- From p. 90 of "The invisible world revealed by the microscope or, thoughts on animalcules.", second edition, 1850 (May have appeared in first edition, too. (Revise date in article to 1846, if so.))
- Snow J (1849). On the Mode of Communication of Cholera. London: J. Churchill.
There is no doubt that the mortality was much diminished, as I said before, by the flight of the population, which commenced soon after the outbreak; but the attacks had so far diminished before the use of the water was stopped, that it is impossible to decide whether the well still contained the cholera poison in an active state, or whether, from some cause, the water had become free from it
- Chapelle F (2005). "Ch. 5: Hidden Life, Hidden Death". Wellsprings. New Brunswick NJ: Rutgers University Press. p. 82. ISBN 978-0-8135-3614-9.
- Pasteur L, Ernst HC (1880) [May 1880]. "(translated from French)" [On the extension of the germ theory to the etiology of certain common diseases]. Comptes Rendus de l'Académie des Sciences. Vol. XC. pp. 1033–44. Archived from the original on 8 September 2017. Retrieved 3 December 2012.
- Walker L, Levine H, Jucker M (July 2006). "Koch's postulates and infectious proteins". Acta Neuropathologica. 112 (1): 1–4. doi:10.1007/s00401-006-0072-x. PMC 8544537. PMID 16703338. S2CID 22210933.
- Koch R (1884). "Die Aetiologie der Tuberkulose". Mittheilungen aus dem Kaiserlichen Gesundheitsamte. Vol. 2. pp. 1–88.
- Koch R (1893). "Über den augenblicklichen Stand der bakteriologischen Choleradiagnose". Zeitschrift für Hygiene und Infektionskrankheiten (in German). 14: 319–33. doi:10.1007/BF02284324. S2CID 9388121.
- Brock TD (1999). Robert Koch: a life in medicine and bacteriology. Washington DC: American Society of Microbiology Press. ISBN 1-55581-143-4.
- Evans AS (May 1976). "Causation and disease: the Henle-Koch postulates revisited". The Yale Journal of Biology and Medicine. 49 (2): 175–195. PMC 2595276. PMID 782050.
- Jacomo V, Kelly PJ, Raoult D (January 2002). "Natural history of Bartonella infections (an exception to Koch's postulate)". Clinical and Diagnostic Laboratory Immunology. 9 (1): 8–18. doi:10.1128/CDLI.9.1.8-18.2002. PMC 119901. PMID 11777823.
- Falkow S (1988). "Molecular Koch's postulates applied to microbial pathogenicity" (PDF). Reviews of Infectious Diseases. 10 Suppl 2 (Suppl 2): S274–S276. doi:10.1093/cid/10.Supplement_2.S274. PMID 3055197. S2CID 13602080. Archived from the original (PDF) on 3 March 2019.
- Inglis TJ (November 2007). "Principia aetiologica: taking causality beyond Koch's postulates". Journal of Medical Microbiology. 56 (Pt 11): 1419–1422. doi:10.1099/jmm.0.47179-0. PMID 17965339.
External links
- Stephen T. Abedon Germ Theory of Disease Supplemental Lecture (98/03/28 update)
- William C. Campbell The Germ Theory Timeline
- Science's war on infectious diseases