Tretinoin
Tretinoin, also known as all-trans retinoic acid (ATRA), is a medication used for the treatment of acne and acute promyelocytic leukemia.[5][6][7] For acne, it is applied to the skin as a cream, gel or ointment.[7] For leukemia, it is taken by mouth for up to three months.[5] Topical tretinoin is also the most extensively investigated retinoid therapy for photoaging.[8]
 | |
| Clinical data | |
|---|---|
| Pronunciation | See pronunciation note |
| Trade names | Retin-a, Avita, Renova, others |
| Other names | ATRA |
| AHFS/Drugs.com | Monograph Topical Monograph |
| MedlinePlus | a608032 |
| License data |
|
| Pregnancy category | |
| Routes of administration | Topical, by mouth |
| ATC code | |
| Legal status | |
| Legal status | |
| Pharmacokinetic data | |
| Protein binding | > 95% |
| Elimination half-life | 0.5–2 hours |
| Identifiers | |
IUPAC name
| |
| CAS Number | |
| PubChem CID | |
| IUPHAR/BPS | |
| DrugBank | |
| ChemSpider | |
| UNII | |
| KEGG | |
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.005.573 |
| Chemical and physical data | |
| Formula | C20H28O2 |
| Molar mass | 300.442 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 180 °C (356 °F) |
| |
| |
| (verify) | |
Common side effects when used as a cream are limited to the skin and include skin redness, peeling, and sun sensitivity.[7] When used by mouth, side effects include shortness of breath, headache, numbness, depression, skin dryness, itchiness, hair loss, vomiting, muscle pains, and vision changes.[5] Other severe side effects include high white blood cell counts and blood clots.[5] Use during pregnancy is contraindicated due to the risk of birth defects.[5][1] It is in the retinoid family of medications.[6]
Tretinoin was patented in 1957, and approved for medical use in 1962.[9] It is on the World Health Organization's List of Essential Medicines.[10] Tretinoin is available as a generic medication.[11] In 2019, it was the 244th most commonly prescribed medication in the United States, with more than 1 million prescriptions.[12][13]
Medical uses
Skin use
Tretinoin is most commonly used to treat acne,[4] both inflammatory and noninflammatory. Multiple studies support the efficacy of topical retinoids in the treatment of acne vulgaris.[14][15] It is sometimes used in conjunction with other topical acne medications to enhance their penetration.[16] In addition to treating active acne, retinoids accelerate the resolution of acne-induced postinflammatory hyperpigmentation.[17] It is also useful as maintenance therapy for people who have responded to their initial treatment, reducing the prolonged use of antibiotics for acne.[18]
Leukemia
Tretinoin is used to induce remission in people with acute promyelocytic leukemia who have a mutation (the t(15;17) translocation 160 and/or the presence of the PML/RARα gene) and who do not respond to anthracyclines or cannot take that class of drug. It is not used for maintenance therapy.[3][19][20]
The evidence is very uncertain about the effect of tretinoin in addition to chemotherapy for patients with an acute myeloid leukemia on diarrhoea, nausea/vomiting and heart-related toxicity grades III/IV. Furthermore, tretinoin in addition to chemotherapy probably results in little to no difference in the mortality, relapse, progress, mortality during the trial and infections grade III/IV.[21]
Photoaging
Photoaging is premature skin aging resulting from prolonged and repeated exposure to solar radiation. Features of photoaging include fine and coarse wrinkles, change in skin pigmentation, and loss of elasticity. In human skin, topical retinoids increase collagen production, induce epidermal hyperplasia, and decrease keratinocyte and melanocyte atypia. Topical tretinoin is the most extensively investigated retinoid therapy for photoaging.[22] Topical tretinoin can be used for mild to severe photoaging in people of all skin types. Several weeks or months of use are typically required before improvement is appreciated. The benefits of topical tretinoin are lost upon discontinuation. Although it has only been studied for a duration of two years, it may be continued indefinitely. A long-term maintenance regimen with a lower concentration or less frequent application may be an alternative to continued use.[23]
Side effects
Skin use
Topical tretinoin is only for use on the skin and should not be applied to eyes or mucosal tissues. Common side effects include skin irritation, redness, swelling, and blistering.[4] If irritation is a problem, a decrease in the frequency of application to every other or every third night can be considered, and the frequency of application can be increased as tolerance improves. The fine skin flaking that is often seen can be gently exfoliated with a washcloth. A non-comedogenic facial moisturizer can also be applied if needed. Delaying application of the retinoid for at least 20 minutes after washing and drying the face may also be helpful. Topical retinoids are not true photosensitizing drugs, but people using topical retinoids have described symptoms of increased sun sensitivity. This is thought to be due to thinning of the stratum corneum leading to a decreased barrier against ultraviolet light exposure, as well as an enhanced sensitivity due to the presence of cutaneous irritation.[24]
Leukemia use
The oral form of the drug has boxed warnings concerning the risks of retinoic acid syndrome and leukocytosis.[3]
Other significant side effects include a risk of thrombosis, benign intracranial hypertension in children, high lipids (hypercholesterolemia and/or hypertriglyceridemia), and liver damage.[3]
There are many significant side effects from this drug that include malaise (66%), shivering (63%), hemorrhage (60%), infections (58%), peripheral edema (52%), pain (37%), chest discomfort (32%), edema (29%), disseminated intravascular coagulation (26%), weight increase (23%), injection site reactions (17%), anorexia (17%), weight decrease (17%), and myalgia (14%).[3]
Respiratory side effects usually signify retinoic acid syndrome, and include upper respiratory tract disorders (63%), dyspnea (60%), respiratory insufficiency (26%), pleural effusion (20%), pneumonia (14%), rales (14%), and expiratory wheezing (14%), and many others at less than 10%.[3]
Around 23% of people taking the drug have reported earache or a feeling of fullness in their ears.[3]
Gastrointestinal disorders include bleeding (34%), abdominal pain (31%), diarrhea (23%), constipation (17%), dyspepsia (14%), and swollen belly (11%) and many others at less than 10%.[3]
In the cardiovascular system, side effects include arrhythmias (23%), flushing (23%), hypotension (14%), hypertension (11%), phlebitis (11%), and cardiac failure (6%) and for 3% of patients: cardiac arrest, myocardial infarction, enlarged heart, heart murmur, ischemia, stroke, myocarditis, pericarditis, pulmonary hypertension, secondary cardiomyopathy.[3]
In the nervous system, side effects include dizziness (20%), paresthesias (17%), anxiety (17%), insomnia (14%), depression (14%), confusion (11%), and many others at less than 10% frequency.[3]
In the urinary system, side effects include chronic kidney disease (11%) and several others at less than 10% frequency.[3]
Mechanism of action
For its use in cancer, its mechanism of action is unknown, but on a cellular level, laboratory tests show that tretinoin forces APL cells to differentiate and stops them from proliferating; in people there is evidence that it forces the primary cancerous promyelocytes to differentiate into their final form, allowing normal cells to take over the bone marrow.[3] Recent study shows that ATRA inhibits and degrades active PIN1.[25]
For its use in acne, tretinoin (along with other retinoids) are vitamin A derivatives that act by binding to two nuclear receptor families within keratinocytes: the retinoic acid receptors (RAR) and the retinoid X receptors (RXR).[17] These events contribute to the normalization of follicular keratinization and decreased cohesiveness of keratinocytes, resulting in reduced follicular occlusion and microcomedone formation.[26] The retinoid-receptor complex competes for coactivator proteins of AP-1, a key transcription factor involved in inflammation.[17] Retinoids also down-regulate expression of toll-like receptor (TLR)-2, which has been implicated in the inflammatory response in acne.[27] Moreover, tretinoin and retinoids may enhance the penetration of other topical acne medications.[16]
The combination of the 10% benzoyl peroxide and light results in more than 50% degradation of tretinoin in about 2 hours and 95% in 24 hours.[28] This lack of stability in the presence of light and oxidizing agents has led to the development of novel formulations of the drug. When microencapsulated tretinoin is exposed to benzoyl peroxide and light only 1% degradation takes place in about 4 hours and only 13% after 24 hours.[29]
Biosynthesis
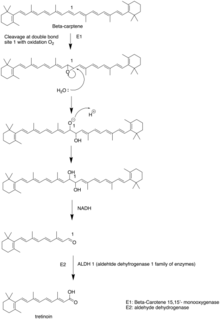
Tretinoin is synthesized from beta-carotene. The beta-carotene is firstly cleaved into beta-carotene 15-15'-monooxygenase through site 1 double bond oxidized to epoxide. The epoxide is attacked by water to form diol in site 1. NADH, as a reduction agent, reduce the alcohol group to aldehydes.[30]
History
Tretinoin was co-developed for its use in acne by James Fulton and Albert Kligman when they were at University of Pennsylvania in the 1960s.[31][32] Phase I trials, the first conducted on human subjects, were performed on inmates at Holmesburg Prison during a long-running regime of non-therapeutic and unethical testing on prison inmates at Holmesburg.[33][34] The University of Pennsylvania held the patent for Retin-A, which it licensed to pharmaceutical companies.[32]
Treatment of acute promyelocytic leukemia was first introduced at Ruijin Hospital in Shanghai by Wang Zhenyi in a 1988 clinical trial.[35]
Etymology
The origin of the name tretinoin is uncertain,[36][37] although several sources agree (one with probability,[36] one with asserted certainty[38]) that it probably comes from trans- + retinoic [acid] + -in, which is plausible given that tretinoin is the all-trans isomer of retinoic acid. The name isotretinoin is the same root tretinoin plus the prefix iso-. Regarding pronunciation, the following variants apply equally to both tretinoin and isotretinoin. Given that retinoic is pronounced /ˌrɛtɪˈnoʊɪk/,[37][38][39][40] it is natural that /ˌtrɛtɪˈnoʊɪn/ is a commonly heard pronunciation. Dictionary transcriptions also include /ˌtrɪˈtɪnoʊɪn/ (tri-TIN-oh-in)[37][39] and /ˈtrɛtɪnɔɪn/.[38][40]
Research
Tretinoin has been explored as a treatment for hair loss, potentially as a way to increase the ability of minoxidil to penetrate the scalp, but the evidence is weak and contradictory.[41][42]
It has been used off-label to treat and reduce the appearance of stretch marks.[43] It has also been studied in skin aging.[44]
References
- "Tretinoin (Vesanoid) Use During Pregnancy". Drugs.com. 25 July 2019. Retrieved 16 January 2020.
- "Tretinoin topical Use During Pregnancy". Drugs.com. 1 July 2019. Retrieved 16 January 2020.
- "Tretinoin capsule". DailyMed. 12 December 2018. Retrieved 16 January 2020.
- "Tretinoin Cream- tretinoin cream". DailyMed. 1 December 2018. Retrieved 16 January 2020.
- "Tretinoin". The American Society of Health-System Pharmacists. Archived from the original on 30 November 2016. Retrieved 8 December 2016.
- Tivnan A (2016). Resistance to Targeted Therapies Against Adult Brain Cancers. Springer. p. 123. ISBN 978-3-319-46505-0. Archived from the original on 5 November 2017.
- British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. pp. 627, 821–822. ISBN 978-0-85711-156-2.
- "Retinoids, topical". American Osteopathic College of Dermatology.
- Fischer J, Ganellin CR (2006). Analogue-based Drug Discovery. John Wiley & Sons. p. 476. ISBN 978-3-527-60749-5. Archived from the original on 5 November 2017.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- "Tretinoin topical". The American Society of Health-System Pharmacists. Archived from the original on 16 May 2016. Retrieved 8 December 2016.
- "The Top 300 of 2019". ClinCalc. Retrieved 16 October 2021.
- "Tretinoin – Drug Usage Statistics". ClinCalc. Retrieved 16 October 2021.
- Leyden JJ, Shalita A, Thiboutot D, Washenik K, Webster G (February 2005). "Topical retinoids in inflammatory acne: a retrospective, investigator-blinded, vehicle-controlled, photographic assessment". Clinical Therapeutics. 27 (2): 216–24. doi:10.1016/j.clinthera.2005.02.009. PMID 15811485.
- Webster G, Cargill DI, Quiring J, Vogelson CT, Slade HB (March 2009). "A combined analysis of 2 randomized clinical studies of tretinoin gel 0.05% for the treatment of acne". Cutis. 83 (3): 146–54. PMID 19363908.
- Gollnick H, Cunliffe W, Berson D, Dreno B, Finlay A, Leyden JJ, et al. (July 2003). "Management of acne: a report from a Global Alliance to Improve Outcomes in Acne". Journal of the American Academy of Dermatology. 49 (1 Suppl): S1-37. doi:10.1067/mjd.2003.618. PMID 12833004.
- Kang S, Voorhees JJ. Topical retinoids. In: Fitzpatrick's Dermatology in General Medicine, 7th ed, Wolff K, Goldsmith LA, Katz SI, et al (Eds), McGraw Hill, New York 2008. p.2106.
- Leyden, James; Stein-Gold, Linda; Weiss, Jonathan (5 June 2017). "Why Topical Retinoids Are Mainstay of Therapy for Acne". Dermatology and Therapy. 7 (3): 293–304. doi:10.1007/s13555-017-0185-2. ISSN 2193-8210. PMC 5574737. PMID 28585191.
- Huang ME, Ye YC, Chen SR, Chai JR, Lu JX, Zhoa L, et al. (August 1988). "Use of all-trans retinoic acid in the treatment of acute promyelocytic leukemia" (PDF). Blood. 72 (2): 567–72. doi:10.1182/blood.V72.2.567.567. PMID 3165295.
- Castaigne S, Chomienne C, Daniel MT, Ballerini P, Berger R, Fenaux P, Degos L (November 1990). "All-trans retinoic acid as a differentiation therapy for acute promyelocytic leukemia. I. Clinical results" (PDF). Blood. 76 (9): 1704–9. doi:10.1182/blood.V76.9.1704.1704. PMID 2224119.
- Küley-Bagheri Y, Kreuzer KA, Monsef I, Lübbert M, Skoetz N (August 2018). Cochrane Haematological Malignancies Group (ed.). "Effects of all-trans retinoic acid (ATRA) in addition to chemotherapy for adults with acute myeloid leukaemia (AML) (non-acute promyelocytic leukaemia (non-APL))". The Cochrane Database of Systematic Reviews. 2018 (8): CD011960. doi:10.1002/14651858.CD011960.pub2. PMC 6513628. PMID 30080246.
- Han A, Chien AL, Kang S (July 2014). "Photoaging". Dermatologic Clinics. 32 (3): 291–9, vii. doi:10.1016/j.det.2014.03.015. PMID 24891052.
- Kang S, Bergfeld W, Gottlieb AB, Hickman J, Humeniuk J, Kempers S, et al. (2005). "Long-term efficacy and safety of tretinoin emollient cream 0.05% in the treatment of photodamaged facial skin: a two-year, randomized, placebo-controlled trial". American Journal of Clinical Dermatology. 6 (4): 245–53. doi:10.2165/00128071-200506040-00005. PMID 16060712. S2CID 40127961.
- Zaenglein AL (September 2008). "Topical retinoids in the treatment of acne vulgaris". Seminars in Cutaneous Medicine and Surgery. 27 (3): 177–82. doi:10.1016/j.sder.2008.06.001. PMID 18786495.
- Wei S, Kozono S, Kats L, Nechama M, Li W, Guarnerio J, et al. (May 2015). "Active Pin1 is a key target of all-trans retinoic acid in acute promyelocytic leukemia and breast cancer". Nature Medicine. 21 (5): 457–66. doi:10.1038/nm.3839. PMC 4425616. PMID 25849135.
- Fernandez [Graber] EM, Zaenglein A, Thiboutot D. Acne Treatment Methodologies. In: Cosmetic Formulation of Skin Care Products, Taylor and Francis Group, New York 2006. p.273.
- Liu PT, Krutzik SR, Kim J, Modlin RL (March 2005). "Cutting edge: all-trans retinoic acid down-regulates TLR2 expression and function". Journal of Immunology. 174 (5): 2467–70. doi:10.4049/jimmunol.174.5.2467. PMID 15728448. S2CID 20740543.
- Martin; Meunier; Montels; Watts (1998). "Chemical stability of adapalene and tretinoin when combined with benzoyl peroxide in presence and in absence of visible light and ultraviolet radiation". British Journal of Dermatology. Wiley. 139 (s52): 8–11. doi:10.1046/j.1365-2133.1998.1390s2008.x. ISSN 0007-0963. PMID 9990414. S2CID 43287596.
- "The Stability of Tretinoin in Tretinoin Gel Microsphere 0.1%". www.mdedge.com. Retrieved 14 May 2021.
- Woggon, Wolf-D. (1 January 2002). "Oxidative cleavage of carotenoids catalyzed by enzyme models and beta-carotene 15,15´-monooxygenase". Pure and Applied Chemistry. 74 (8): 1397–1408. doi:10.1351/pac200274081397.
- Vivant Pharmaceuticals, LLC Press Release. 10 July 2013, Vivant Skin Care Co-founder James E. Fulton, MD, Loses Colon Cancer Battle
- Gellene D (22 February 2010). "Dr. Albert M. Kligman, Dermatologist, Dies at 93". The New York Times.
- Washington, Harriet A. (2006). Medical apartheid : the dark history of medical experimentation on Black Americans from colonial times to the present. New York: Doubleday. ISBN 0-385-50993-6. OCLC 61131882.
- Hornblum, Allen M. (1998). Acres of skin : human experiments at Holmesburg Prison : a story of abuse and exploitation in the name of medical science. New York: Routledge. ISBN 0-415-91990-8. OCLC 37884781.
- Huang ME, Ye YC, Chen SR, Chai JR, Lu JX, Zhoa L, et al. (August 1988). "Use of all-trans retinoic acid in the treatment of acute promyelocytic leukemia". Blood. 72 (2): 567–72. doi:10.1182/blood.V72.2.567.567. PMID 3165295.
- Merriam-Webster, Merriam-Webster's Unabridged Dictionary, Merriam-Webster.
- Oxford Dictionaries, Oxford Dictionaries Online, Oxford University Press, archived from the original on 22 October 2014.
- Houghton Mifflin Harcourt, The American Heritage Dictionary of the English Language, Houghton Mifflin Harcourt, archived from the original on 25 September 2015, retrieved 24 January 2015.
- Merriam-Webster, Merriam-Webster's Medical Dictionary, Merriam-Webster.
- Elsevier, Dorland's Illustrated Medical Dictionary, Elsevier.
- Ralph M. Trüeb. The Difficult Hair Loss Patient: Guide to Successful Management of Alopecia and Related Conditions. Springer, 2015. ISBN 9783319197012 Pg. 95 Archived 5 November 2017 at the Wayback Machine
- Rogers NE, Avram MR (October 2008). "Medical treatments for male and female pattern hair loss". Journal of the American Academy of Dermatology. 59 (4): 547–66, quiz 567–8. doi:10.1016/j.jaad.2008.07.001. PMID 18793935.
- Arthur W. Perry (2007). Straight talk about cosmetic surgery. Yale University Press. pp. 63. ISBN 978-0-300-12104-9.
- Mukherjee S, Date A, Patravale V, Korting HC, Roeder A, Weindl G (December 2006). "Retinoids in the treatment of skin aging: an overview of clinical efficacy and safety". Clinical Interventions in Aging. 1 (4): 327–48. doi:10.2147/ciia.2006.1.4.327. PMC 2699641. PMID 18046911.
External links
- "Tretinoin". Drug Information Portal. U.S. National Library of Medicine.
- "Tretinoin Topical". MedlinePlus.