Retinol
Retinol, also called vitamin A1, is a fat-soluble vitamin in the vitamin A family[1] found in food and used as a dietary supplement.[2] As a supplement it is used to treat and prevent vitamin A deficiency, especially that which results in xerophthalmia.[1] In regions where deficiency is common, a single large dose is recommended to those at high risk twice a year.[3] It is also used to reduce the risk of complications in measles patients.[3] It is taken by mouth or by injection into a muscle.[1]
 | |
 Retinol | |
| Clinical data | |
|---|---|
| AHFS/Drugs.com | Monograph |
| License data |
|
| Routes of administration | by mouth, IM[1] |
| Drug class | vitamin |
| ATC code | |
| Legal status | |
| Legal status |
|
| Identifiers | |
IUPAC name
| |
| CAS Number |
|
| PubChem CID | |
| IUPHAR/BPS | |
| ChemSpider | |
| UNII |
|
| ChEBI | |
| ChEMBL | |
| CompTox Dashboard (EPA) | |
| ECHA InfoCard | 100.000.621 |
| Chemical and physical data | |
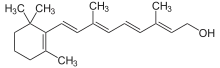
| Formula | C20H30O |
| Molar mass | 286.4516 g·mol−1 |
| 3D model (JSmol) | |
| Melting point | 62–64 °C (144–147 °F) |
| Boiling point | 137–138 °C (279–280 °F) (10−6 mm Hg) |
| |
| |
Retinol at normal doses is well tolerated.[1] High doses may cause enlargement of the liver, dry skin, and hypervitaminosis A.[1][4] High doses during pregnancy may harm the fetus.[1] The body converts retinol to retinal and retinoic acid, through which it acts.[2] Dietary sources include fish, dairy products, and meat.[2]
Retinol was discovered in 1909, isolated in 1931, and first made in 1947.[5][6] It is on the World Health Organization's List of Essential Medicines.[7] Retinol is available as a generic medication and over the counter.[1]
Medical uses
Retinol is used to treat vitamin A deficiency.
Three approaches may be used when populations have low vitamin A levels:[8]
- Through dietary modification involving the adjustment of menu choices of affected persons from available food sources to optimize vitamin A content.
- Enriching commonly eaten and affordable foods with vitamin A, a process called fortification. It involves addition of synthetic vitamin A to staple foods like margarine, bread, flours, cereals, and infant formula during processing.
- By giving high-doses of vitamin A to the targeted deficient population, a method known as supplementation.
Side effects
The Tolerable Upper Intake Level (UL) for vitamin A, for a 25-year-old man, is 3,000 micrograms/day, or about 10,000 IU. In breastfeeding mothers, vitamin A intake should be 1,200 to 1,300 retinol activity units (RAE).[9]
Too much vitamin A in retinoid form can be harmful. The body converts the dimerized form, carotene, into vitamin A as it is needed, so high levels of carotene are not toxic, whereas the ester (animal) forms are. The livers of certain animals, especially those adapted to polar environments, such as polar bears and seals,[10] often contain amounts of vitamin A that would be toxic to humans. Thus, vitamin A toxicity is typically reported in Arctic explorers and people taking large doses of synthetic vitamin A. The first documented death possibly caused by vitamin A poisoning was that of Xavier Mertz, a Swiss scientist, who died in January 1913 on an Antarctic expedition that had lost its food supplies and fell to eating its sled dogs. Mertz may have consumed lethal amounts of vitamin A by eating the dogs' livers.[11]
Vitamin A acute toxicity occurs when a person ingests vitamin A in large amounts more than the daily recommended value in the threshold of 25,000 IU/kg or more. Often, the patient consumes about 3–4 times the RDA's specification.[12] Toxicity of vitamin A is believed to be associated with the methods of increasing vitamin A in the body, such as food modification, fortification, and supplementation, all of which are used to combat vitamin A deficiency.[13] Toxicity is classified into two categories: acute and chronic. The former occurs a few hours or days after ingestion of a large amount of vitamin A. Chronic toxicity takes place when about 4,000 IU/kg or more of vitamin A is consumed for a long time. Symptoms of both include nausea, blurred vision, fatigue, weight-loss, and menstrual abnormalities.[14]
Excess vitamin A is suspected to be a contributor to osteoporosis. This seems to happen at much lower doses than those required to induce acute intoxication. Only preformed vitamin A can cause these problems, because the conversion of carotenoids into vitamin A is downregulated when physiological requirements are met; but excessive uptake of carotenoids can cause carotenosis.
Excess preformed vitamin A during early pregnancy is associated with a significant increase in birth defects.[15] These defects may be severe, even life-threatening. Even twice the daily recommended amount can cause severe birth defects.[16] The FDA recommends that pregnant women get their vitamin A from foods containing beta carotene and that they ensure that they consume no more than 5,000 IU of preformed vitamin A (if any) per day. Although vitamin A is necessary for fetal development, most women carry stores of vitamin A in their fat cells, so over-supplementation should be strictly avoided.
A review of all randomized controlled trials in the scientific literature by the Cochrane Collaboration published in JAMA in 2007 found that supplementation with beta carotene or vitamin A increased mortality by 5% and 16%, respectively.[17]
Studies emerging from developing countries India, Bangladesh, and Indonesia strongly suggest that, in populations in which vitamin A deficiency is common and maternal mortality is high, dosing expectant mothers can greatly reduce maternal mortality.[18] Similarly, dosing newborn infants with 50,000 IU (15 mg) of vitamin A within two days of birth can significantly reduce neonatal mortality.[19][20]
Biological roles
Retinol or other forms of vitamin A are needed for eyesight, maintenance of the skin, and human development.[1] Other than for vision, the active compound is all-trans-retinoic acid, synthesized from retinal, in turn synthesized from retinol.
Embryology
Retinoic acid via the retinoic acid receptor influences the process of cell differentiation, hence, the growth and development of embryos. During development, there is a concentration gradient of retinoic acid along the anterior-posterior (head-tail) axis. Cells in the embryo respond to retinoic acid differently depending on the amount present. For example, in vertebrates, the hindbrain transiently forms eight rhombomeres and each rhombomere has a specific pattern of genes being expressed. If retinoic acid is not present the last four rhombomeres do not develop. Instead, rhombomeres 1–4 grow to cover the same amount of space as all eight would normally occupy. Retinoic acid has its effects by turning on a differential pattern of Homeobox (Hox) genes that encode different homeodomain transcription factors which in turn can turn on cell type specific genes. Deletion of the Homeobox (Hox-1) gene from rhombomere 4 makes the neurons growing in that region behave like neurons from rhombomere 2. Retinoic acid is not required for patterning of the retina as originally proposed, but retinoic acid synthesized in the retina is secreted into surrounding mesenchyme where it is required to prevent overgrowth of perioptic mesenchyme which can cause microphthalmia, defects in the cornea and eyelid, and rotation of the optic cup.[21]
Stem cell biology
Retinoic acid is an influential factor used in differentiation of stem cells to more committed fates, echoing retinoic acid's importance in natural embryonic developmental pathways. It is thought to initiate differentiation into a number of different cell lineages by unsequestering certain sequences in the genome.
It has numerous applications in the experimental induction of stem cell differentiation; amongst these are the differentiation of human embryonic stem cells to posterior foregut lineages and also to functional motor neurons.
Vision
Retinol is an essential compound in the cycle of light-activated chemical reactions called the "visual cycle" that underlies vertebrate vision. Retinol is converted by the protein RPE65 within the pigment epithelium of the retina into 11-cis-retinal. This molecule is then transported into the retina's photoreceptor cells (the rod or cone cells in mammals) where it binds to an opsin protein and acts as a light-activated molecular switch. When 11-cis-retinal absorbs light it isomerizes into all-trans-retinal. The change in the shape of the molecule in turn changes the configuration of the opsin in a cascade that leads to the neuronal firing, which signals the detection of light.[22] The opsin then splits into the protein component (such metarhodopsin) and the cofactor all-trans-retinal. The regeneration of active opsin requires conversion of all-trans-retinal back to 11-cis-retinal via retinol. The regeneration of 11-cis-retinal occurs in vertebrates via conversion of all-trans-retinol to 11-cis-retinol in a sequence of chemical transformations that occurs primarily in the pigment epithelial cells.
Without adequate amounts of retinol, regeneration of rhodopsin is incomplete and night blindness occurs. Night blindness, the inability to see well in dim light, is associated with a deficiency of vitamin A, a class of compounds that includes retinol and retinal. In the early stages of vitamin A deficiency, the more light-sensitive and abundant rods, which have rhodopsin, have impaired sensitivity, and the cone cells are less affected. The cones are less abundant than rods and come in three types, each contains its own type of iodopsin, the opsins of the cones. The cones mediate color vision, and vision in bright light (day vision).
Glycoprotein synthesis
Glycoprotein synthesis requires adequate vitamin A status. In severe vitamin A deficiency, lack of glycoproteins may lead to corneal ulcers or liquefaction.[23]
Immune system
Vitamin A is essential to maintain intact epithelial tissues as a physical barrier to infection; it is also involved in maintaining a number of immune cell types from both the innate and acquired immune systems.[24] These include the lymphocytes (B-cells, T-cells, and natural killer cells), as well as many myelocytes (neutrophils, macrophages, and myeloid dendritic cells).
Skin
Deficiencies in vitamin A have been linked to an increased susceptibility to skin infection and inflammation.[25] Vitamin A appears to modulate the innate immune response and maintains homeostasis of epithelial tissues and mucosa through its metabolite, retinoic acid (RA). As part of the innate immune system, toll-like receptors in skin cells respond to pathogens and cell damage by inducing a pro-inflammatory immune response which includes increased RA production.[25] The epithelium of the skin encounters bacteria, fungi and viruses. Keratinocytes of the epidermal layer of the skin produce and secrete antimicrobial peptides (AMPs). Production of AMPs resistin and cathelicidin, are promoted by RA.[25] Another way that vitamin A helps maintain a healthy skin and hair follicle microbiome, especially on the face, is by reduction of sebum secretion, which is a nutrient source for bacteria.[25]
Red blood cells
Vitamin A may be needed for normal red blood cell formation;[26][27] deficiency causes abnormalities in iron metabolism.[28] Vitamin A is needed to produce the red blood cells from stem cells through retinoid differentiation.[29]
Units of measurement
When referring to dietary allowances or nutritional science, retinol is usually measured in international units (IU). IU refers to biological activity and therefore is unique to each individual compound, however 1 IU of retinol is equivalent to approximately 0.3 micrograms (300 nanograms).
Nutrition
| Vitamin properties | |
|---|---|
| Solubility | Fat |
| RDA (adult male) | 900 µg/day |
| RDA (adult female) | 700 µg/day |
| RDA upper limit (adult male) | 3,000 µg/day |
| RDA upper limit (adult female) | 3,000 µg/day |
| Deficiency symptoms | |
| |
| Excess symptoms | |
| |
| Common sources | |
| |
This vitamin plays an essential role in vision, particularly night vision, normal bone and tooth development, reproduction, and the health of skin and mucous membranes (the mucus-secreting layer that lines body regions such as the respiratory tract). Vitamin A also acts in the body as an antioxidant, a protective chemical that may reduce the risk of certain cancers.
There are two sources of dietary vitamin A. Active forms, which are immediately available to the body are obtained from animal products. These are known as retinoids and include retinaldehyde and retinol. Precursors, also known as provitamins, which must be converted to active forms by the body, are obtained from fruits and vegetables containing yellow, orange and dark green pigments, known as carotenoids, the most well-known being β-carotene. For this reason, amounts of vitamin A are measured in Retinol Equivalents (RE). One RE is equivalent to 0.001 mg of retinol, or 0.006 mg of β-carotene, or 3.3 International Units of vitamin A.
In the intestine, vitamin A is protected from being chemically changed by vitamin E. Vitamin A is fat-soluble and can be stored in the body. Most of the vitamin A consumed is stored in the liver. When required by a particular part of the body, the liver releases some vitamin A, which is carried by the blood and delivered to the target cells and tissues.
Dietary intake
The Dietary Reference Intake (DRI) Recommended Daily Amount (RDA) for vitamin A for a 25-year-old male is 900 micrograms/day, or 3000 IU. National Health Service daily recommended values are slightly lower at 700 micrograms for men and 600 micrograms for women.[30]
During the absorption process in the intestines, retinol is incorporated into chylomicrons as the ester form, and it is these particles that mediate transport to the liver. Liver cells store vitamin A as the ester, and when retinol is needed in other tissues, it is de-esterifed and released into the blood as the alcohol. Retinol then attaches to a serum carrier, retinol binding protein, for transport to target tissues. A binding protein inside cells, cellular retinoic acid binding protein, serves to store and move retinoic acid intracellularly.
Deficiency
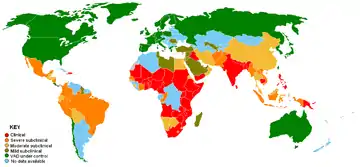
Vitamin A deficiency is common in developing countries but rarely seen in developed countries. Approximately 250,000 to 500,000 malnourished children in the developing world go blind each year from a deficiency of vitamin A.[31] Vitamin A deficiency in expecting mothers increases the mortality rate of children shortly after childbirth.[32] Night blindness is one of the first signs of vitamin A deficiency. Vitamin A deficiency contributes to blindness by making the cornea very dry and damaging the retina and cornea.[33]
Chemistry
Many different geometric isomers of retinol, retinal and retinoic acid are possible as a result of either a trans or cis configuration of four of the five double bonds found in the polyene chain. The cis isomers are less stable and can readily convert to the all-trans configuration (as seen in the structure of all-trans-retinol shown at the top of this page). Nevertheless, some cis isomers are found naturally and carry out essential functions. For example, the 11-cis-retinal isomer is the chromophore of rhodopsin, the vertebrate photoreceptor molecule. Rhodopsin is composed of the 11-cis-retinal covalently linked via a Schiff base to the opsin protein (either rod opsin or blue, red or green cone opsins). The process of vision relies on the light-induced isomerisation of the chromophore from 11-cis to all-trans resulting in a change of the conformation and activation of the photoreceptor molecule. One of the earliest signs of vitamin A deficiency is night-blindness followed by decreased visual acuity.
Many of the non-visual functions of vitamin A are mediated by retinoic acid, which regulates gene expression by activating nuclear retinoic acid receptors.[21] The non-visual functions of vitamin A are essential in the immunological function, reproduction and embryonic development of vertebrates as evidenced by the impaired growth, susceptibility to infection and birth defects observed in populations receiving suboptimal vitamin A in their diet.
Synthesis
Biosynthesis
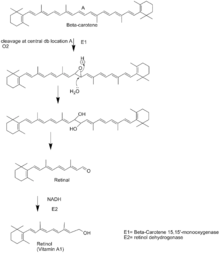
Retinol is synthesized from the breakdown of β-carotene. First, the β-carotene 15-15'-monooxygenase cleaves β-carotene at the central double bond, creating an epoxide. This epoxide is then attacked by water creating two hydroxyl groups in the center of the structure. The cleavage occurs when these alcohols are oxidized to the aldehydes using NADH. This compound is called retinal. Retinal is then reduced to retinol by the enzyme retinol dehydrogenase. Retinol dehydrogenase is an enzyme that is dependent on NADH.[35]
Industrial synthesis
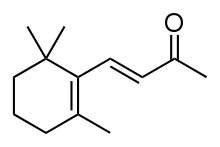
β-carotene can be extracted from fungus Blakeslea trispora, marine algae Dunaliella salina or genetically modified bacteria of the genus Sphingomonas, or else via total synthesis using either a method developed by BASF[36][37] or a Grignard reaction utilized by Hoffman-La Roche.[38]
The world market for synthetic retinol is primarily for animal feed, leaving approximately 13% for a combination of food, prescription medication and dietary supplement use.[39] The first industrialized synthesis of retinol was achieved by the company Hoffmann-La Roche in 1947. In the following decades, eight other companies developed their own processes. β-ionone, synthesized from acetone, is the essential starting point for all industrial syntheses. Each process involves elongating the unsaturated carbon chain.[39] Pure retinol is extremely sensitive to oxidization and is prepared and transported at low temperatures and oxygen-free atmospheres. When prepared as a dietary supplement or food additive, retinol is stabilized as the ester derivatives retinyl acetate or retinyl palmitate. Prior to 1999, three companies, Roche, BASF and Rhone-Poulenc controlled 96% of global vitamin A sales. In 2001, the European Commission imposed total fines of 855.22 Euros on these and five other companies for their participation in eight distinct market-sharing and price-fixing cartels that dated back to 1989. Roche sold its vitamin division to DSM in 2003. DSM and BASF have the major share of industrial production.[39]
History
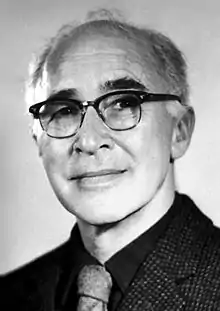
In 1912, Frederick Gowland Hopkins demonstrated that unknown accessory factors found in milk, other than carbohydrates, proteins, and fats were necessary for growth in rats. Hopkins received a Nobel Prize for this discovery in 1929.[40] One year later, Elmer McCollum, a biochemist at the University of Wisconsin–Madison, and colleague Marguerite Davis identified a fat-soluble nutrient in butterfat and cod liver oil. Their work confirmed that of Thomas Burr Osborne and Lafayette Mendel, at Yale, also in 1913, which suggested a fat-soluble nutrient in butterfat.[41] The "accessory factors" were termed "fat soluble" in 1918 and later "vitamin A" in 1920. In 1931, Swiss chemist Paul Karrer described the chemical structure of vitamin A.[40] Retinoic acid and retinol were first synthesized in 1946 and 1947 by two Dutch chemists, David Adriaan van Dorp and Jozef Ferdinand Arens.[42][43]
In 1967, George Wald was a co-recipient of the Nobel Prize in Physiology and Medicine "..."for their discoveries concerning the primary physiological and chemical visual processes in the eye."[44] Photoreceptor cells in the eye contain a chromophore composed of the protein opsin and 11-cis retinal. When struck by light, 11-cis retinal undergoes photoisomerization to all-trans retinal and via signal transduction cascade send a nerve signal to the brain. The all-trans retinal is reduced to all-trans retinol and travels back to the retinal pigment epithelium to be recycled to 11-cis retinal and conjugated to opsin.[45]
Although vitamin A was not confirmed as an essential nutrient and a chemical structure described until the 20th century, written observations of conditions created by deficiency of this nutrient appeared much earlier in history. Sommer classified historical accounts related to vitamin A and/or manifestations of deficiency as follows: "ancient" accounts; 18th- to 19th-century clinical descriptions (and their purported etiologic associations); early 20th-century laboratory animal experiments, and clinical and epidemiologic observations that identified the existence of this unique nutrient and manifestations of its deficiency.[18]
References
- "Vitamin A". The American Society of Health-System Pharmacists. Archived from the original on 30 December 2016. Retrieved 8 December 2016.
- "Office of Dietary Supplements - Vitamin A". ods.od.nih.gov. 31 August 2016. Archived from the original on 12 December 2016. Retrieved 30 December 2016.
- World Health Organization (2009). Stuart MC, Kouimtzi M, Hill SR (eds.). WHO Model Formulary 2008. World Health Organization. p. 500. hdl:10665/44053. ISBN 9789241547659.
- British national formulary : BNF 69 (69 ed.). British Medical Association. 2015. p. 701. ISBN 9780857111562.
- Squires VR (2011). The Role of Food, Agriculture, Forestry and Fisheries in Human Nutrition. Vol. IV. EOLSS Publications. p. 121. ISBN 9781848261952. Archived from the original on 5 November 2017.
- Ullmann's Food and Feed, 3 Volume Set. John Wiley & Sons. 2016. p. Chapter 2. ISBN 9783527695522. Archived from the original on 5 November 2017.
- World Health Organization (2019). World Health Organization model list of essential medicines: 21st list 2019. Geneva: World Health Organization. hdl:10665/325771. WHO/MVP/EMP/IAU/2019.06. License: CC BY-NC-SA 3.0 IGO.
- Schultink W (September 2002). "Use of under-five mortality rate as an indicator for vitamin A deficiency in a population". The Journal of Nutrition. 132 (9 Suppl): 2881S–2883S. doi:10.1093/jn/132.9.2881S. PMID 12221264.
- "Vitamin A: Fact Sheet for Health Professionals". National Institutes of Health. October 2018.
- Rodahl K, Moore T (July 1943). "The vitamin A content and toxicity of bear and seal liver". The Biochemical Journal. 37 (2): 166–168. doi:10.1042/bj0370166. PMC 1257872. PMID 16747610.
- Nataraja A. "Man's best friend? (An account of Mertz's illness)". Archived from the original on 29 January 2007.
- Gropper SS, Smith JL, Groff JL (2009). Advanced Nutrition and Human Metabolism (5th ed.). pp. 373–1182.
- Thompson J, Manore M (2005). "Ch. 8: Nutrients involved in antioxidant function". Nutrition: An Applied Approach. Pearson Education Inc. pp. 276–283.
- Mohsen SE, Mckinney K, Shanti MS (2008). "Vitamin A toxicity". Medscape. Archived from the original on 23 July 2013.
- Challem J (1995). "Caution Urged With Vitamin A in Pregnancy: But Beta-Carotene is Safe". The Nutrition Reporter Newsletter. Archived from the original on 1 September 2004.
- Stone B (6 October 1995). "Vitamin A and Birth Defects". United States FDA. Archived from the original on 4 February 2004.
- Bjelakovic G, Nikolova D, Gluud LL, Simonetti RG, Gluud C (February 2007). "Mortality in randomized trials of antioxidant supplements for primary and secondary prevention: systematic review and meta-analysis" (PDF). JAMA. 297 (8): 842–857. doi:10.1001/jama.297.8.842. PMID 17327526. Archived (PDF) from the original on 4 February 2016.
- Sommer A (October 2008). "Vitamin a deficiency and clinical disease: an historical overview". The Journal of Nutrition. 138 (10): 1835–1839. doi:10.1093/jn/138.10.1835. PMID 18806089.
- Tielsch JM, Rahmathullah L, Thulasiraj RD, Katz J, Coles C, Sheeladevi S, et al. (November 2007). "Newborn vitamin A dosing reduces the case fatality but not incidence of common childhood morbidities in South India". The Journal of Nutrition. 137 (11): 2470–2474. doi:10.1093/jn/137.11.2470. PMID 17951487.
- Klemm RD, Labrique AB, Christian P, Rashid M, Shamim AA, Katz J, et al. (July 2008). "Newborn vitamin A supplementation reduced infant mortality in rural Bangladesh". Pediatrics. 122 (1): e242–e250. doi:10.1542/peds.2007-3448. PMID 18595969. S2CID 27427577.
- Duester G (September 2008). "Retinoic acid synthesis and signaling during early organogenesis". Cell. 134 (6): 921–931. doi:10.1016/j.cell.2008.09.002. PMC 2632951. PMID 18805086.
- Purves, D; Augustine, GJ; Fitzpatrick, D; Katz, LC; LaMantia, AS; McNamara, JO; Williams, SM (2001). "Phototransduction". Neuroscience. 2nd Edition.
- Starck T (1997). "Severe Corneal Ulcerations and Vitamin A Deficiency". Advances in Corneal Research. Springer, Boston, MA. p. 558. doi:10.1007/978-1-4615-5389-2_46. ISBN 978-1-4613-7460-2.
- "Vitamin A directs immune cells to intestines". ScienceDaily. Retrieved 17 March 2020.
- Roche FC, Harris-Tryon TA (January 2021). "Illuminating the Role of Vitamin A in Skin Innate Immunity and the Skin Microbiome: A Narrative Review". Nutrients. 13 (2): 302. doi:10.3390/nu13020302. PMC 7909803. PMID 33494277.
- Oren T, Sher JA, Evans T (November 2003). "Hematopoiesis and retinoids: development and disease". Leukemia & Lymphoma. 44 (11): 1881–1891. doi:10.1080/1042819031000116661. PMID 14738139. S2CID 11348076.
- Evans T (September 2005). "Regulation of hematopoiesis by retinoid signaling". Experimental Hematology. 33 (9): 1055–1061. doi:10.1016/j.exphem.2005.06.007. PMID 16140154.
- García-Casal MN, Layrisse M, Solano L, Barón MA, Arguello F, Llovera D, et al. (March 1998). "Vitamin A and beta-carotene can improve nonheme iron absorption from rice, wheat and corn by humans". The Journal of Nutrition. 128 (3): 646–650. doi:10.1093/jn/128.3.646. PMID 9482776.
- "Carotenoid Oxygenase". InterPro. Retrieved 7 November 2018.
- Vitamins and minerals – Vitamin A – NHS Choices Archived 2013-09-23 at the Wayback Machine. Nhs.uk (2012-11-26). Retrieved on 2013-09-19.
- "Micronutrient deficiencies - Vitamin A deficiency". World Health Organization. 18 April 2018. Retrieved 18 April 2018.
- Akhtar S, Ahmed A, Randhawa MA, Atukorala S, Arlappa N, Ismail T, Ali Z (December 2013). "Prevalence of vitamin A deficiency in South Asia: causes, outcomes, and possible remedies". Journal of Health, Population, and Nutrition. 31 (4): 413–423. doi:10.3329/jhpn.v31i4.19975. PMC 3905635. PMID 24592582.
- Sommer A (February 1994). "Vitamin A: its effect on childhood sight and life". Nutrition Reviews. 52 (2 Pt 2): S60–S66. doi:10.1111/j.1753-4887.1994.tb01388.x. PMID 8202284.
- Brown, J. E. (2002). Vitamins and Your Health. Nutrition Now. 3rd ed., pp. 20–1 to 20–20.
- Dewick, Paul M. (2009), Medicinal Natural Products, Wiley, ISBN 0470741678.
- Wittig G.; Pommer H.: DBP 954247, 1956
- Wittig G.; Pommer H. (1959). Chem. Abstr. 53: 2279
- US 2609396, Inhoffen Hans Herloff & Pommer Horst, "Compounds with the carbon skeleton of beta-carotene and process for the manufacture thereof", published 1952-09-02
- Parker GL, Smith LK, Baxendale IR (February 2016). "Development of the industrial synthesis of vitamin A". Tetrahedron. 72 (13): 1645–52. doi:10.1016/j.tet.2016.02.029.
- Semba RD (2012). "On the 'discovery' of vitamin A". Annals of Nutrition & Metabolism. 61 (3): 192–198. doi:10.1159/000343124. PMID 23183288. S2CID 27542506.
- Semba RD (April 1999). "Vitamin A as "anti-infective" therapy, 1920-1940". The Journal of Nutrition. 129 (4): 783–791. doi:10.1093/jn/129.4.783. PMID 10203551.
- Arens JF, Van Dorp DA (February 1946). "Synthesis of some compounds possessing vitamin A activity". Nature. 157 (3981): 190–191. Bibcode:1946Natur.157..190A. doi:10.1038/157190a0. PMID 21015124. S2CID 27157783.
- Van Dorp DA, Arens JF (August 1947). "Synthesis of vitamin A aldehyde". Nature. 159 (4058): 189. Bibcode:1947Natur.160..189V. doi:10.1038/160189a0. PMID 20256189. S2CID 4137483.
- "The Nobel Prize in Physiology or Medicine 1967". Nobel Foundation. Archived from the original on 4 December 2013. Retrieved 28 July 2007.
- Ebrey T, Koutalos Y (January 2001). "Vertebrate photoreceptors". Progress in Retinal and Eye Research. 20 (1): 49–94. doi:10.1016/S1350-9462(00)00014-8. PMID 11070368. S2CID 2789591.
External links
- Jane Higdon, "Vitamin A", Micronutrient Information Center, Linus Pauling Institute, Oregon State University
- NIH Office of Dietary Supplements – Vitamin A
- Vitamin A Deficiency at the Merck Manual of Diagnosis and Therapy
- WHO publications on Vitamin A Deficiency
- "Retinol". Drug Information Portal. U.S. National Library of Medicine.