Addiction
Addiction is a neuropsychological disorder characterized by a persistent and intense urge to engage in certain behaviors, often usage of a drug, despite substantial harm and other negative consequences. Repetitive drug use often alters brain function in ways that perpetuate craving, and weakens (but does not completely negate) self-control.[6] This phenomenon – drugs reshaping brain function – has led to an understanding of addiction as a brain disorder with a complex variety of psychosocial as well as neurobiological (and thus involuntary)[lower-alpha 1] factors that are implicated in addiction's development.[3][7][8] Classic signs of addiction include compulsive engagement in rewarding stimuli, preoccupation with substances or behavior, and continued use despite negative consequences. Habits and patterns associated with addiction are typically characterized by immediate gratification (short-term reward),[9][10] coupled with delayed deleterious effects (long-term costs).[7][11]
| Addiction | |
|---|---|
| Other names | Severe substance use disorder[1][2] |
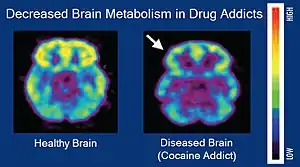 | |
| Brain positron emission tomography images that compare brain metabolism in a healthy individual and an individual with a cocaine addiction | |
| Specialty | Psychiatry, clinical psychology, toxicology, addiction medicine |
| Addiction and dependence glossary[3][4][5][2] | |
|---|---|
| |
Examples of drug and behavioral addictions include alcoholism, marijuana addiction, amphetamine addiction, cocaine addiction, nicotine addiction, opioid addiction, video game addiction, gambling addiction, eating or food addiction, pornography addiction and sexual addiction. The only behavioral addiction recognized by the DSM-5 and the ICD-10 is gambling addiction. With the introduction of the ICD-11 gaming addiction was appended.[12] The term "addiction" is frequently misused when referring to other compulsive behaviors or disorders, particularly dependence, in news media.[13] An important distinction between drug addiction and dependence is that drug dependence is a disorder in which cessation of drug use results in an unpleasant state of withdrawal, which can lead to further drug use.[14] Addiction is the compulsive use of a substance or performance of a behavior that is independent of withdrawal. Addiction can occur in the absence of dependence, and dependence can occur in the absence of addiction, although the two often occur together.
Behavioral addiction
The term "behavioral addiction" refers to a compulsion to engage in a natural reward – which is a behavior that is inherently rewarding (i.e., desirable or appealing) – despite adverse consequences.[10][15][16] Preclinical evidence has demonstrated that marked increases in the expression of ΔFosB through repetitive and excessive exposure to a natural reward induces the same behavioral effects and neuroplasticity as occurs in a drug addiction.[15][17][18][19]
Sexual Addiction
Sexual addiction involves an engagement in excessive, compulsive, or otherwise problematic sexual behaviour that persists despite negative physiological, psychological, social, and occupational consequences.[20] Sexual addiction may also be referred to as hypersexuality or compulsive sexual behaviour disorder.[20] The DSM-5 does not recognize sexual addiction as a clinical diagnosis despite proposals to include this diagnosis in its fifth edition, citing insufficient evidence supporting the existence of sexual addiction as a discrete mental health condition.[21] Reviews of both clinical research in humans and preclinical studies involving ΔFosB have identified compulsive sexual activity – specifically, any form of sexual intercourse – as an addiction (i.e., sexual addiction).[15][17] Moreover, reward cross-sensitization between amphetamine and sexual activity, meaning that exposure to one increases the desire for both, has been shown to occur preclinically and clinically as a dopamine dysregulation syndrome;[15][17][18][19] ΔFosB expression is required for this cross-sensitization effect, which intensifies with the level of ΔFosB expression.[15][18][19]
Food Addiction
Reviews of preclinical studies indicate that long-term frequent and excessive consumption of high fat or sugar foods can produce an addiction (food addiction).[15][16] This can include chocolate. Chocolates' sweet flavour and pharmacological ingredients is known to create a strong craving or feel 'addictive' by the consumer.[22] A person who has a strong liking for chocolate may refer to themselves as a chocoholic. Chocolate is not yet formally recognised by the DSM-5 as a diagnosable addiction.[23]
Gambling provides a natural reward which is associated with compulsive behavior and for which clinical diagnostic manuals, namely the DSM-5, have identified diagnostic criteria for an "addiction".[15] In order for a person's gambling behavior to meet criteria of an addiction, it shows certain characteristics, such as mood modification, compulsivity, and withdrawal. There is evidence from functional neuroimaging that gambling activates the reward system and the mesolimbic pathway in particular.[15][24] Similarly, shopping and playing video games are associated with compulsive behaviors in humans and have also been shown to activate the mesolimbic pathway and other parts of the reward system.[15] Based upon this evidence, gambling addiction, video game addiction, and shopping addiction are classified accordingly.[15][24]
Causes
Personality theories
Personality theories of addiction are psychological models that associate personality traits or modes of thinking (i.e., affective states) with an individual's proclivity for developing an addiction. Data analysis demonstrates that there is a significant difference in the psychological profiles of drug users and non-users and the psychological predisposition to using different drugs may be different.[25] Models of addiction risk that have been proposed in psychology literature include an affect dysregulation model of positive and negative psychological affects, the reinforcement sensitivity theory model of impulsiveness and behavioral inhibition, and an impulsivity model of reward sensitization and impulsiveness.[26][27][28][29][30]
Neuropsychology
Cognitive control and stimulus control, which is associated with operant and classical conditioning, represent opposite processes (i.e., internal vs external or environmental, respectively) that compete over the control of an individual's elicited behaviors.[31] Cognitive control, and particularly inhibitory control over behavior, is impaired in both addiction and attention deficit hyperactivity disorder.[32][33] Stimulus-driven behavioral responses (i.e., stimulus control) that are associated with a particular rewarding stimulus tend to dominate one's behavior in an addiction.[33]
Risk factors
There are a number of genetic and environmental risk factors for developing an addiction, that vary across the population.[3][34] Genetic and environmental risk factors each account for roughly half of an individual's risk for developing an addiction;[3] the contribution from epigenetic risk factors to the total risk is unknown.[34] Even in individuals with a relatively low genetic risk, exposure to sufficiently high doses of an addictive drug for a long period of time (e.g., weeks–months) can result in an addiction.[3] Adverse childhood events are associated with negative health outcomes, such as substance use disorder. Studies show that childhood abuse or exposure to violent crime was positively related to developing a mood or anxiety disorder, as well as a substance dependence risk.[35]
Genetic factors
Genetic factors, along with environmental (e.g., psychosocial) factors, have been established as significant contributors to addiction vulnerability.[3][34] Studies done on 350 hospitalized drug-dependent patients showed that over half met the criteria for alcohol abuse, with a role of familial factors being prevalent.[36] Epidemiological studies estimate that genetic factors account for 40–60% of the risk factors for alcoholism.[37] Similar rates of heritability for other types of drug addiction have been indicated by other studies, specifically in genes that encode the Alpha5 Nicotinic Acetylcholine Receptor.[38] Knestler hypothesized in 1964 that a gene or group of genes might contribute to predisposition to addiction in several ways. For example, altered levels of a normal protein due to environmental factors may change the structure or functioning of specific brain neurons during development. These altered brain neurons could affect the susceptibility of an individual to an initial drug use experience. In support of this hypothesis, animal studies have shown that environmental factors such as stress can affect an animal's genetic expression.[38]
In humans, twin studies into addiction have provided some of the highest-quality evidence of this link, with results finding that if one twin is affected by addiction, the other twin is likely to be as well, and often to the same substance.[39] Further evidence of a genetic component is research findings from family studies which suggest that if one family member has a history of addiction, the chances of a relative or close family developing those same habits are much higher than one who has not been introduced to addiction at a young age.[40]
However, the data implicating specific genes in the development of drug addiction is mixed for most genes. Many addiction studies that aim to identify specific genes focus on common variants with an allele frequency of greater than 5% in the general population; however, when associated with disease, these only confer a small amount of additional risk with an odds ratio of 1.1–1.3 percent; this has led to the development the rare variant hypothesis, which states that genes with low frequencies in the population (<1%) confer much greater additional risk in the development of the disease.[41]
Genome-wide association studies (GWAS) are used to examine genetic associations with dependence, addiction, and drug use; however, these studies rarely identify genes from proteins previously described via animal knockout models and candidate gene analysis. Instead, large percentages of genes involved in processes such as cell adhesion are commonly identified. The important effects of endophenotypes are typically not capable of being captured by these methods. Genes identified in GWAS for drug addiction may be involved either in adjusting brain behavior prior to drug experiences, subsequent to them, or both.[42]
Environmental factors
Environmental risk factors for addiction are the experiences of an individual during their lifetime that interact with the individual's genetic composition to increase or decrease his or her vulnerability to addiction.[3] For example, after the nationwide outbreak of COVID-19, more people quit (vs. started) smoking; and smokers, on average, reduced the quantity of cigarettes they consumed.[43] More generally, a number of different environmental factors have been implicated as risk factors for addiction, including various psychosocial stressors. The National Institute on Drug Abuse (NIDA) cites lack of parental supervision, the prevalence of peer substance use, drug availability, and poverty as risk factors for substance use among children and adolescents.[44] The brain disease model of addiction posits that an individual's exposure to an addictive drug is the most significant environmental risk factor for addiction.[45] However, many researchers, including neuroscientists, indicate that the brain disease model presents a misleading, incomplete, and potentially detrimental explanation of addiction.[46]
Adverse childhood experiences (ACEs) are various forms of maltreatment and household dysfunction experienced in childhood. The Adverse Childhood Experiences Study by the Centers for Disease Control and Prevention has shown a strong dose–response relationship between ACEs and numerous health, social, and behavioral problems throughout a person's lifespan, including substance use disorder.[47] Children's neurological development can be permanently disrupted when they are chronically exposed to stressful events such as physical, emotional, or sexual abuse, physical or emotional neglect, witnessing violence in the household, or a parent being incarcerated or having a mental illness. As a result, the child's cognitive functioning or ability to cope with negative or disruptive emotions may be impaired. Over time, the child may adopt substance use as a coping mechanism, particularly during adolescence.[47] A study of 900 court cases involving children who experienced abuse found that a vast amount of them went on to have some form of addiction in their adolescence or adult life.[48] This pathway towards addiction that is opened through stressful experiences during childhood can be avoided by a change in environmental factors throughout an individual's life and opportunities of professional help.[48] If one has friends or peers who engage in drug use favorably, the chances of them developing an addiction increases. Family conflict and home management is also a cause for one to become engaged in alcohol or other drug use.[49]
Age
Adolescence represents a period of unique vulnerability for developing an addiction.[50] In adolescence, the incentive-rewards systems in the brain mature well before the cognitive control center. This consequentially grants the incentive-rewards systems a disproportionate amount of power in the behavioral decision-making process. Therefore, adolescents are increasingly likely to act on their impulses and engage in risky, potentially addicting behavior before considering the consequences.[51] Not only are adolescents more likely to initiate and maintain drug use, but once addicted they are more resistant to treatment and more liable to relapse.[52][53]
Most individuals are exposed to and use addictive drugs for the first time during their teenage years.[54] In the United States, there were just over 2.8 million new users of illicit drugs in 2013 (~7,800 new users per day);[54] among them, 54.1% were under 18 years of age.[54] In 2011, there were approximately 20.6 million people in the United States over the age of 12 with an addiction.[55] Over 90% of those with an addiction began drinking, smoking or using illicit drugs before the age of 18.[55]
Comorbid disorders
Individuals with comorbid (i.e., co-occurring) mental health disorders such as depression, anxiety, attention-deficit/hyperactivity disorder (ADHD) or post-traumatic stress disorder are more likely to develop substance use disorders.[56][57][58] The NIDA cites early aggressive behavior as a risk factor for substance use.[44] A study by the National Bureau of Economic Research found that there is a "definite connection between mental illness and the use of addictive substances" and a majority of mental health patients participate in the use of these substances: 38% alcohol, 44% cocaine, and 40% cigarettes.[59]
Transgenerational epigenetic inheritance
Epigenetic genes and their products (e.g., proteins) are the key components through which environmental influences can affect the genes of an individual;[34] they also serve as the mechanism responsible for transgenerational epigenetic inheritance, a phenomenon in which environmental influences on the genes of a parent can affect the associated traits and behavioral phenotypes of their offspring (e.g., behavioral responses to environmental stimuli).[34] In addiction, epigenetic mechanisms play a central role in the pathophysiology of the disease;[3] it has been noted that some of the alterations to the epigenome which arise through chronic exposure to addictive stimuli during an addiction can be transmitted across generations, in turn affecting the behavior of one's children (e.g., the child's behavioral responses to addictive drugs and natural rewards).[34][60]
The general classes of epigenetic alterations that have been implicated in transgenerational epigenetic inheritance include DNA methylation, histone modifications, and downregulation or upregulation of microRNAs.[34] With respect to addiction, more research is needed to determine the specific heritable epigenetic alterations that arise from various forms of addiction in humans and the corresponding behavioral phenotypes from these epigenetic alterations that occur in human offspring.[34][60] Based upon preclinical evidence from animal research, certain addiction-induced epigenetic alterations in rats can be transmitted from parent to offspring and produce behavioral phenotypes that decrease the offspring's risk of developing an addiction.[note 1][34] More generally, the heritable behavioral phenotypes that are derived from addiction-induced epigenetic alterations and transmitted from parent to offspring may serve to either increase or decrease the offspring's risk of developing an addiction.[34][60]
Mechanisms
Addiction is a disorder of the brain's reward system developing through transcriptional and epigenetic mechanisms as a result of chronically high levels of exposure to an addictive stimulus (e.g., eating food, the use of cocaine, engagement in sexual activity, participation in high-thrill cultural activities such as gambling, etc.) over extended time.[3][61][15] DeltaFosB (ΔFosB), a gene transcription factor, is a critical component and common factor in the development of virtually all forms of behavioral and drug addictions.[61][15][62][16] Two decades of research into ΔFosB's role in addiction have demonstrated that addiction arises, and the associated compulsive behavior intensifies or attenuates, along with the overexpression of ΔFosB in the D1-type medium spiny neurons of the nucleus accumbens.[3][61][15][62] Due to the causal relationship between ΔFosB expression and addictions, it is used preclinically as an addiction biomarker.[3][61][62] ΔFosB expression in these neurons directly and positively regulates drug self-administration and reward sensitization through positive reinforcement, while decreasing sensitivity to aversion.[note 2][3][61]
| Transcription factor glossary | |
|---|---|
| |
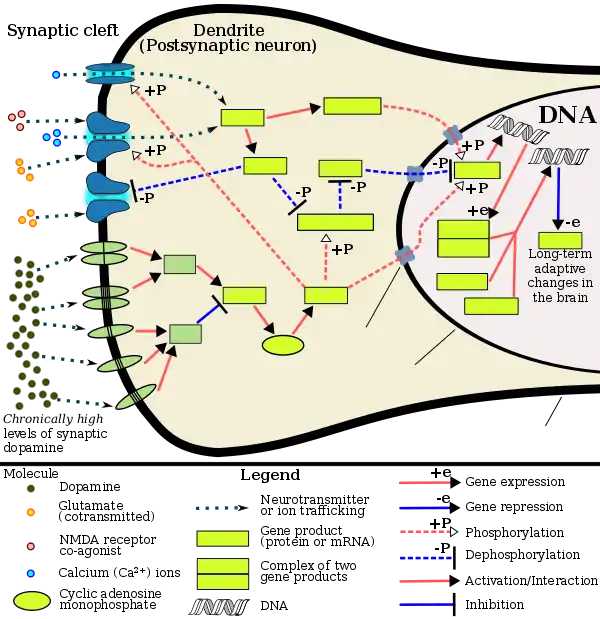
Signaling cascade in the nucleus accumbens that results in psychostimulant addiction
|
Chronic addictive drug use causes alterations in gene expression in the mesocorticolimbic projection.[16][70][71] The most important transcription factors that produce these alterations are ΔFosB, cAMP response element binding protein (CREB), and nuclear factor kappa B (NF-κB).[16] ΔFosB is the most significant biomolecular mechanism in addiction because the overexpression of ΔFosB in the D1-type medium spiny neurons in the nucleus accumbens is necessary and sufficient for many of the neural adaptations and behavioral effects (e.g., expression-dependent increases in drug self-administration and reward sensitization) seen in drug addiction.[16] ΔFosB expression in nucleus accumbens D1-type medium spiny neurons directly and positively regulates drug self-administration and reward sensitization through positive reinforcement while decreasing sensitivity to aversion.[note 2][3][61] ΔFosB has been implicated in mediating addictions to many different drugs and drug classes, including alcohol, amphetamine and other substituted amphetamines, cannabinoids, cocaine, methylphenidate, nicotine, opiates, phenylcyclidine, and propofol, among others.[61][16][70][72][73] ΔJunD, a transcription factor, and G9a, a histone methyltransferase, both oppose the function of ΔFosB and inhibit increases in its expression.[3][16][74] Increases in nucleus accumbens ΔJunD expression (via viral vector-mediated gene transfer) or G9a expression (via pharmacological means) reduces, or with a large increase can even block, many of the neural and behavioral alterations that result from chronic high-dose use of addictive drugs (i.e., the alterations mediated by ΔFosB).[62][16]
ΔFosB also plays an important role in regulating behavioral responses to natural rewards, such as palatable food, sex, and exercise.[16][75] Natural rewards, like drugs of abuse, induce gene expression of ΔFosB in the nucleus accumbens, and chronic acquisition of these rewards can result in a similar pathological addictive state through ΔFosB overexpression.[15][16][75] Consequently, ΔFosB is the key transcription factor involved in addictions to natural rewards (i.e., behavioral addictions) as well;[16][15][75] in particular, ΔFosB in the nucleus accumbens is critical for the reinforcing effects of sexual reward.[75] Research on the interaction between natural and drug rewards suggests that dopaminergic psychostimulants (e.g., amphetamine) and sexual behavior act on similar biomolecular mechanisms to induce ΔFosB in the nucleus accumbens and possess bidirectional cross-sensitization effects that are mediated through ΔFosB.[15][18][19] This phenomenon is notable since, in humans, a dopamine dysregulation syndrome, characterized by drug-induced compulsive engagement in natural rewards (specifically, sexual activity, shopping, and gambling), has also been observed in some individuals taking dopaminergic medications.[15]
ΔFosB inhibitors (drugs or treatments that oppose its action) may be an effective treatment for addiction and addictive disorders.[76]
The release of dopamine in the nucleus accumbens plays a role in the reinforcing qualities of many forms of stimuli, including naturally reinforcing stimuli like palatable food and sex.[77][78] Altered dopamine neurotransmission is frequently observed following the development of an addictive state.[15] In humans and lab animals that have developed an addiction, alterations in dopamine or opioid neurotransmission in the nucleus accumbens and other parts of the striatum are evident.[15] Studies have found that use of certain drugs (e.g., cocaine) affect cholinergic neurons that innervate the reward system, in turn affecting dopamine signaling in this region.[79]
Mesocorticolimbic pathway
ΔFosB accumulation from excessive drug use
Top: this depicts the initial effects of high dose exposure to an addictive drug on gene expression in the nucleus accumbens for various Fos family proteins (i.e., c-Fos, FosB, ΔFosB, Fra1, and Fra2).
Bottom: this illustrates the progressive increase in ΔFosB expression in the nucleus accumbens following repeated twice daily drug binges, where these phosphorylated (35–37 kilodalton) ΔFosB isoforms persist in the D1-type medium spiny neurons of the nucleus accumbens for up to 2 months.[68][80] |
Understanding the pathways in which drugs act and how drugs can alter those pathways is key when examining the biological basis of drug addiction. The reward pathway, known as the mesolimbic pathway, or its extension, the mesocorticolimbic pathway, is characterized by the interaction of several areas of the brain.
- The projections from the ventral tegmental area (VTA) are a network of dopaminergic neurons with co-localized postsynaptic glutamate receptors (AMPAR and NMDAR). These cells respond when stimuli indicative of a reward are present. The VTA supports learning and sensitization development and releases DA into the forebrain.[81] These neurons also project and release DA into the nucleus accumbens,[82] through the mesolimbic pathway. Virtually all drugs causing drug addiction increase the dopamine release in the mesolimbic pathway,[83] in addition to their specific effects.
- The nucleus accumbens (NAcc) is one output of the VTA projections. The nucleus accumbens itself consists mainly of GABAergic medium spiny neurons (MSNs).[84] The NAcc is associated with acquiring and eliciting conditioned behaviors, and is involved in the increased sensitivity to drugs as addiction progresses.[81] Overexpression of ΔFosB in the nucleus accumbens is a necessary common factor in essentially all known forms of addiction;[3] ΔFosB is a strong positive modulator of positively reinforced behaviors.[3]
- The prefrontal cortex, including the anterior cingulate and orbitofrontal cortices,[85] is another VTA output in the mesocorticolimbic pathway; it is important for the integration of information which helps determine whether a behavior will be elicited.[86] It is also critical for forming associations between the rewarding experience of drug use and cues in the environment. Importantly, these cues are strong mediators of drug-seeking behavior and can trigger relapse even after months or years of abstinence.[87]
Other brain structures that are involved in addiction include:
- The basolateral amygdala projects into the NAcc and is thought to also be important for motivation.[86]
- The hippocampus is involved in drug addiction, because of its role in learning and memory. Much of this evidence stems from investigations showing that manipulating cells in the hippocampus alters dopamine levels in NAcc and firing rates of VTA dopaminergic cells.[82]
Role of dopamine and glutamate
Dopamine is the primary neurotransmitter of the reward system in the brain. It plays a role in regulating movement, emotion, cognition, motivation, and feelings of pleasure.[88] Natural rewards, like eating, as well as recreational drug use cause a release of dopamine, and are associated with the reinforcing nature of these stimuli.[88][89] Nearly all addictive drugs, directly or indirectly, act upon the brain's reward system by heightening dopaminergic activity.[90]
Excessive intake of many types of addictive drugs results in repeated release of high amounts of dopamine, which in turn affects the reward pathway directly through heightened dopamine receptor activation. Prolonged and abnormally high levels of dopamine in the synaptic cleft can induce receptor downregulation in the neural pathway. Downregulation of mesolimbic dopamine receptors can result in a decrease in the sensitivity to natural reinforcers.[88]
Drug seeking behavior is induced by glutamatergic projections from the prefrontal cortex to the nucleus accumbens. This idea is supported with data from experiments showing that drug seeking behavior can be prevented following the inhibition of AMPA glutamate receptors and glutamate release in the nucleus accumbens.[85]
Reward sensitization
| Target gene |
Target expression |
Neural effects | Behavioral effects |
|---|---|---|---|
| c-Fos | ↓ | Molecular switch enabling the chronic induction of ΔFosB[note 3] | – |
| dynorphin | ↓ [note 4] | • Downregulation of κ-opioid feedback loop | • Increased drug reward |
| NF-κB | ↑ | • Expansion of NAcc dendritic processes • NF-κB inflammatory response in the NAcc • NF-κB inflammatory response in the CP | • Increased drug reward • Increased drug reward • Locomotor sensitization |
| GluR2 | ↑ | • Decreased sensitivity to glutamate | • Increased drug reward |
| Cdk5 | ↑ | • GluR1 synaptic protein phosphorylation • Expansion of NAcc dendritic processes | Decreased drug reward (net effect) |
Reward sensitization is a process that causes an increase in the amount of reward (specifically, incentive salience[note 5]) that is assigned by the brain to a rewarding stimulus (e.g., a drug). In simple terms, when reward sensitization to a specific stimulus (e.g., a drug) occurs, an individual's "wanting" or desire for the stimulus itself and its associated cues increases.[93][92][94] Reward sensitization normally occurs following chronically high levels of exposure to the stimulus. ΔFosB (DeltaFosB) expression in D1-type medium spiny neurons in the nucleus accumbens has been shown to directly and positively regulate reward sensitization involving drugs and natural rewards.[3][61][62]
"Cue-induced wanting" or "cue-triggered wanting", a form of craving that occurs in addiction, is responsible for most of the compulsive behavior that people with addictions exhibit.[92][94] During the development of an addiction, the repeated association of otherwise neutral and even non-rewarding stimuli with drug consumption triggers an associative learning process that causes these previously neutral stimuli to act as conditioned positive reinforcers of addictive drug use (i.e., these stimuli start to function as drug cues).[92][95][94] As conditioned positive reinforcers of drug use, these previously neutral stimuli are assigned incentive salience (which manifests as a craving) – sometimes at pathologically high levels due to reward sensitization – which can transfer to the primary reinforcer (e.g., the use of an addictive drug) with which it was originally paired.[92][95][94]
Research on the interaction between natural and drug rewards suggests that dopaminergic psychostimulants (e.g., amphetamine) and sexual behavior act on similar biomolecular mechanisms to induce ΔFosB in the nucleus accumbens and possess a bidirectional reward cross-sensitization effect[note 6] that is mediated through ΔFosB.[15][18][19] In contrast to ΔFosB's reward-sensitizing effect, CREB transcriptional activity decreases user's sensitivity to the rewarding effects of the substance. CREB transcription in the nucleus accumbens is implicated in psychological dependence and symptoms involving a lack of pleasure or motivation during drug withdrawal.[3][80][91]
| Form of neuroplasticity or behavioral plasticity |
Type of reinforcer | Sources | |||||
|---|---|---|---|---|---|---|---|
| Opiates | Psychostimulants | High fat or sugar food | Sexual intercourse | Physical exercise (aerobic) |
Environmental enrichment | ||
| ΔFosB expression in nucleus accumbens D1-type MSNs |
↑ | ↑ | ↑ | ↑ | ↑ | ↑ | [15] |
| Behavioral plasticity | |||||||
| Escalation of intake | Yes | Yes | Yes | [15] | |||
| Psychostimulant cross-sensitization |
Yes | Not applicable | Yes | Yes | Attenuated | Attenuated | [15] |
| Psychostimulant self-administration |
↑ | ↑ | ↓ | ↓ | ↓ | [15] | |
| Psychostimulant conditioned place preference |
↑ | ↑ | ↓ | ↑ | ↓ | ↑ | [15] |
| Reinstatement of drug-seeking behavior | ↑ | ↑ | ↓ | ↓ | [15] | ||
| Neurochemical plasticity | |||||||
| CREB phosphorylation in the nucleus accumbens |
↓ | ↓ | ↓ | ↓ | ↓ | [15] | |
| Sensitized dopamine response in the nucleus accumbens |
No | Yes | No | Yes | [15] | ||
| Altered striatal dopamine signaling | ↓DRD2, ↑DRD3 | ↑DRD1, ↓DRD2, ↑DRD3 | ↑DRD1, ↓DRD2, ↑DRD3 | ↑DRD2 | ↑DRD2 | [15] | |
| Altered striatal opioid signaling | No change or ↑μ-opioid receptors | ↑μ-opioid receptors ↑κ-opioid receptors | ↑μ-opioid receptors | ↑μ-opioid receptors | No change | No change | [15] |
| Changes in striatal opioid peptides | ↑dynorphin No change: enkephalin | ↑dynorphin | ↓enkephalin | ↑dynorphin | ↑dynorphin | [15] | |
| Mesocorticolimbic synaptic plasticity | |||||||
| Number of dendrites in the nucleus accumbens | ↓ | ↑ | ↑ | [15] | |||
| Dendritic spine density in the nucleus accumbens |
↓ | ↑ | ↑ | [15] | |||
Neuroepigenetic mechanisms
Altered epigenetic regulation of gene expression within the brain's reward system plays a significant and complex role in the development of drug addiction.[74][96] Addictive drugs are associated with three types of epigenetic modifications within neurons.[74] These are (1) histone modifications, (2) epigenetic methylation of DNA at CpG sites at (or adjacent to) particular genes, and (3) epigenetic downregulation or upregulation of microRNAs which have particular target genes.[74][16][96] As an example, while hundreds of genes in the cells of the nucleus accumbens (NAc) exhibit histone modifications following drug exposure – particularly, altered acetylation and methylation states of histone residues[96] – most other genes in the NAc cells do not show such changes.[74]
Diagnosis
DSM-5
The 5th edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) uses the term "substance use disorder" to refer to a spectrum of drug use-related disorders. The DSM-5 eliminates the terms "abuse" and "dependence" from diagnostic categories, instead using the specifiers of mild, moderate and severe to indicate the extent of disordered use. These specifiers are determined by the number of diagnostic criteria present in a given case. In the DSM-5, the term drug addiction is synonymous with severe substance use disorder.[1][2]
The DSM-5 introduced a new diagnostic category for behavioral addictions; however, problem gambling is the only condition included in that category in the 5th edition.[13] Internet gaming disorder is listed as a "condition requiring further study" in the DSM-5.[97]
Past editions have used physical dependence and the associated withdrawal syndrome to identify an addictive state. Physical dependence occurs when the body has adjusted by incorporating the substance into its "normal" functioning – i.e., attains homeostasis – and therefore physical withdrawal symptoms occur upon cessation of use.[98] Tolerance is the process by which the body continually adapts to the substance and requires increasingly larger amounts to achieve the original effects. Withdrawal refers to physical and psychological symptoms experienced when reducing or discontinuing a substance that the body has become dependent on. Symptoms of withdrawal generally include but are not limited to body aches, anxiety, irritability, intense cravings for the substance, nausea, hallucinations, headaches, cold sweats, tremors, and seizures.
Medical researchers who actively study addiction have criticized the DSM classification of addiction for being flawed and involving arbitrary diagnostic criteria.[14]
ICD-11
The eleventh revision of the International Classification of Diseases, commonly referred to as ICD-11, conceptualizes diagnosis somewhat differently. ICD-11 first distinguishes between problems with psychoactive substance use ("Disorders due to substance use") and behavioral addictions ("Disorders due to addictive behaviours").[99] With regard to psychoactive substances, ICD-11 explains that the included substances initially produce "pleasant or appealing psychoactive effects that are rewarding and reinforcing with repeated use, [but] with continued use, many of the included substances have the capacity to produce dependence. They also have the potential to cause numerous forms of harm, both to mental and physical health."[100] Instead of the DSM-5 approach of one diagnosis ("Substance Use Disorder") covering all types of problematic substance use, ICD-11 offers three diagnostic possibilities: 1) Episode of Harmful Psychoactive Substance Use, 2) Harmful Pattern of Psychoactive Substance Use, and 3) Substance Dependence.[100]
Prevention
Abuse liability
Abuse liability, which is also known as addiction liability, is the tendency to use drugs in a non-medical situation. This is typically for euphoria, mood changing, or sedation.[101] Abuse liability is used when the person using the drugs wants something that they otherwise can not obtain. The only way to obtain this is through the use of drugs. When looking at abuse liability there are a number of determining factors in whether the drug is abused. These factors are: the chemical makeup of the drug, the effects on the brain, and the age, vulnerability, and the health (mental and physical) of the population being studied.[101] There are a few drugs with a specific chemical makeup that leads to a high abuse liability. These are: cocaine, heroin, inhalants, marijuana, MDMA (ecstasy), methamphetamine, PCP, synthetic cannabinoids, synthetic cathinones (bath salts), nicotine (e.g. tobacco), and alcohol.[102]
Treatment and management
According to a review, "in order to be effective, all pharmacological or biologically based treatments for addiction need to be integrated into other established forms of addiction rehabilitation, such as cognitive behavioral therapy, individual and group psychotherapy, behavior modification strategies, twelve-step programs, and residential treatment facilities."[103]
A biosocial approach to the treatment of addiction brings to the fore the social determinants of illness and wellbeing and considers the dynamic and reciprocal relationships that exist for, and influence, the individual's experience.[104]
The work of A.V. Schlosser (2018) aims to pronounce the individual lived experiences of women receiving medication-assisted treatment (e.g., methadone, naltrexone, burprenorphine) in a long-term rehabilitation setting, through a twenty month long ethnographic fieldwork investigation. This person-centred research shows how the experiences of these women "emerge from stable systems of inequality based in intersectional gender, race, and class marginalization entangled with processes of intra-action."[105]
Viewing addiction treatment through this lens also highlights the importance of framing clients' own bodies as "social flesh." As Schlosser (2018) points out, "client bodies" as well as the "embodied experiences of self and social belonging emerge in and through the structures, temporalities, and expectations of the treatment centre."[105]
Further challenges and embodied tensions have the potential to arise as a result of the dynamics inherent in the patient-provider relationship, in addition to the experience of being "alienated from their own bodies, psyches and sociality's when sedated on medications in treatment."[105]
Biotechnologies currently make up a large portion of the future treatments for addiction. To name a few, deep-brain stimulation, agonist/antagonist implants and hapten conjugate vaccines. Vaccinations against addiction specifically overlaps with the belief that memory plays a large role in the damaging effects of addiction and relapses. Hapten conjugate vaccines are designed to block opioid receptors in one area, while allowing other receptors to behave normally. Essentially, once a high can no longer be achieved in relation to a traumatic event, the relation of drugs to a traumatic memory can be disconnected and therapy can then play a role in treatment.[106]
Behavioral therapy
A meta-analytic review on the efficacy of various behavioral therapies for treating drug and behavioral addictions found that cognitive behavioral therapy (e.g., relapse prevention and contingency management), motivational interviewing, and a community reinforcement approach were effective interventions with moderate effect sizes.[107]
Clinical and preclinical evidence indicate that consistent aerobic exercise, especially endurance exercise (e.g., marathon running), actually prevents the development of certain drug addictions and is an effective adjunct treatment for drug addiction, and for psychostimulant addiction in particular.[15][108][109][110][111] Consistent aerobic exercise magnitude-dependently (i.e., by duration and intensity) reduces drug addiction risk, which appears to occur through the reversal of drug induced addiction-related neuroplasticity.[15][109] One review noted that exercise may prevent the development of drug addiction by altering ΔFosB or c-Fos immunoreactivity in the striatum or other parts of the reward system.[111] Aerobic exercise decreases drug self-administration, reduces the likelihood of relapse, and induces opposite effects on striatal dopamine receptor D2 (DRD2) signaling (increased DRD2 density) to those induced by addictions to several drug classes (decreased DRD2 density).[15][109] Consequently, consistent aerobic exercise may lead to better treatment outcomes when used as an adjunct treatment for drug addiction.[15][109][110]
Alcohol addiction
Alcohol, like opioids, can induce a severe state of physical dependence and produce withdrawal symptoms such as delirium tremens. Because of this, treatment for alcohol addiction usually involves a combined approach dealing with dependence and addiction simultaneously. Benzodiazepines have the largest and the best evidence base in the treatment of alcohol withdrawal and are considered the gold standard of alcohol detoxification.[112]
Pharmacological treatments for alcohol addiction include drugs like naltrexone (opioid antagonist), disulfiram, acamprosate, and topiramate.[113][114] Rather than substituting for alcohol, these drugs are intended to affect the desire to drink, either by directly reducing cravings as with acamprosate and topiramate, or by producing unpleasant effects when alcohol is consumed, as with disulfiram. These drugs can be effective if treatment is maintained, but compliance can be an issue as alcoholic patients often forget to take their medication, or discontinue use because of excessive side effects.[115][116] According to a Cochrane Collaboration review, the opioid antagonist naltrexone has been shown to be an effective treatment for alcoholism, with the effects lasting three to twelve months after the end of treatment.[117]
Behavioral addictions
Behavioral addiction is a treatable condition. Treatment options include psychotherapy and psychopharmacotherapy (i.e., medications) or a combination of both. Cognitive behavioral therapy (CBT) is the most common form of psychotherapy used in treating behavioral addictions; it focuses on identifying patterns that trigger compulsive behavior and making lifestyle changes to promote healthier behaviors. Because cognitive behavioral therapy is considered a short term therapy, the number of sessions for treatment normally ranges from five to twenty. During the session, therapists will lead patients through the topics of identifying the issue, becoming aware of one's thoughts surrounding the issue, identifying any negative or false thinking, and reshaping said negative and false thinking. While CBT does not cure behavioral addiction, it does help with coping with the condition in a healthy way. Currently, there are no medications approved for treatment of behavioral addictions in general, but some medications used for treatment of drug addiction may also be beneficial with specific behavioral addictions.[24] Any unrelated psychiatric disorders should be kept under control, and differentiated from the contributing factors that cause the addiction.
Cannabinoid addiction
A 2013 review on cannabinoid addiction noted that the development of CB1 receptor agonists that have reduced interaction with β-arrestin 2 signalling might be therapeutically useful.[118]As of 2019, there has been some evidence of effective pharmacological interventions for cannabinoid addiction, however, none have been approved yet.[119]
Nicotine addiction
Another area in which drug treatment has been widely used is in the treatment of nicotine addiction, which usually involves the use of nicotine replacement therapy, nicotinic receptor antagonists, or nicotinic receptor partial agonists.[120][121] Examples of drugs that act on nicotinic receptors and have been used for treating nicotine addiction include antagonists like bupropion and the partial agonist varenicline.[120][121] A 2019 review looking at the partial agonist cytisine, names it an effective, and affordable cessation treatment for smokers.[122] When access to varenicline and nicotine replacement therapy is limited (due to availability or cost), cytisine is considered the first line of treatment for smoking cessation.[122]
Opioid addiction
Opioids cause physical dependence, and treatment typically addresses both dependence and addiction.
Physical dependence is treated using replacement drugs such as suboxone or subutex (both containing the active ingredients buprenorphine) and methadone.[123][124] Although these drugs perpetuate physical dependence, the goal of opiate maintenance is to provide a measure of control over both pain and cravings. Use of replacement drugs increases the addicted individual's ability to function normally and eliminates the negative consequences of obtaining controlled substances illicitly. Once a prescribed dosage is stabilized, treatment enters maintenance or tapering phases. In the United States, opiate replacement therapy is tightly regulated in methadone clinics and under the DATA 2000 legislation. In some countries, other opioid derivatives such as dihydrocodeine,[125] dihydroetorphine[126] and even heroin[127][128] are used as substitute drugs for illegal street opiates, with different prescriptions being given depending on the needs of the individual patient. Baclofen has led to successful reductions of cravings for stimulants, alcohol, and opioids, and also alleviates alcohol withdrawal syndrome. Many patients have stated they "became indifferent to alcohol" or "indifferent to cocaine" overnight after starting baclofen therapy.[129] Some studies show the interconnection between opioid drug detoxification and overdose mortality.[130]
Psychostimulant addiction
As of May 2014, there is no effective pharmacotherapy for any form of psychostimulant addiction.[103][131][132][133] Reviews from 2015, 2016, and 2018 indicated that TAAR1-selective agonists have significant therapeutic potential as a treatment for psychostimulant addictions;[134][135][136] however, as of 2018, the only compounds which are known to function as TAAR1-selective agonists are experimental drugs.[134][135][136]
Research
Research indicates that vaccines which utilize anti-drug monoclonal antibodies can mitigate drug-induced positive reinforcement by preventing the drug from moving across the blood–brain barrier;[137] however, current vaccine-based therapies are only effective in a relatively small subset of individuals.[137][138] As of November 2015, vaccine-based therapies are being tested in human clinical trials as a treatment for addiction and preventive measure against drug overdoses involving nicotine, cocaine, and methamphetamine.[137]
The new study shows, that the vaccine may also save lives during a drug overdose. In this instance, the idea is that the body will respond to the vaccine by quickly producing antibodies to prevent the opioids from accessing the brain.[139]
Since addiction involves abnormalities in glutamate and GABAergic neurotransmission,[140][141] receptors associated with these neurotransmitters (e.g., AMPA receptors, NMDA receptors, and GABAB receptors) are potential therapeutic targets for addictions.[140][141][142][143] N-acetylcysteine, which affects metabotropic glutamate receptors and NMDA receptors, has shown some benefit in preclinical and clinical studies involving addictions to cocaine, heroin, and cannabinoids.[140] It may also be useful as an adjunct therapy for addictions to amphetamine-type stimulants, but more clinical research is required.[140]
Current medical reviews of research involving lab animals have identified a drug class – class I histone deacetylase inhibitors[note 7] – that indirectly inhibits the function and further increases in the expression of accumbal ΔFosB by inducing G9a expression in the nucleus accumbens after prolonged use.[62][74][144][96] These reviews and subsequent preliminary evidence which used oral administration or intraperitoneal administration of the sodium salt of butyric acid or other class I HDAC inhibitors for an extended period indicate that these drugs have efficacy in reducing addictive behavior in lab animals[note 8] that have developed addictions to ethanol, psychostimulants (i.e., amphetamine and cocaine), nicotine, and opiates;[74][96][145][146] however, few clinical trials involving humans with addictions and any HDAC class I inhibitors have been conducted to test for treatment efficacy in humans or identify an optimal dosing regimen.[note 9]
Gene therapy for addiction is an active area of research. One line of gene therapy research involves the use of viral vectors to increase the expression of dopamine D2 receptor proteins in the brain.[148][149][150][151][152]
Epidemiology
Due to cultural variations, the proportion of individuals who develop a drug or behavioral addiction within a specified time period (i.e., the prevalence) varies over time, by country, and across national population demographics (e.g., by age group, socioeconomic status, etc.).[34]
Asia
The prevalence of alcohol dependence is not as high as is seen in other regions. In Asia, not only socioeconomic factors but also biological factors influence drinking behavior.[153]
The overall prevalence of smartphone ownership is 62%, ranging from 41% in China to 84% in South Korea. Moreover, participation in online gaming ranges from 11% in China to 39% in Japan. Hong Kong has the highest number of adolescents reporting daily or above Internet use (68%). Internet addiction disorder is highest in the Philippines, according to both the IAT (Internet Addiction Test) – 5% and the CIAS-R (Revised Chen Internet Addiction Scale) – 21%.[154]
Australia
The prevalence of substance use disorder among Australians was reported at 5.1% in 2009.[155]
Europe
In 2015, the estimated prevalence among the adult population was 18.4% for heavy episodic alcohol use (in the past 30 days); 15.2% for daily tobacco smoking; and 3.8, 0.77, 0.37 and 0.35% in 2017 cannabis, amphetamine, opioid and cocaine use. The mortality rates for alcohol and illicit drugs were highest in Eastern Europe.[156]
United States
Based upon representative samples of the US youth population in 2011, the lifetime prevalence[note 10] of addictions to alcohol and illicit drugs has been estimated to be approximately 8% and 2–3% respectively.[157] Based upon representative samples of the US adult population in 2011, the 12 month prevalence of alcohol and illicit drug addictions were estimated at 12% and 2–3% respectively.[157] The lifetime prevalence of prescription drug addictions is currently around 4.7%.[158]
As of 2016, about 22 million people in the United States need treatment for an addiction to alcohol, nicotine, or other drugs.[159][160] Only about 10%, or a little over 2 million, receive any form of treatments, and those that do generally do not receive evidence-based care.[159][160] One-third of inpatient hospital costs and 20% of all deaths in the US every year are the result of untreated addictions and risky substance use.[159][160] In spite of the massive overall economic cost to society, which is greater than the cost of diabetes and all forms of cancer combined, most doctors in the US lack the training to effectively address a drug addiction.[159][160]
Another review listed estimates of lifetime prevalence rates for several behavioral addictions in the United States, including 1–2% for compulsive gambling, 5% for sexual addiction, 2.8% for food addiction, and 5–6% for compulsive shopping.[15] A systematic review indicated that the time-invariant prevalence rate for sexual addiction and related compulsive sexual behavior (e.g., compulsive masturbation with or without pornography, compulsive cybersex, etc.) within the United States ranges from 3–6% of the population.[17]
According to a 2017 poll conducted by the Pew Research Center, almost half of US adults know a family member or close friend who has struggled with a drug addiction at some point in their life.[161]
In 2019, opioid addiction was acknowledged as a national crisis in the United States.[162] An article in The Washington Post stated that "America's largest drug companies flooded the country with pain pills from 2006 through 2012, even when it became apparent that they were fueling addiction and overdoses."
The National Epidemiologic Survey on Alcohol and Related Conditions found that from 2012 to 2013 the prevalence of Cannabis use disorder in U.S. adults was 2.9%.[163]
South America
The realities of opioid use and opioid use disorder in Latin America may be deceptive if observations are limited to epidemiological findings. In the United Nations Office on Drugs and Crime report,[164] although South America produced 3% of the world's morphine and heroin and 0.01% of its opium, prevalence of use is uneven. According to the Inter-American Commission on Drug Abuse Control, consumption of heroin is low in most Latin American countries, although Colombia is the area's largest opium producer. Mexico, because of its border with the United States, has the highest incidence of use.[165]
History and etymology
The etymology of the term addiction throughout history has been often misunderstood and has taken on various meanings associated with the word.[166] An example is the usage of the word in the religious landscape of early modern Europe.[167] "Addiction" at the time meant "to attach" to something, giving it both positive and negative connotations. The object of this attachment could be characterised as "good or bad".[168] However, the meaning of addiction during the early modern period was mostly associated with positivity and goodness;[167] during this early modern and highly religious era of Christian revivalism and Pietistic tendencies,[167] it was seen as a way of "devoting oneself to another".[168]
Modern research on addiction has led to a better understanding of the disease with research studies on the topic dating back to 1875, specifically on morphine addiction.[169] This furthered the understanding of addiction being a medical condition. It wasn't until the 19th century that addiction was seen and acknowledged in the Western world as a disease, being both a physical condition and mental illness.[170] Today, addiction is understood both as a biopsychosocial and neurological disorder that negatively impacts those who are affected by it, most commonly associated with the use of drugs and excessive use of alcohol.[7] The understanding of addiction has changed throughout history, which has impacted and continues to impact the ways it is medically treated and diagnosed.
Society and culture
.jpg.webp)
A biopsychosocial–spiritual understanding of addiction
While regarded biomedically as a neuropsychological disorder, addiction is multi-layered, with biological, psychological, social, cultural and spiritual (biopsychosocial–spiritual) elements.[171][172] A biopsychosocial–spiritual approach fosters the crossing of disciplinary boundaries, and promotes holistic considerations of addiction.[173][174][175] A biopsychosocial–spiritual approach considers, for example, how physical environments influence experiences, habits, and patterns of addiction.
Ethnographic engagements and developments in fields of knowledge have contributed to biopsychosocial–spiritual understandings of addiction, including the work of Philippe Bourgois, whose fieldwork with street-level drug dealers in East Harlem highlights correlations between drug use and structural oppression in the United States.[176][3] Prior models that have informed the prevailing biopsychosocial–spiritual consideration of addiction include:
The Cultural Model
The cultural model, an anthropological understanding of the emergence of drug use and abuse, was developed by Dwight Heath.[177] Heath undertook ethnographic research and fieldwork with the Camba people of Bolivia from June 1956 to August 1957.[178] Heath observed that adult members of society drank ‘large quantities of rum and became intoxicated for several contiguous days at least twice a month’.[177] This frequent, heavy drinking from which intoxication followed was typically undertaken socially, during festivals.[178] Having returned in 1989, Heath observed that whilst much had changed, ‘drinking parties’ remained, as per his initial observations, and ‘there appear to be no harmful consequences to anyone’.[179] Heath’s observations and interactions reflected that this form of social behaviour, the habitual heavy consumption of alcohol, was encouraged and valued, enforcing social bonds in the Camba community.[178] Despite frequent intoxication, “even to the point of unconsciousness”, the Camba held no concept of alcoholism (a form of addiction), and no visible social problems associated with drunkenness, or addiction, were apparent.[177]
As noted by Merrill Singer, Heath’s findings, when considered alongside subsequent cross-cultural experiences, challenged the perception that intoxication is socially ‘inherently disruptive’.[177] Following this fieldwork, Heath proposed the ‘cultural model’, suggesting that ‘problems’ associated with heavy drinking, such as alcoholism – a recognised form addiction – were cultural: that is, that alcoholism is determined by cultural beliefs, and therefore varies among cultures. Heath’s findings challenged the notion that ‘continued use [of alcohol] is inexorably addictive and damaging to the consumer’s health’.[178][177]
The cultural model did face criticism by Sociologist Robin Room and others, who felt anthropologists could “downgrade the severity of the problem”.[177] Merrill Singer found it notable that the ethnographers working within the prominence of the cultural model were part of the ‘wet generation’: while not blind to the ‘disruptive, dysfunctional and debilitating effects of alcohol consumption’, they were products ‘socialized to view alcohol consumption as normal’.[177]
The Subcultural Model
Historically, addiction has been viewed from the etic perspective, defining users through the pathology of their condition.[180] As reports of drug use rapidly increased, the cultural model found application in anthropological research exploring western drug subculture practices.[177]
The approach evolved from the ethnographic exploration into the lived experiences and subjectivities of 1960s and 1970s drug subcultures.[177] The seminal publication “Taking care of business”, by Edward Preble and John J. Casey, documented the daily lives of New York street-based intravenous heroin users in rich detail, providing unique insight into the dynamic social worlds and activities that surrounded their drug use.[181]
These findings challenge popular narratives of immorality and deviance, conceptualising substance abuse as a social phenomenon. Furthermore, it suggests that the prevailing culture can have a greater influence on drug taking behaviours than the physical and psychological effects of the drug itself.[182] To marginalised individuals, drug subcultures can provide social connection, symbolic meaning, and socially constructed purpose that they may feel is unattainable through conventional means.[182] The subcultural model demonstrates the complexities of addiction, highlighting the need for an integrated approach. It contends that a biosocial approach is required to achieve a holistic understanding of addiction.[177]
The Critical Medical Anthropology Model
Emerging in the early 1980s, the critical medical anthropology model was introduced, and as Merrill Singer offers ‘was applied quickly to the analysis of drug use’.[177] Where the cultural model of the 1950s looked at the social body, the critical medical anthropology model revealed the body politic, considering drug use and addiction within the context of macro level structures including larger political systems, economic inequalities, and the institutional power held over social processes.[177]
Highly relevant to addiction, the three issues emphasized in the model are:
- The social production of suffering
- Self-medication
- The political economy (licit and illicit drugs)[177]
These three key points highlight how drugs may come to be used to self-medicate the psychological trauma of socio-political disparity and injustice, intertwining with licit and illicit drug market politics.[177] Social suffering, “the misery among those on the weaker end of power relations in terms of physical health, mental health and lived experience”, is used by anthropologists to analyse how individuals may have personal problems caused by political and economic power.[177] From the perspective of critical medical anthropology heavy drug use and addiction is a consequence of such larger scale unequal distributions of power.[177]
The three models developed here – the cultural model, the subcultural model, and the Critical Medical Anthropology Model – display how addiction is not an experience to be considered only biomedically. Through consideration of addiction alongside the biological, psychological, social, cultural and spiritual (biopsychosocial–spiritual) elements which influence its experience, a holistic and comprehensive understanding can be built.
Addiction causes an "astoundingly high financial and human toll" on individuals and society as a whole.[183][157][159] In the United States, the total economic cost to society is greater than that of all types of diabetes and all cancers combined.[159] These costs arise from the direct adverse effects of drugs and associated healthcare costs (e.g., emergency medical services and outpatient and inpatient care), long-term complications (e.g., lung cancer from smoking tobacco products, liver cirrhosis and dementia from chronic alcohol consumption, and meth mouth from methamphetamine use), the loss of productivity and associated welfare costs, fatal and non-fatal accidents (e.g., traffic collisions), suicides, homicides, and incarceration, among others.[183][157][159][184] In the United States, a study conducted by the National Institute on Drug Abuse has found that overdose deaths in the United States have almost tripled amongst male and females from 2002 to 2017, with 72,306 overdose deaths reported in 2017 in the U.S.[185] 2020 marked the year with highest number of overdose deaths over a 12-month period, with 81,000 overdose deaths, exceeding the records set in 2017.[186]
The suffixes "-holic" and "-holism"
In contemporary modern English "-holic" is a suffix that can be added to a subject to denote an addiction to it. It was extracted from the word alcoholism (one of the first addictions to be widely identified both medically and socially) (correctly the root "wikt:alcohol" plus the suffix "-ism") by misdividing or rebracketing it into "alco" and "-holism". (Another such misdivision is interpreting "helicopter" as "heli-copter" rather than the etymologically correct "helico-pter", giving rise to such derived words as "heliport" and "jetcopter".[187]) There are correct medico-legal terms for such addictions: dipsomania is the medico-legal term for alcoholism;[188] other examples are in this table:
| Colloquial term | Addiction to | Medico-legal term |
|---|---|---|
| danceaholic | dance | choreomania |
| workaholic | work | ergomania |
| sexaholic | sex | erotomania, satyromania, nymphomania |
| sugarholic | sugar | saccharomania |
| chocoholic | chocolate | |
| rageaholic | rage / anger |
See also
- Autonomic nervous system
- Binge drinking
- Binge eating disorder
- Discrimination against drug addicts
- Dopaminergic pathways
- Pavlovian-instrumental transfer
- Philosophy of medicine
- Substance dependence
Endnotes
- In other words, a person cannot control the neurobiological processes that occur in the body in response to using an addictive drug. A person can make a voluntary choice to, for example, start using a drug or to seek help after becoming addicted, although resisting the urge to use becomes increasingly difficult as addiction worsens. See [6] for detailed discussion.
Notes
- According to a review of experimental animal models that examined the transgenerational epigenetic inheritance of epigenetic marks that occur in addiction, alterations in histone acetylation – specifically, di-acetylation of lysine residues 9 and 14 on histone 3 (i.e., H3K9ac2 and H3K14ac2) in association with BDNF gene promoters – have been shown to occur within the medial prefrontal cortex (mPFC), testes, and sperm of cocaine-addicted male rats.[34] These epigenetic alterations in the rat mPFC result in increased BDNF gene expression within the mPFC, which in turn blunts the rewarding properties of cocaine and reduces cocaine self-administration.[34] The male but not female offspring of these cocaine-exposed rats inherited both epigenetic marks (i.e., di-acetylation of lysine residues 9 and 14 on histone 3) within mPFC neurons, the corresponding increase in BDNF expression within mPFC neurons, and the behavioral phenotype associated with these effects (i.e., a reduction in cocaine reward, resulting in reduced cocaine-seeking by these male offspring).[34] Consequently, the transmission of these two cocaine-induced epigenetic alterations (i.e., H3K9ac2 and H3K14ac2) in rats from male fathers to male offspring served to reduce the offspring's risk of developing an addiction to cocaine.[34] As of 2018, neither the heritability of these epigenetic marks in humans nor the behavioral effects of the marks within human mPFC neurons has been established.[34]
- A decrease in aversion sensitivity, in simpler terms, means that an individual's behavior is less likely to be influenced by undesirable outcomes.
- In other words, c-Fos repression allows ΔFosB to more rapidly accumulate within the D1-type medium spiny neurons of the nucleus accumbens because it is selectively induced in this state.[3] Prior to c-Fos repression, all Fos family proteins (e.g., c-Fos, Fra1, Fra2, FosB, and ΔFosB) are induced together, with ΔFosB expression increasing to a lesser extent.[3]
- According to two medical reviews, ΔFosB has been implicated in causing both increases and decreases in dynorphin expression in different studies;[61][91] this table entry reflects only a decrease.
- Incentive salience, the "motivational salience" for a reward, is a "desire" or "want" attribute, which includes a motivational component, that the brain assigns to a rewarding stimulus.[92][93] As a consequence, incentive salience acts as a motivational "magnet" for a rewarding stimulus that commands attention, induces approach, and causes the rewarding stimulus to be sought out.[92]
- In simplest terms, this means that when either amphetamine or sex is perceived as more alluring or desirable through reward sensitization, this effect occurs with the other as well.
- Inhibitors of class I histone deacetylase (HDAC) enzymes are drugs that inhibit four specific histone-modifying enzymes: HDAC1, HDAC2, HDAC3, and HDAC8. Most of the animal research with HDAC inhibitors has been conducted with four drugs: butyrate salts (mainly sodium butyrate), trichostatin A, valproic acid, and SAHA;[144][96] butyric acid is a naturally occurring short-chain fatty acid in humans, while the latter two compounds are FDA-approved drugs with medical indications unrelated to addiction.
- Specifically, prolonged administration of a class I HDAC inhibitor appears to reduce an animal's motivation to acquire and use an addictive drug without affecting an animals motivation to attain other rewards (i.e., it does not appear to cause motivational anhedonia) and reduce the amount of the drug that is self-administered when it is readily available.[74][96][145]
- Among the few clinical trials that employed a class I HDAC inhibitor, one utilized valproate for methamphetamine addiction.[147]
- The lifetime prevalence of an addiction is the percentage of individuals in a population that developed an addiction at some point in their life.
- Image legend
References
- "Facing Addiction in America: The Surgeon General's Report on Alcohol, Drugs, and Health" (PDF). Office of the Surgeon General. US Department of Health and Human Services. November 2016. pp. 35–37, 45, 63, 155, 317, 338. Retrieved 28 January 2017.
- Volkow ND, Koob GF, McLellan AT (January 2016). "Neurobiologic Advances from the Brain Disease Model of Addiction". New England Journal of Medicine. 374 (4): 363–371. doi:10.1056/NEJMra1511480. PMC 6135257. PMID 26816013.
Substance-use disorder: A diagnostic term in the fifth edition of the Diagnostic and Statistical Manual of Mental Disorders (DSM-5) referring to recurrent use of alcohol or other drugs that causes clinically and functionally significant impairment, such as health problems, disability, and failure to meet major responsibilities at work, school, or home. Depending on the level of severity, this disorder is classified as mild, moderate, or severe.
Addiction: A term used to indicate the most severe, chronic stage of substance-use disorder, in which there is a substantial loss of self-control, as indicated by compulsive drug taking despite the desire to stop taking the drug. In the DSM-5, the term addiction is synonymous with the classification of severe substance-use disorder. - Nestler EJ (December 2013). "Cellular basis of memory for addiction". Dialogues in Clinical Neuroscience. 15 (4): 431–443. PMC 3898681. PMID 24459410.
Despite the importance of numerous psychosocial factors, at its core, drug addiction involves a biological process: the ability of repeated exposure to a drug of abuse to induce changes in a vulnerable brain that drive the compulsive seeking and taking of drugs, and loss of control over drug use, that define a state of addiction. ... A large body of literature has demonstrated that such ΔFosB induction in D1-type [nucleus accumbens] neurons increases an animal's sensitivity to drug as well as natural rewards and promotes drug self-administration, presumably through a process of positive reinforcement ... Another ΔFosB target is cFos: as ΔFosB accumulates with repeated drug exposure it represses c-Fos and contributes to the molecular switch whereby ΔFosB is selectively induced in the chronic drug-treated state.41 ... Moreover, there is increasing evidence that, despite a range of genetic risks for addiction across the population, exposure to sufficiently high doses of a drug for long periods of time can transform someone who has relatively lower genetic loading into an addict.
- Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and Addictive Disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 364–375. ISBN 9780071481274.
- "Glossary of Terms". Mount Sinai School of Medicine. Department of Neuroscience. Retrieved 9 February 2015.
- Heilig M, MacKillop J, Martinez D, Rehm J, Leggio L, Vanderschuren LJ (September 2021). "Addiction as a brain disease revised: why it still matters, and the need for consilience". Neuropsychopharmacology. 46 (10): 1715–1723. doi:10.1038/s41386-020-00950-y. PMC 8357831. PMID 33619327.
pre-existing vulnerabilities and persistent drug use lead to a vicious circle of substantive disruptions in the brain that impair and undermine choice capacities for adaptive behavior, but do not annihilate them.
- "Drugs, Brains, and Behavior: The Science of Addiction – Drug Misuse and Addiction". www.drugabuse.gov. North Bethesda, Maryland: National Institute on Drug Abuse. 13 July 2020. Retrieved 23 December 2021.
- Henden E (2017). "Addiction, Compulsion, and Weakness of the Will: A Dual-Process Perspective.". In Heather N, Gabriel S (eds.). Addiction and Choice: Rethinking the Relationship. Oxford, UK: Oxford University Press. pp. 116–132.
- Angres DH, Bettinardi-Angres K (October 2008). "The disease of addiction: origins, treatment, and recovery". Disease-a-Month. 54 (10): 696–721. doi:10.1016/j.disamonth.2008.07.002. PMID 18790142.
- Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and Addictive Disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 364–65, 375. ISBN 978-0-07-148127-4.
The defining feature of addiction is compulsive, out-of-control drug use, despite negative consequences. ...
compulsive eating, shopping, gambling, and sex – so-called "natural addictions" – Indeed, addiction to both drugs and behavioral rewards may arise from similar dysregulation of the mesolimbic dopamine system. - Marlatt GA, Baer JS, Donovan DM, Kivlahan DR (1988). "Addictive behaviors: etiology and treatment". Annu Rev Psychol. 39: 223–52. doi:10.1146/annurev.ps.39.020188.001255. PMID 3278676.
- ME (12 September 2019). "Gaming Addiction in ICD-11: Issues and Implications". Psychiatric Times. Psychiatric Times Vol 36, Issue 9. 36 (9). Retrieved 3 March 2020.
- American Psychiatric Association (2013). "Substance-Related and Addictive Disorders" (PDF). American Psychiatric Publishing. pp. 1–2. Archived from the original (PDF) on 15 August 2015. Retrieved 10 July 2015.
Additionally, the diagnosis of dependence caused much confusion. Most people link dependence with "addiction" when in fact dependence can be a normal body response to a substance.
- Malenka RC, Nestler EJ, Hyman SE, Holtzman DM (2015). "Chapter 16: Reinforcement and Addictive Disorders". Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (3rd ed.). New York: McGraw-Hill Medical. ISBN 978-0-07-182770-6.
The official diagnosis of drug addiction by the Diagnostic and Statistic Manual of Mental Disorders (2013), which uses the term substance use disorder, is flawed. Criteria used to make the diagnosis of substance use disorders include tolerance and somatic dependence/withdrawal, even though these processes are not integral to addiction as noted. It is ironic and unfortunate that the manual still avoids use of the term addiction as an official diagnosis, even though addiction provides the best description of the clinical syndrome.
- Olsen CM (December 2011). "Natural rewards, neuroplasticity, and non-drug addictions". Neuropharmacology. 61 (7): 1109–22. doi:10.1016/j.neuropharm.2011.03.010. PMC 3139704. PMID 21459101.
Functional neuroimaging studies in humans have shown that gambling (Breiter et al, 2001), shopping (Knutson et al, 2007), orgasm (Komisaruk et al, 2004), playing video games (Koepp et al, 1998; Hoeft et al, 2008) and the sight of appetizing food (Wang et al, 2004a) activate many of the same brain regions (i.e., the mesocorticolimbic system and extended amygdala) as drugs of abuse (Volkow et al, 2004). ... Cross-sensitization is also bidirectional, as a history of amphetamine administration facilitates sexual behavior and enhances the associated increase in NAc DA ... As described for food reward, sexual experience can also lead to activation of plasticity-related signaling cascades. The transcription factor delta FosB is increased in the NAc, PFC, dorsal striatum, and VTA following repeated sexual behavior (Wallace et al., 2008; Pitchers et al., 2010b). This natural increase in delta FosB or viral overexpression of delta FosB within the NAc modulates sexual performance, and NAc blockade of delta FosB attenuates this behavior (Hedges et al, 2009; Pitchers et al., 2010b). Further, viral overexpression of delta FosB enhances the conditioned place preference for an environment paired with sexual experience (Hedges et al., 2009). ... In some people, there is a transition from "normal" to compulsive engagement in natural rewards (such as food or sex), a condition that some have termed behavioral or non-drug addictions (Holden, 2001; Grant et al., 2006a). ... In humans, the role of dopamine signaling in incentive-sensitization processes has recently been highlighted by the observation of a dopamine dysregulation syndrome in some patients taking dopaminergic drugs. This syndrome is characterized by a medication-induced increase in (or compulsive) engagement in non-drug rewards such as gambling, shopping, or sex (Evans et al, 2006; Aiken, 2007; Lader, 2008)."
Table 1: Summary of plasticity observed following exposure to drug or natural reinforcers" - Robison AJ, Nestler EJ (November 2011). "Transcriptional and epigenetic mechanisms of addiction". Nat. Rev. Neurosci. 12 (11): 623–37. doi:10.1038/nrn3111. PMC 3272277. PMID 21989194.
ΔFosB has been linked directly to several addiction-related behaviors ... Importantly, genetic or viral overexpression of ΔJunD, a dominant negative mutant of JunD which antagonizes ΔFosB- and other AP-1-mediated transcriptional activity, in the NAc or OFC blocks these key effects of drug exposure14,22–24. This indicates that ΔFosB is both necessary and sufficient for many of the changes wrought in the brain by chronic drug exposure. ΔFosB is also induced in D1-type NAc MSNs by chronic consumption of several natural rewards, including sucrose, high fat food, sex, wheel running, where it promotes that consumption14,26–30. This implicates ΔFosB in the regulation of natural rewards under normal conditions and perhaps during pathological addictive-like states.
- Karila L, Wéry A, Weinstein A, Cottencin O, Petit A, Reynaud M, Billieux J (2014). "Sexual addiction or hypersexual disorder: different terms for the same problem? A review of the literature". Curr. Pharm. Des. 20 (25): 4012–20. doi:10.2174/13816128113199990619. PMID 24001295.
Sexual addiction, which is also known as hypersexual disorder, has largely been ignored by psychiatrists, even though the condition causes serious psychosocial problems for many people. A lack of empirical evidence on sexual addiction is the result of the disease's complete absence from versions of the Diagnostic and Statistical Manual of Mental Disorders. ... Existing prevalence rates of sexual addiction-related disorders range from 3% to 6%. Sexual addiction/hypersexual disorder is used as an umbrella construct to encompass various types of problematic behaviors, including excessive masturbation, cybersex, pornography use, sexual behavior with consenting adults, telephone sex, strip club visitation, and other behaviors. The adverse consequences of sexual addiction are similar to the consequences of other addictive disorders. Addictive, somatic and psychiatric disorders coexist with sexual addiction. In recent years, research on sexual addiction has proliferated, and screening instruments have increasingly been developed to diagnose or quantify sexual addiction disorders. In our systematic review of the existing measures, 22 questionnaires were identified. As with other behavioral addictions, the appropriate treatment of sexual addiction should combine pharmacological and psychological approaches.
- Pitchers KK, Vialou V, Nestler EJ, Laviolette SR, Lehman MN, Coolen LM (February 2013). "Natural and drug rewards act on common neural plasticity mechanisms with ΔFosB as a key mediator". The Journal of Neuroscience. 33 (8): 3434–42. doi:10.1523/JNEUROSCI.4881-12.2013. PMC 3865508. PMID 23426671.
Drugs of abuse induce neuroplasticity in the natural reward pathway, specifically the nucleus accumbens (NAc), thereby causing development and expression of addictive behavior. ... Together, these findings demonstrate that drugs of abuse and natural reward behaviors act on common molecular and cellular mechanisms of plasticity that control vulnerability to drug addiction, and that this increased vulnerability is mediated by ΔFosB and its downstream transcriptional targets. ... Sexual behavior is highly rewarding (Tenk et al., 2009), and sexual experience causes sensitized drug-related behaviors, including cross-sensitization to amphetamine (Amph)-induced locomotor activity (Bradley and Meisel, 2001; Pitchers et al., 2010a) and enhanced Amph reward (Pitchers et al., 2010a). Moreover, sexual experience induces neural plasticity in the NAc similar to that induced by psychostimulant exposure, including increased dendritic spine density (Meisel and Mullins, 2006; Pitchers et al., 2010a), altered glutamate receptor trafficking, and decreased synaptic strength in prefrontal cortex-responding NAc shell neurons (Pitchers et al., 2012). Finally, periods of abstinence from sexual experience were found to be critical for enhanced Amph reward, NAc spinogenesis (Pitchers et al., 2010a), and glutamate receptor trafficking (Pitchers et al., 2012). These findings suggest that natural and drug reward experiences share common mechanisms of neural plasticity
- Beloate LN, Weems PW, Casey GR, Webb IC, Coolen LM (February 2016). "Nucleus accumbens NMDA receptor activation regulates amphetamine cross-sensitization and deltaFosB expression following sexual experience in male rats". Neuropharmacology. 101: 154–64. doi:10.1016/j.neuropharm.2015.09.023. PMID 26391065. S2CID 25317397.
- Derbyshire, Katherine L.; Grant, Jon E. (2015-06). "Compulsive sexual behavior: A review of the literature". Journal of Behavioral Addictions. 4 (2): 37–43. doi:10.1556/2006.4.2015.003. ISSN 2062-5871. PMC 4500883. PMID 26014671.
{{cite journal}}: Check date values in:|date=(help)CS1 maint: PMC format (link) - Diagnostic and Statistical Manual of Mental Disorders: DSM-5 (5th ed.). American Psychiatric Association. 2013. p. 481. ISBN 9780890425558.
- Nehlig A (2004). Coffee, tea, chocolate, and the brain. Boca Raton: CRC Press. pp. 203–218. ISBN 9780429211928.
- Meule A, Gearhardt AN (September 2014). "Food addiction in the light of DSM-5". Nutrients. 6 (9): 3653–71. doi:10.3390/nu6093653. PMC 4179181. PMID 25230209.
- Grant JE, Potenza MN, Weinstein A, Gorelick DA (September 2010). "Introduction to behavioral addictions". Am. J. Drug Alcohol Abuse. 36 (5): 233–241. doi:10.3109/00952990.2010.491884. PMC 3164585. PMID 20560821.
Naltrexone, a mu-opioid receptor antagonist approved by the US Food and Drug Administration for the treatment of alcoholism and opioid dependence, has shown efficacy in controlled clinical trials for the treatment of pathological gambling and kleptomania (76–79), and promise in uncontrolled studies of compulsive buying (80), compulsive sexual behavior (81), internet addiction (82), and pathologic skin picking (83). ... Topiramate, an anti-convulsant which blocks the AMPA subtype of glutamate receptor (among other actions), has shown promise in open-label studies of pathological gambling, compulsive buying, and compulsive skin picking (85), as well as efficacy in reducing alcohol (86), cigarette (87), and cocaine (88) use. N-acetyl cysteine, an amino acid that restores extracellular glutamate concentration in the nucleus accumbens, reduced gambling urges and behavior in one study of pathological gamblers (89), and reduces cocaine craving (90) and cocaine use (91) in cocaine addicts. These studies suggest that glutamatergic modulation of dopaminergic tone in the nucleus accumbens may be a mechanism common to behavioral addiction and substance use disorders (92).
- Fehrman E, Egan V, Gorban AN, Levesley J, Mirkes EM, Muhammad AK (2019). Personality Traits and Drug Consumption. A Story Told by Data. Springer, Cham. arXiv:2001.06520. doi:10.1007/978-3-030-10442-9. ISBN 978-3-030-10441-2. S2CID 151160405.
- Cheetham A, Allen NB, Yücel M, Lubman DI (August 2010). "The role of affective dysregulation in drug addiction". Clin Psychol Rev. 30 (6): 621–34. doi:10.1016/j.cpr.2010.04.005. PMID 20546986.
- Franken IH, Muris P (2006). "BIS/BAS personality characteristics and college students' substance use". Personality and Individual Differences. 40 (7): 1497–503. doi:10.1016/j.paid.2005.12.005.
- Genovese JE, Wallace D (December 2007). "Reward sensitivity and substance abuse in middle school and high school students". J Genet Psychol. 168 (4): 465–69. doi:10.3200/GNTP.168.4.465-469. PMID 18232522. S2CID 207640075.
- Kimbrel NA, Nelson-Gray RO, Mitchell JT (April 2007). "Reinforcement sensitivity and maternal style as predictors of psychopathology". Personality and Individual Differences. 42 (6): 1139–49. doi:10.1016/j.paid.2006.06.028.
- Dawe S, Loxton NJ (May 2004). "The role of impulsivity in the development of substance use and eating disorders". Neurosci Biobehav Rev. 28 (3): 343–51. doi:10.1016/j.neubiorev.2004.03.007. PMID 15225976. S2CID 24435589.
- Washburn DA (2016). "The Stroop effect at 80: The competition between stimulus control and cognitive control". J Exp Anal Behav. 105 (1): 3–13. doi:10.1002/jeab.194. PMID 26781048.
Today, arguably more than at any time in history, the constructs of attention, executive functioning, and cognitive control seem to be pervasive and preeminent in research and theory. Even within the cognitive framework, however, there has long been an understanding that behavior is multiply determined, and that many responses are relatively automatic, unattended, contention-scheduled, and habitual. Indeed, the cognitive flexibility, response inhibition, and self-regulation that appear to be hallmarks of cognitive control are noteworthy only in contrast to responses that are relatively rigid, associative, and involuntary.
- Diamond A (2013). "Executive functions". Annu Rev Psychol. 64: 135–68. doi:10.1146/annurev-psych-113011-143750. PMC 4084861. PMID 23020641.
Core EFs are inhibition [response inhibition (self-control – resisting temptations and resisting acting impulsively) and interference control (selective attention and cognitive inhibition)], working memory, and cognitive flexibility (including creatively thinking "outside the box," seeing anything from different perspectives, and quickly and flexibly adapting to changed circumstances). ... EFs and prefrontal cortex are the first to suffer, and suffer disproportionately, if something is not right in your life. They suffer first, and most, if you are stressed (Arnsten 1998, Liston et al. 2009, Oaten & Cheng 2005), sad (Hirt et al. 2008, von Hecker & Meiser 2005), lonely (Baumeister et al. 2002, Cacioppo & Patrick 2008, Campbell et al. 2006, Tun et al. 2012), sleep deprived (Barnes et al. 2012, Huang et al. 2007), or not physically fit (Best 2010, Chaddock et al. 2011, Hillman et al. 2008). Any of these can cause you to appear to have a disorder of EFs, such as ADHD, when you do not. You can see the deleterious effects of stress, sadness, loneliness, and lack of physical health or fitness at the physiological and neuroanatomical level in prefrontal cortex and at the behavioral level in worse EFs (poorer reasoning and problem solving, forgetting things, and impaired ability to exercise discipline and self-control). ...
EFs can be improved (Diamond & Lee 2011, Klingberg 2010). ... At any age across the life cycle EFs can be improved, including in the elderly and in infants. There has been much work with excellent results on improving EFs in the elderly by improving physical fitness (Erickson & Kramer 2009, Voss et al. 2011) ... Inhibitory control (one of the core EFs) involves being able to control one's attention, behavior, thoughts, and/or emotions to override a strong internal predisposition or external lure, and instead do what's more appropriate or needed. Without inhibitory control we would be at the mercy of impulses, old habits of thought or action (conditioned responses), and/or stimuli in the environment that pull us this way or that. Thus, inhibitory control makes it possible for us to change and for us to choose how we react and how we behave rather than being unthinking creatures of habit. It doesn't make it easy. Indeed, we usually are creatures of habit and our behavior is under the control of environmental stimuli far more than we usually realize, but having the ability to exercise inhibitory control creates the possibility of change and choice. ... The subthalamic nucleus appears to play a critical role in preventing such impulsive or premature responding (Frank 2006). - Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 13: Higher Cognitive Function and Behavioral Control". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 313–21. ISBN 978-0-07-148127-4.
• Executive function, the cognitive control of behavior, depends on the prefrontal cortex, which is highly developed in higher primates and especially humans.
• Working memory is a short-term, capacity-limited cognitive buffer that stores information and permits its manipulation to guide decision-making and behavior. ...
These diverse inputs and back projections to both cortical and subcortical structures put the prefrontal cortex in a position to exert what is often called "top-down" control or cognitive control of behavior. ... The prefrontal cortex receives inputs not only from other cortical regions, including association cortex, but also, via the thalamus, inputs from subcortical structures subserving emotion and motivation, such as the amygdala (Chapter 14) and ventral striatum (or nucleus accumbens; Chapter 15). ...
In conditions in which prepotent responses tend to dominate behavior, such as in drug addiction, where drug cues can elicit drug seeking (Chapter 15), or in attention deficit hyperactivity disorder (ADHD; described below), significant negative consequences can result. ... ADHD can be conceptualized as a disorder of executive function; specifically, ADHD is characterized by reduced ability to exert and maintain cognitive control of behavior. Compared with healthy individuals, those with ADHD have diminished ability to suppress inappropriate prepotent responses to stimuli (impaired response inhibition) and diminished ability to inhibit responses to irrelevant stimuli (impaired interference suppression). ... Functional neuroimaging in humans demonstrates activation of the prefrontal cortex and caudate nucleus (part of the striatum) in tasks that demand inhibitory control of behavior. Subjects with ADHD exhibit less activation of the medial prefrontal cortex than healthy controls even when they succeed in such tasks and utilize different circuits. ... Early results with structural MRI show thinning of the cerebral cortex in ADHD subjects compared with age-matched controls in prefrontal cortex and posterior parietal cortex, areas involved in working memory and attention. - Vassoler FM, Sadri-Vakili G (2014). "Mechanisms of transgenerational inheritance of addictive-like behaviors". Neuroscience. 264: 198–206. doi:10.1016/j.neuroscience.2013.07.064. PMC 3872494. PMID 23920159.
However, the components that are responsible for the heritability of characteristics that make an individual more susceptible to drug addiction in humans remain largely unknown given that patterns of inheritance cannot be explained by simple genetic mechanisms (Cloninger et al., 1981; Schuckit et al., 1972). The environment also plays a large role in the development of addiction as evidenced by great societal variability in drug use patterns between countries and across time (UNODC, 2012). Therefore, both genetics and the environment contribute to an individual's vulnerability to become addicted following an initial exposure to drugs of abuse. ...
The evidence presented here demonstrates that rapid environmental adaptation occurs following exposure to a number of stimuli. Epigenetic mechanisms represent the key components by which the environment can influence genetics, and they provide the missing link between genetic heritability and environmental influences on the behavioral and physiological phenotypes of the offspring. - Douglas KR, Chan G, Gelernter J, Arias AJ, Anton RF, Weiss RD, et al. (January 2010). "Adverse childhood events as risk factors for substance dependence: partial mediation by mood and anxiety disorders". Addictive Behaviors. 35 (1): 7–13. doi:10.1016/j.addbeh.2009.07.004. PMC 2763992. PMID 19720467.
- Mirin SM, Weiss RD, Griffin ML, Michael JL (1 January 1991). "Psychopathology in drug abusers and their families". Comprehensive Psychiatry. 32 (1): 36–51. doi:10.1016/0010-440X(91)90068-N. PMID 2001619.
- Mayfield RD, Harris RA, Schuckit MA (May 2008). "Genetic factors influencing alcohol dependence". British Journal of Pharmacology. 154 (2): 275–287. doi:10.1038/bjp.2008.88. PMC 2442454. PMID 18362899.
- Kendler KS, Neale MC, Heath AC, Kessler RC, Eaves LJ (May 1994). "A twin-family study of alcoholism in women". The American Journal of Psychiatry. 151 (5): 707–715. doi:10.1176/ajp.151.5.707. PMID 8166312.
- Crowe JR. "Genetics of alcoholism". Alcohol Health and Research World: 1–11. Retrieved 13 December 2017.
- Melemis SM. "The Genetics of Addiction – Is Addiction a Disease?". I Want to Change My Life. Retrieved 17 September 2018.
- Clarke TK, Crist RC, Kampman KM, Dackis CA, Pettinati HM, O'Brien CP, Oslin DW, Ferraro TN, Lohoff FW, Berrettini WH (2013). "Low frequency genetic variants in the μ-opioid receptor (OPRM1) affect risk for addiction to heroin and cocaine". Neuroscience Letters. 542: 71–75. doi:10.1016/j.neulet.2013.02.018. PMC 3640707. PMID 23454283.
- Hall FS, Drgonova J, Jain S, Uhl GR (December 2013). "Implications of genome wide association studies for addiction: are our a priori assumptions all wrong?". Pharmacology & Therapeutics. 140 (3): 267–79. doi:10.1016/j.pharmthera.2013.07.006. PMC 3797854. PMID 23872493.
- Yang H, Ma J (August 2021). "How the COVID-19 pandemic impacts tobacco addiction: Changes in smoking behavior and associations with well-being". Addictive Behaviors. 119: 106917. doi:10.1016/j.addbeh.2021.106917. PMC 9186053. PMID 33862579. S2CID 233278782.
- "What are risk factors and protective factors?". National Institute on Drug Abuse. Retrieved 13 December 2017.
- "Understanding Drug Use and Addiction". www.drugabuse.gov. National Institute on Drug Abuse. 6 June 2018. Retrieved 29 May 2020.
- Lewis M (October 2018). Longo DL (ed.). "Brain Change in Addiction as Learning, Not Disease". The New England Journal of Medicine. 379 (16): 1551–1560. doi:10.1056/NEJMra1602872. PMID 30332573. S2CID 205117578.
Addictive activities are determined neither solely by brain changes nor solely by social conditions ... the narrowing seen in addiction takes place within the behavioral repertoire, the social surround, and the brain — all at the same time.
- "Adverse Childhood Experiences". samhsa.gov. Rockville, Maryland, United States: Substance Abuse and Mental Health Services Administration. Archived from the original on 9 October 2016. Retrieved 26 September 2016.
- Enoch MA (March 2011). "The role of early life stress as a predictor for alcohol and drug dependence". Psychopharmacology. 214 (1): 17–31. doi:10.1007/s00213-010-1916-6. PMC 3005022. PMID 20596857.
- "Environmental Risk Factors". learn.genetics.utah.edu. Archived from the original on 17 September 2018. Retrieved 17 September 2018.
- Spear LP (June 2000). "The adolescent brain and age-related behavioral manifestations". Neuroscience and Biobehavioral Reviews. 24 (4): 417–63. CiteSeerX 10.1.1.461.3295. doi:10.1016/s0149-7634(00)00014-2. PMID 10817843. S2CID 14686245.
- Hammond CJ, Mayes LC, Potenza MN (April 2014). "Neurobiology of adolescent substance use and addictive behaviors: treatment implications". Adolescent Medicine. 25 (1): 15–32. PMC 4446977. PMID 25022184.
- Catalano RF, Hawkins JD, Wells EA, Miller J, Brewer D (1990). "Evaluation of the effectiveness of adolescent drug abuse treatment, assessment of risks for relapse, and promising approaches for relapse prevention". The International Journal of the Addictions. 25 (9A–10A): 1085–140. doi:10.3109/10826089109081039. PMID 2131328.
- Perepletchikova F, Krystal JH, Kaufman J (November 2008). "Practitioner review: adolescent alcohol use disorders: assessment and treatment issues". Journal of Child Psychology and Psychiatry, and Allied Disciplines. 49 (11): 1131–54. doi:10.1111/j.1469-7610.2008.01934.x. PMC 4113213. PMID 19017028.
- "Nationwide Trends". National Institute on Drug Abuse. June 2015. Retrieved 15 December 2017.
- "Addiction Statistics – Facts on Drug and Alcohol Addiction". AddictionCenter. Retrieved 17 September 2018.
- SAMHSA. "Risk and Protective Factors". Substance Abuse and Mental Health Administration. Archived from the original on 8 December 2016. Retrieved 19 December 2016.
- "Infographic – Risk Factors of Addiction | Recovery Research Institute". www.recoveryanswers.org. Archived from the original on 17 December 2016. Retrieved 19 December 2016.
- "Drug addiction Risk factors – Mayo Clinic". www.mayoclinic.org. Retrieved 19 December 2016.
- "The Connection Between Mental Illness and Substance Abuse | Dual Diagnosis". Dual Diagnosis. Retrieved 17 September 2018.
- Yuan TF, Li A, Sun X, Ouyang H, Campos C, Rocha NB, Arias-Carrión O, Machado S, Hou G, So KF (2015). "Transgenerational Inheritance of Paternal Neurobehavioral Phenotypes: Stress, Addiction, Ageing and Metabolism". Mol. Neurobiol. 53 (9): 6367–76. doi:10.1007/s12035-015-9526-2. hdl:10400.22/7331. PMID 26572641. S2CID 25694221.
- Ruffle JK (November 2014). "Molecular neurobiology of addiction: what's all the (Δ)FosB about?". Am. J. Drug Alcohol Abuse. 40 (6): 428–37. doi:10.3109/00952990.2014.933840. PMID 25083822. S2CID 19157711.
ΔFosB is an essential transcription factor implicated in the molecular and behavioral pathways of addiction following repeated drug exposure. The formation of ΔFosB in multiple brain regions, and the molecular pathway leading to the formation of AP-1 complexes is well understood. The establishment of a functional purpose for ΔFosB has allowed further determination as to some of the key aspects of its molecular cascades[…]As a consequence of our improved understanding of ΔFosB in addiction, it is possible to evaluate the addictive potential of current medications (119), as well as use it as a biomarker for assessing the efficacy of therapeutic interventions (121,122,124). Some of these proposed interventions have limitations (125) or are in their infancy (75). However, it is hoped that some of these preliminary findings may lead to innovative treatments, which are much needed in addiction.
- Biliński P, Wojtyła A, Kapka-Skrzypczak L, Chwedorowicz R, Cyranka M, Studziński T (2012). "Epigenetic regulation in drug addiction". Ann. Agric. Environ. Med. 19 (3): 491–96. PMID 23020045.
[…]ΔFosB is considered a primary and causative transcription factor in creating new neural connections in the reward centre, prefrontal cortex, and other regions of the limbic system. This is reflected in the increased, stable and long-lasting level of sensitivity to cocaine and other drugs, and tendency to relapse even after long periods of abstinence.
- Renthal W, Nestler EJ (September 2009). "Chromatin regulation in drug addiction and depression". Dialogues in Clinical Neuroscience. 11 (3): 257–268. PMC 2834246. PMID 19877494.
[Psychostimulants] increase cAMP levels in striatum, which activates protein kinase A (PKA) and leads to phosphorylation of its targets. This includes the cAMP response element binding protein (CREB), the phosphorylation of which induces its association with the histone acetyltransferase, CREB binding protein (CBP) to acetylate histones and facilitate gene activation. This is known to occur on many genes including fosB and c-fos in response to psychostimulant exposure. ΔFosB is also upregulated by chronic psychostimulant treatments, and is known to activate certain genes (eg, cdk5) and repress others (eg, c-fos) where it recruits HDAC1 as a corepressor. ... Chronic exposure to psychostimulants increases glutamatergic [signaling] from the prefrontal cortex to the NAc. Glutamatergic signaling elevates Ca2+ levels in NAc postsynaptic elements where it activates CaMK (calcium/calmodulin protein kinases) signaling, which, in addition to phosphorylating CREB, also phosphorylates HDAC5.
Figure 2: Psychostimulant-induced signaling events - Broussard JI (January 2012). "Co-transmission of dopamine and glutamate". The Journal of General Physiology. 139 (1): 93–96. doi:10.1085/jgp.201110659. PMC 3250102. PMID 22200950.
Coincident and convergent input often induces plasticity on a postsynaptic neuron. The NAc integrates processed information about the environment from basolateral amygdala, hippocampus, and prefrontal cortex (PFC), as well as projections from midbrain dopamine neurons. Previous studies have demonstrated how dopamine modulates this integrative process. For example, high frequency stimulation potentiates hippocampal inputs to the NAc while simultaneously depressing PFC synapses (Goto and Grace, 2005). The converse was also shown to be true; stimulation at PFC potentiates PFC–NAc synapses but depresses hippocampal–NAc synapses. In light of the new functional evidence of midbrain dopamine/glutamate co-transmission (references above), new experiments of NAc function will have to test whether midbrain glutamatergic inputs bias or filter either limbic or cortical inputs to guide goal-directed behavior.
- Kanehisa Laboratories (10 October 2014). "Amphetamine – Homo sapiens (human)". KEGG Pathway. Retrieved 31 October 2014.
Most addictive drugs increase extracellular concentrations of dopamine (DA) in nucleus accumbens (NAc) and medial prefrontal cortex (mPFC), projection areas of mesocorticolimbic DA neurons and key components of the "brain reward circuit". Amphetamine achieves this elevation in extracellular levels of DA by promoting efflux from synaptic terminals. ... Chronic exposure to amphetamine induces a unique transcription factor delta FosB, which plays an essential role in long-term adaptive changes in the brain.
- Cadet JL, Brannock C, Jayanthi S, Krasnova IN (2015). "Transcriptional and epigenetic substrates of methamphetamine addiction and withdrawal: evidence from a long-access self-administration model in the rat". Molecular Neurobiology. 51 (2): 696–717 (Figure 1). doi:10.1007/s12035-014-8776-8. PMC 4359351. PMID 24939695.
- Robison AJ, Nestler EJ (November 2011). "Transcriptional and epigenetic mechanisms of addiction". Nature Reviews Neuroscience. 12 (11): 623–637. doi:10.1038/nrn3111. PMC 3272277. PMID 21989194.
ΔFosB serves as one of the master control proteins governing this structural plasticity. ... ΔFosB also represses G9a expression, leading to reduced repressive histone methylation at the cdk5 gene. The net result is gene activation and increased CDK5 expression. ... In contrast, ΔFosB binds to the c-fos gene and recruits several co-repressors, including HDAC1 (histone deacetylase 1) and SIRT 1 (sirtuin 1). ... The net result is c-fos gene repression.
Figure 4: Epigenetic basis of drug regulation of gene expression - Nestler EJ (December 2012). "Transcriptional mechanisms of drug addiction". Clinical Psychopharmacology and Neuroscience. 10 (3): 136–143. doi:10.9758/cpn.2012.10.3.136. PMC 3569166. PMID 23430970.
The 35-37 kD ΔFosB isoforms accumulate with chronic drug exposure due to their extraordinarily long half-lives. ... As a result of its stability, the ΔFosB protein persists in neurons for at least several weeks after cessation of drug exposure. ... ΔFosB overexpression in nucleus accumbens induces NFκB ... In contrast, the ability of ΔFosB to repress the c-Fos gene occurs in concert with the recruitment of a histone deacetylase and presumably several other repressive proteins such as a repressive histone methyltransferase
- Nestler EJ (October 2008). "Transcriptional mechanisms of addiction: Role of ΔFosB". Philosophical Transactions of the Royal Society B: Biological Sciences. 363 (1507): 3245–3255. doi:10.1098/rstb.2008.0067. PMC 2607320. PMID 18640924.
Recent evidence has shown that ΔFosB also represses the c-fos gene that helps create the molecular switch—from the induction of several short-lived Fos family proteins after acute drug exposure to the predominant accumulation of ΔFosB after chronic drug exposure
- Hyman SE, Malenka RC, Nestler EJ (2006). "Neural mechanisms of addiction: the role of reward-related learning and memory". Annu. Rev. Neurosci. 29: 565–98. doi:10.1146/annurev.neuro.29.051605.113009. PMID 16776597.
- Steiner H, Van Waes V (January 2013). "Addiction-related gene regulation: risks of exposure to cognitive enhancers vs. other psychostimulants". Prog. Neurobiol. 100: 60–80. doi:10.1016/j.pneurobio.2012.10.001. PMC 3525776. PMID 23085425.
- Kanehisa Laboratories (2 August 2013). "Alcoholism – Homo sapiens (human)". KEGG Pathway. Retrieved 10 April 2014.
- Kim Y, Teylan MA, Baron M, Sands A, Nairn AC, Greengard P (February 2009). "Methylphenidate-induced dendritic spine formation and DeltaFosB expression in nucleus accumbens". Proc. Natl. Acad. Sci. USA. 106 (8): 2915–20. Bibcode:2009PNAS..106.2915K. doi:10.1073/pnas.0813179106. PMC 2650365. PMID 19202072.
- Nestler EJ (January 2014). "Epigenetic mechanisms of drug addiction". Neuropharmacology. 76 (Pt B): 259–68. doi:10.1016/j.neuropharm.2013.04.004. PMC 3766384. PMID 23643695.
Short-term increases in histone acetylation generally promote behavioral responses to the drugs, while sustained increases oppose cocaine's effects, based on the actions of systemic or intra-NAc administration of HDAC inhibitors. ... Genetic or pharmacological blockade of G9a in the NAc potentiates behavioral responses to cocaine and opiates, whereas increasing G9a function exerts the opposite effect (Maze et al., 2010; Sun et al., 2012a). Such drug-induced downregulation of G9a and H3K9me2 also sensitizes animals to the deleterious effects of subsequent chronic stress (Covington et al., 2011). Downregulation of G9a increases the dendritic arborization of NAc neurons, and is associated with increased expression of numerous proteins implicated in synaptic function, which directly connects altered G9a/H3K9me2 in the synaptic plasticity associated with addiction (Maze et al., 2010).
G9a appears to be a critical control point for epigenetic regulation in NAc, as we know it functions in two negative feedback loops. It opposes the induction of ΔFosB, a long-lasting transcription factor important for drug addiction (Robison and Nestler, 2011), while ΔFosB in turn suppresses G9a expression (Maze et al., 2010; Sun et al., 2012a). ... Also, G9a is induced in NAc upon prolonged HDAC inhibition, which explains the paradoxical attenuation of cocaine's behavioral effects seen under these conditions, as noted above (Kennedy et al., 2013). GABAA receptor subunit genes are among those that are controlled by this feedback loop. Thus, chronic cocaine, or prolonged HDAC inhibition, induces several GABAA receptor subunits in NAc, which is associated with increased frequency of inhibitory postsynaptic currents (IPSCs). In striking contrast, combined exposure to cocaine and HDAC inhibition, which triggers the induction of G9a and increased global levels of H3K9me2, leads to blockade of GABAA receptor and IPSC regulation. - Blum K, Werner T, Carnes S, Carnes P, Bowirrat A, Giordano J, Oscar-Berman M, Gold M (2012). "Sex, drugs, and rock 'n' roll: hypothesizing common mesolimbic activation as a function of reward gene polymorphisms". Journal of Psychoactive Drugs. 44 (1): 38–55. doi:10.1080/02791072.2012.662112. PMC 4040958. PMID 22641964.
It has been found that deltaFosB gene in the NAc is critical for reinforcing effects of sexual reward. Pitchers and colleagues (2010) reported that sexual experience was shown to cause DeltaFosB accumulation in several limbic brain regions including the NAc, medial pre-frontal cortex, VTA, caudate, and putamen, but not the medial preoptic nucleus. Next, the induction of c-Fos, a downstream (repressed) target of DeltaFosB, was measured in sexually experienced and naive animals. The number of mating-induced c-Fos-IR cells was significantly decreased in sexually experienced animals compared to sexually naive controls. Finally, DeltaFosB levels and its activity in the NAc were manipulated using viral-mediated gene transfer to study its potential role in mediating sexual experience and experience-induced facilitation of sexual performance. Animals with DeltaFosB overexpression displayed enhanced facilitation of sexual performance with sexual experience relative to controls. In contrast, the expression of DeltaJunD, a dominant-negative binding partner of DeltaFosB, attenuated sexual experience-induced facilitation of sexual performance, and stunted long-term maintenance of facilitation compared to DeltaFosB overexpressing group. Together, these findings support a critical role for DeltaFosB expression in the NAc in the reinforcing effects of sexual behavior and sexual experience-induced facilitation of sexual performance. ... both drug addiction and sexual addiction represent pathological forms of neuroplasticity along with the emergence of aberrant behaviors involving a cascade of neurochemical changes mainly in the brain's rewarding circuitry.
- Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 15: Reinforcement and addictive disorders". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 384–85. ISBN 978-0-07-148127-4.
- Salamone JD (1992). "Complex motor and sensorimotor functions of striatal and accumbens dopamine: involvement in instrumental behavior processes". Psychopharmacology. 107 (2–3): 160–74. doi:10.1007/bf02245133. PMID 1615120. S2CID 30545845.
- Kauer JA, Malenka RC (November 2007). "Synaptic plasticity and addiction". Nature Reviews. Neuroscience. 8 (11): 844–58. doi:10.1038/nrn2234. PMID 17948030. S2CID 38811195.
- Witten IB, Lin SC, Brodsky M, Prakash R, Diester I, Anikeeva P, et al. (December 2010). "Cholinergic interneurons control local circuit activity and cocaine conditioning". Science. 330 (6011): 1677–81. Bibcode:2010Sci...330.1677W. doi:10.1126/science.1193771. PMC 3142356. PMID 21164015.
- Nestler EJ, Barrot M, Self DW (September 2001). "DeltaFosB: a sustained molecular switch for addiction". Proc. Natl. Acad. Sci. U.S.A. 98 (20): 11042–46. Bibcode:2001PNAS...9811042N. doi:10.1073/pnas.191352698. PMC 58680. PMID 11572966.
Although the ΔFosB signal is relatively long-lived, it is not permanent. ΔFosB degrades gradually and can no longer be detected in [the] brain after 1–2 months of drug withdrawal ... Indeed, ΔFosB is the longest-lived adaptation known to occur in [the] adult brain, not only in response to drugs of abuse, but to any other perturbation (that doesn't involve lesions) as well.
- Jones S, Bonci A (2005). "Synaptic plasticity and drug addiction". Current Opinion in Pharmacology. 5 (1): 20–25. doi:10.1016/j.coph.2004.08.011. PMID 15661621.
- Eisch AJ, Harburg GC (2006). "Opiates, psychostimulants, and adult hippocampal neurogenesis: Insights for addiction and stem cell biology". Hippocampus. 16 (3): 271–86. doi:10.1002/hipo.20161. PMID 16411230. S2CID 23667629.
- Rang HP (2003). Pharmacology. Edinburgh: Churchill Livingstone. p. 596. ISBN 978-0-443-07145-4.
- Kourrich S, Rothwell PE, Klug JR, Thomas MJ (2007). "Cocaine experience controls bidirectional synaptic plasticity in the nucleus accumbens". J. Neurosci. 27 (30): 7921–28. doi:10.1523/JNEUROSCI.1859-07.2007. PMC 6672735. PMID 17652583.
- Kalivas PW, Volkow ND (August 2005). "The neural basis of addiction: a pathology of motivation and choice". The American Journal of Psychiatry. 162 (8): 1403–13. doi:10.1176/appi.ajp.162.8.1403. PMID 16055761.
- Floresco SB, Ghods-Sharifi S (February 2007). "Amygdala-prefrontal cortical circuitry regulates effort-based decision making". Cerebral Cortex. 17 (2): 251–60. CiteSeerX 10.1.1.335.4681. doi:10.1093/cercor/bhj143. PMID 16495432.
- Perry CJ, Zbukvic I, Kim JH, Lawrence AJ (October 2014). "Role of cues and contexts on drug-seeking behaviour". British Journal of Pharmacology. 171 (20): 4636–72. doi:10.1111/bph.12735. PMC 4209936. PMID 24749941.
- Volkow ND, Fowler JS, Wang GJ, Swanson JM, Telang F (2007). "Dopamine in drug abuse and addiction: results of imaging studies and treatment implications". Arch. Neurol. 64 (11): 1575–79. doi:10.1001/archneur.64.11.1575. PMID 17998440.
- "Drugs, Brains, and Behavior: The Science of Addiction". National Institute on Drug Abuse.
- "Understanding Drug Abuse and Addiction". National Institute on Drug Abuse. November 2012. Archived from the original on 16 August 2011. Retrieved 12 February 2015.
- Nestler EJ (October 2008). "Review. Transcriptional mechanisms of addiction: role of DeltaFosB". Philosophical Transactions of the Royal Society of London. Series B, Biological Sciences. 363 (1507): 3245–55. doi:10.1098/rstb.2008.0067. PMC 2607320. PMID 18640924.
Recent evidence has shown that ΔFosB also represses the c-fos gene that helps create the molecular switch – from the induction of several short-lived Fos family proteins after acute drug exposure to the predominant accumulation of ΔFosB after chronic drug exposure – cited earlier (Renthal et al. in press). The mechanism responsible for ΔFosB repression of c-fos expression is complex and is covered below. ...
Examples of validated targets for ΔFosB in nucleus accumbens ... GluR2 ... dynorphin ... Cdk5 ... NFκB ... c-Fos
Table 3 - Berridge KC (April 2012). "From prediction error to incentive salience: mesolimbic computation of reward motivation". Eur. J. Neurosci. 35 (7): 1124–43. doi:10.1111/j.1460-9568.2012.07990.x. PMC 3325516. PMID 22487042.
Here I discuss how mesocorticolimbic mechanisms generate the motivation component of incentive salience. Incentive salience takes Pavlovian learning and memory as one input and as an equally important input takes neurobiological state factors (e.g. drug states, appetite states, satiety states) that can vary independently of learning. Neurobiological state changes can produce unlearned fluctuations or even reversals in the ability of a previously learned reward cue to trigger motivation. Such fluctuations in cue-triggered motivation can dramatically depart from all previously learned values about the associated reward outcome. ... Associative learning and prediction are important contributors to motivation for rewards. Learning gives incentive value to arbitrary cues such as a Pavlovian conditioned stimulus (CS) that is associated with a reward (unconditioned stimulus or UCS). Learned cues for reward are often potent triggers of desires. For example, learned cues can trigger normal appetites in everyone, and can sometimes trigger compulsive urges and relapse in individuals with addictions.
Cue-triggered 'wanting' for the UCS
A brief CS encounter (or brief UCS encounter) often primes a pulse of elevated motivation to obtain and consume more reward UCS. This is a signature feature of incentive salience.
Cue as attractive motivational magnets
When a Pavlovian CS+ is attributed with incentive salience it not only triggers 'wanting' for its UCS, but often the cue itself becomes highly attractive – even to an irrational degree. This cue attraction is another signature feature of incentive salience ... Two recognizable features of incentive salience are often visible that can be used in neuroscience experiments: (i) UCS-directed 'wanting' – CS-triggered pulses of intensified 'wanting' for the UCS reward; and (ii) CS-directed 'wanting' – motivated attraction to the Pavlovian cue, which makes the arbitrary CS stimulus into a motivational magnet. - Malenka RC, Nestler EJ, Hyman SE (2009). Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. pp. 147–48, 366–67, 375–76. ISBN 978-0-07-148127-4.
VTA DA neurons play a critical role in motivation, reward-related behavior (Chapter 15), attention, and multiple forms of memory. This organization of the DA system, wide projection from a limited number of cell bodies, permits coordinated responses to potent new rewards. Thus, acting in diverse terminal fields, dopamine confers motivational salience ("wanting") on the reward itself or associated cues (nucleus accumbens shell region), updates the value placed on different goals in light of this new experience (orbital prefrontal cortex), helps consolidate multiple forms of memory (amygdala and hippocampus), and encodes new motor programs that will facilitate obtaining this reward in the future (nucleus accumbens core region and dorsal striatum). In this example, dopamine modulates the processing of sensorimotor information in diverse neural circuits to maximize the ability of the organism to obtain future rewards. ...
The brain reward circuitry that is targeted by addictive drugs normally mediates the pleasure and strengthening of behaviors associated with natural reinforcers, such as food, water, and sexual contact. Dopamine neurons in the VTA are activated by food and water, and dopamine release in the NAc is stimulated by the presence of natural reinforcers, such as food, water, or a sexual partner. ...
The NAc and VTA are central components of the circuitry underlying reward and memory of reward. As previously mentioned, the activity of dopaminergic neurons in the VTA appears to be linked to reward prediction. The NAc is involved in learning associated with reinforcement and the modulation of motoric responses to stimuli that satisfy internal homeostatic needs. The shell of the NAc appears to be particularly important to initial drug actions within reward circuitry; addictive drugs appear to have a greater effect on dopamine release in the shell than in the core of the NAc. ... If motivational drive is described in terms of wanting, and hedonic evaluation in terms of liking, it appears that wanting can be dissociated from liking and that dopamine may influence these phenomena differently. Differences between wanting and liking are confirmed in reports by humans with addictions, who state that their desire for drugs (wanting) increases with continued use even when pleasure (liking) decreases because of tolerance. - Edwards S (2016). "Reinforcement principles for addiction medicine; from recreational drug use to psychiatric disorder". Neuroscience for Addiction Medicine: From Prevention to Rehabilitation - Constructs and Drugs. Progress in Brain Research. Vol. 223. pp. 63–76. doi:10.1016/bs.pbr.2015.07.005. ISBN 978-0-444-63545-7. PMID 26806771.
An important dimension of reinforcement highly relevant to the addiction process (and particularly relapse) is secondary reinforcement (Stewart, 1992). Secondary reinforcers (in many cases also considered conditioned reinforcers) likely drive the majority of reinforcement processes in humans. In the specific case of drug addiction, cues and contexts that are intimately and repeatedly associated with drug use will often themselves become reinforcing ... A fundamental piece of Robinson and Berridge's incentive-sensitization theory of addiction posits that the incentive value or attractive nature of such secondary reinforcement processes, in addition to the primary reinforcers themselves, may persist and even become sensitized over time in league with the development of drug addiction (Robinson and Berridge, 1993).
- Berridge KC, Kringelbach ML (May 2015). "Pleasure systems in the brain". Neuron. 86 (3): 646–664. doi:10.1016/j.neuron.2015.02.018. PMC 4425246. PMID 25950633.
- Walker DM, Cates HM, Heller EA, Nestler EJ (February 2015). "Regulation of chromatin states by drugs of abuse". Curr. Opin. Neurobiol. 30: 112–21. doi:10.1016/j.conb.2014.11.002. PMC 4293340. PMID 25486626.
Studies investigating general HDAC inhibition on behavioral outcomes have produced varying results but it seems that the effects are specific to the timing of exposure (either before, during or after exposure to drugs of abuse) as well as the length of exposure
- Petry NM, Rehbein F, Gentile DA, Lemmens JS, Rumpf HJ, Mößle T, Bischof G, Tao R, Fung DS, Borges G, Auriacombe M, González Ibáñez A, Tam P, O'Brien CP (September 2014). "An international consensus for assessing internet gaming disorder using the new DSM-5 approach". Addiction. 109 (9): 1399–406. doi:10.1111/add.12457. PMID 24456155.
- Torres G, Horowitz JM (1999). "Drugs of abuse and brain gene expression". Psychosom Med. 61 (5): 630–50. CiteSeerX 10.1.1.326.4903. doi:10.1097/00006842-199909000-00007. PMID 10511013.
- "ICD-11 for Mortality and Morbidity Statistics - Disorders due to substance use or addictive behaviours". icd.who.int. Retrieved 10 April 2022.
- "ICD-11 for Mortality and Morbidity Statistics - Disorders due to substance use". icd.who.int. Retrieved 10 April 2022.
- "Drug abuse liability". www.cambridgecognition.com. Retrieved 9 March 2021.
- National Institute on Drug Abuse (20 August 2020). "Commonly Used Drugs Charts". National Institute on Drug Abuse. Retrieved 9 March 2021.
- Taylor SB, Lewis CR, Olive MF (February 2013). "The neurocircuitry of illicit psychostimulant addiction: acute and chronic effects in humans". Subst. Abuse Rehabil. 4: 29–43. doi:10.2147/SAR.S39684. PMC 3931688. PMID 24648786.
Initial drug use can be attributed to the ability of the drug to act as a reward (ie, a pleasurable emotional state or positive reinforcer), which can lead to repeated drug use and dependence.8,9 A great deal of research has focused on the molecular and neuroanatomical mechanisms of the initial rewarding or reinforcing effect of drugs of abuse. ... At present, no pharmacological therapy has been approved by the FDA to treat psychostimulant addiction. Many drugs have been tested, but none have shown conclusive efficacy with tolerable side effects in humans.172 ... A new emphasis on larger-scale biomarker, genetic, and epigenetic research focused on the molecular targets of mental disorders has been recently advocated.212 In addition, the integration of cognitive and behavioral modification of circuit-wide neuroplasticity (i.e., computer-based training to enhance executive function) may prove to be an effective adjunct-treatment approach for addiction, particularly when combined with cognitive enhancers.198,213–216 Furthermore, in order to be effective, all pharmacological or biologically based treatments for addiction need to be integrated into other established forms of addiction rehabilitation, such as cognitive behavioral therapy, individual and group psychotherapy, behavior-modification strategies, twelve-step programs, and residential treatment facilities.
- Magnusson D (1998). Theoretical Models of Human development. New York: John Wiley & sons. pp. 685–759.
- Schlosser AV (September 2018). "'They Medicated Me Out': Social Flesh and Embodied Citizenship in Addiction Treatment". Contemporary Drug Problems. 45 (3): 188–207. doi:10.1177/0091450918781590. S2CID 149842084.
- Wolfe D, Saucier R (February 2021). "Biotechnologies and the future of opioid addiction treatments". The International Journal on Drug Policy. 88: 103041. doi:10.1016/j.drugpo.2020.103041. PMID 33246267. S2CID 227191111.
- Walter M, Dürsteler KM, Petitjean SA, Wiesbeck GA, Euler S, Sollberger D, et al. (April 2015). "[Psychosocial Treatment of Addictive Disorders--An Overview of Psychotherapeutic Options and their Efficacy]" [Psychosocial Treatment of Addictive Disorders – An Overview of Psychotherapeutic Options and their Efficacy]. Fortschritte der Neurologie-Psychiatrie (in German). 83 (4): 201–210. doi:10.1055/s-0034-1399338. PMID 25893493.
- Carroll ME, Smethells JR (February 2016). "Sex Differences in Behavioral Dyscontrol: Role in Drug Addiction and Novel Treatments". Front. Psychiatry. 6: 175. doi:10.3389/fpsyt.2015.00175. PMC 4745113. PMID 26903885.
Environmental Enrichment ...
In humans, non-drug rewards delivered in a contingency management (CM) format successfully reduced drug dependence ... In general, CM programs promote drug abstinence through a combination of positive reinforcement for drug-free urine samples. For instance, voucher-based reinforcement therapy in which medication compliance, therapy session attendance, and negative drug screenings reinforced with vouchers to local business (e.g., movie theater, restaurants, etc.) directly reinforces drug abstinence, provides competing reinforcers, enriches the environment, and it is a robust treatment across a broad range of abused drugs (189). ...
Physical Exercise
There is accelerating evidence that physical exercise is a useful treatment for preventing and reducing drug addiction ... In some individuals, exercise has its own rewarding effects, and a behavioral economic interaction may occur, such that physical and social rewards of exercise can substitute for the rewarding effects of drug abuse. ... The value of this form of treatment for drug addiction in laboratory animals and humans is that exercise, if it can substitute for the rewarding effects of drugs, could be self-maintained over an extended period of time. Work to date in [laboratory animals and humans] regarding exercise as a treatment for drug addiction supports this hypothesis. ... However, a RTC study was recently reported by Rawson et al. (226), whereby they used 8 weeks of exercise as a post-residential treatment for METH addiction, showed a significant reduction in use (confirmed by urine screens) in participants who had been using meth 18 days or less a month. ... Animal and human research on physical exercise as a treatment for stimulant addiction indicates that this is one of the most promising treatments on the horizon. [(emphasis added)] - Lynch WJ, Peterson AB, Sanchez V, Abel J, Smith MA (September 2013). "Exercise as a novel treatment for drug addiction: a neurobiological and stage-dependent hypothesis". Neurosci Biobehav Rev. 37 (8): 1622–44. doi:10.1016/j.neubiorev.2013.06.011. PMC 3788047. PMID 23806439.
[exercise] efficacy may be related to its ability to normalize glutamatergic and dopaminergic signaling and reverse drug-induced changes in chromatin via epigenetic interactions with brain-derived neurotrophic factor (BDNF) in the reward pathway. ... these data show that exercise can affect dopaminergic signaling at many different levels, which may underlie its ability to modify vulnerability during drug use initiation. Exercise also produces neuroadaptations that may influence an individual's vulnerability to initiate drug use. Consistent with this idea, chronic moderate levels of forced treadmill running blocks not only subsequent methamphetamine-induced conditioned place preference, but also stimulant-induced increases in dopamine release in the NAc (Chen et al., 2008) and striatum (Marques et al., 2008). ... [These] findings indicate the efficacy of exercise at reducing drug intake in drug-dependent individuals ... wheel running [reduces] methamphetamine self-administration under extended access conditions (Engelmann et al., 2013) ... These findings suggest that exercise may "magnitude"-dependently prevent the development of an addicted phenotype possibly by blocking/reversing behavioral and neuro-adaptive changes that develop during and following extended access to the drug. ... Exercise has been proposed as a treatment for drug addiction that may reduce drug craving and risk of relapse. Although few clinical studies have investigated the efficacy of exercise for preventing relapse, the few studies that have been conducted generally report a reduction in drug craving and better treatment outcomes (see Table 4). ... Taken together, these data suggest that the potential benefits of exercise during relapse, particularly for relapse to psychostimulants, may be mediated via chromatin remodeling and possibly lead to greater treatment outcomes.
- Linke SE, Ussher M (2015). "Exercise-based treatments for substance use disorders: evidence, theory, and practicality". Am J Drug Alcohol Abuse. 41 (1): 7–15. doi:10.3109/00952990.2014.976708. PMC 4831948. PMID 25397661.
The limited research conducted suggests that exercise may be an effective adjunctive treatment for SUDs. In contrast to the scarce intervention trials to date, a relative abundance of literature on the theoretical and practical reasons supporting the investigation of this topic has been published. ... numerous theoretical and practical reasons support exercise-based treatments for SUDs, including psychological, behavioral, neurobiological, nearly universal safety profile, and overall positive health effects.
- Zhou Y, Zhao M, Zhou C, Li R (July 2015). "Sex differences in drug addiction and response to exercise intervention: From human to animal studies". Front. Neuroendocrinol. 40: 24–41. doi:10.1016/j.yfrne.2015.07.001. PMC 4712120. PMID 26182835.
Collectively, these findings demonstrate that exercise may serve as a substitute or competition for drug abuse by changing ΔFosB or cFos immunoreactivity in the reward system to protect against later or previous drug use. ... As briefly reviewed above, a large number of human and rodent studies clearly show that there are sex differences in drug addiction and exercise. The sex differences are also found in the effectiveness of exercise on drug addiction prevention and treatment, as well as underlying neurobiological mechanisms. The postulate that exercise serves as an ideal intervention for drug addiction has been widely recognized and used in human and animal rehabilitation. ... In particular, more studies on the neurobiological mechanism of exercise and its roles in preventing and treating drug addiction are needed.
- Sachdeva A, Choudhary M, Chandra M (September 2015). "Alcohol Withdrawal Syndrome: Benzodiazepines and Beyond". Journal of Clinical and Diagnostic Research. 9 (9): VE01–VE07. doi:10.7860/JCDR/2015/13407.6538. PMC 4606320. PMID 26500991.
- Soyka M, Roesner S (December 2006). "New pharmacological approaches for the treatment of alcoholism". Expert Opinion on Pharmacotherapy. 7 (17): 2341–53. doi:10.1517/14656566.7.17.2341. PMID 17109610. S2CID 2587029.
- Pettinati HM, Rabinowitz AR (October 2006). "Choosing the right medication for the treatment of alcoholism". Current Psychiatry Reports. 8 (5): 383–88. doi:10.1007/s11920-006-0040-0. PMID 16968619. S2CID 39826013.
- Bouza C, Angeles M, Magro A, Muñoz A, Amate JM (July 2004). "Efficacy and safety of naltrexone and acamprosate in the treatment of alcohol dependence: a systematic review". Addiction. 99 (7): 811–28. doi:10.1111/j.1360-0443.2004.00763.x. PMID 15200577.
- Williams SH (November 2005). "Medications for treating alcohol dependence". American Family Physician. 72 (9): 1775–80. PMID 16300039.
- Rösner S, Hackl-Herrwerth A, Leucht S, Vecchi S, Srisurapanont M, Soyka M (December 2010). Srisurapanont M (ed.). "Opioid antagonists for alcohol dependence". The Cochrane Database of Systematic Reviews (12): CD001867. doi:10.1002/14651858.CD001867.pub2. PMID 21154349.
- Fratta W, Fattore L (August 2013). "Molecular mechanisms of cannabinoid addiction". Curr. Opin. Neurobiol. 23 (4): 487–92. doi:10.1016/j.conb.2013.02.002. PMID 23490548. S2CID 40849553.
14. Nguyen PT, Schmid CL, Raehal KM, Selley DE, Bohn LM, Sim-Selley LJ: b-Arrestin2 regulates cannabinoid CB1 receptor signaling and adaptation in a central nervous system region dependent manner. Biol Psychiatry 2012, 71:714–24.
A pioneering study revealing both positive and negative modulatory effects of beta-arrestin2 on THC tolerance. By demonstrating that tolerance to antinociception is reduced whereas tolerance to catalepsy is enhanced in beta-arrestin2 knockout mice, authors suggest that development of cannabinoid agonists that minimize interactions between CB1Rs and beta-arrestin2 might produce improved cannabinoid analgesics with reduced motor suppression, and be therapeutically beneficial. - Sabioni, Pamela; Le Foll, Bernard (1 April 2019). "Psychosocial and Pharmacological Interventions for the Treatment of Cannabis Use Disorder". FOCUS. 17 (2): 163–168. doi:10.1176/appi.focus.17202. ISSN 1541-4094. PMC 6527000. PMID 32021586.
- Garwood CL, Potts LA (August 2007). "Emerging pharmacotherapies for smoking cessation". American Journal of Health-System Pharmacy. 64 (16): 1693–1698. doi:10.2146/ajhp060427. PMID 17687057.
- Crooks PA, Bardo MT, Dwoskin LP (2014). "Nicotinic Receptor Antagonists as Treatments for Nicotine Abuse". Emerging Targets & Therapeutics in the Treatment of Psychostimulant Abuse. Advances in Pharmacology. Vol. 69. pp. 513–551. doi:10.1016/B978-0-12-420118-7.00013-5. ISBN 978-0-12-420118-7. PMC 4110698. PMID 24484986.
- Tutka, Piotr; Vinnikov, Denis; Courtney, Ryan J.; Benowitz, Neal L. (November 2019). "Cytisine for nicotine addiction treatment: a review of pharmacology, therapeutics and an update of clinical trial evidence for smoking cessation". Addiction. 114 (11): 1951–1969. doi:10.1111/add.14721. ISSN 1360-0443. PMID 31240783.
- Johnson RE, Chutuape MA, Strain EC, Walsh SL, Stitzer ML, Bigelow GE (November 2000). "A comparison of levomethadyl acetate, buprenorphine, and methadone for opioid dependence". The New England Journal of Medicine. 343 (18): 1290–7. doi:10.1056/NEJM200011023431802. PMID 11058673.
- Connock M, Juarez-Garcia A, Jowett S, Frew E, Liu Z, Taylor RJ, et al. (March 2007). "Methadone and buprenorphine for the management of opioid dependence: a systematic review and economic evaluation". Health Technology Assessment. 11 (9): 1–171, iii–iv. doi:10.3310/hta11090. PMID 17313907.
- Robertson JR, Raab GM, Bruce M, McKenzie JS, Storkey HR, Salter A (December 2006). "Addressing the efficacy of dihydrocodeine versus methadone as an alternative maintenance treatment for opiate dependence: A randomized controlled trial". Addiction. 101 (12): 1752–9. doi:10.1111/j.1360-0443.2006.01603.x. PMID 17156174.
- Qin BY (1998). "Advances in dihydroetorphine: From analgesia to detoxification". Drug Development Research. 39 (2): 131–34. doi:10.1002/(SICI)1098-2299(199610)39:2<131::AID-DDR3>3.0.CO;2-Q. S2CID 201878290.
- Metrebian N, Shanahan W, Wells B, Stimson GV (June 1998). "Feasibility of prescribing injectable heroin and methadone to opiate-dependent drug users: associated health gains and harm reductions". The Medical Journal of Australia. 168 (12): 596–600. doi:10.5694/j.1326-5377.1998.tb141444.x. PMID 9673620. S2CID 43302721.
- Metrebian N, Mott J, Carnwath Z, Carnwath T, Stimson GV, Sell L (2007). "Pathways into receiving a prescription for diamorphine (heroin) for the treatment of opiate dependence in the United kingdom". European Addiction Research. 13 (3): 144–7. doi:10.1159/000101550. PMID 17570910. S2CID 7397513.
- Kenna GA, Nielsen DM, Mello P, Schiesl A, Swift RM (2007). "Pharmacotherapy of dual substance abuse and dependence". CNS Drugs. 21 (3): 213–37. doi:10.2165/00023210-200721030-00003. PMID 17338593. S2CID 25979050.
- Strang J, McCambridge J, Best D, Beswick T, Bearn J, Rees S, Gossop M (May 2003). "Loss of tolerance and overdose mortality after inpatient opiate detoxification: follow up study". BMJ (Clinical Research Ed.). 326 (7396): 959–60. doi:10.1136/bmj.326.7396.959. PMC 153851. PMID 12727768.
- Stoops WW, Rush CR (May 2014). "Combination pharmacotherapies for stimulant use disorder: a review of clinical findings and recommendations for future research". Expert Rev Clin Pharmacol. 7 (3): 363–74. doi:10.1586/17512433.2014.909283. PMC 4017926. PMID 24716825.
Despite concerted efforts to identify a pharmacotherapy for managing stimulant use disorders, no widely effective medications have been approved.
- Perez-Mana C, Castells X, Torrens M, Capella D, Farre M (September 2013). "Efficacy of psychostimulant drugs for amphetamine abuse or dependence". Cochrane Database Syst. Rev. 9 (9): CD009695. doi:10.1002/14651858.CD009695.pub2. PMID 23996457.
To date, no pharmacological treatment has been approved for [addiction], and psychotherapy remains the mainstay of treatment. ... Results of this review do not support the use of psychostimulant medications at the tested doses as a replacement therapy
- Forray A, Sofuoglu M (February 2014). "Future pharmacological treatments for substance use disorders". Br. J. Clin. Pharmacol. 77 (2): 382–400. doi:10.1111/j.1365-2125.2012.04474.x. PMC 4014020. PMID 23039267.
- Grandy DK, Miller GM, Li JX (February 2016). ""TAARgeting Addiction" – The Alamo Bears Witness to Another Revolution: An Overview of the Plenary Symposium of the 2015 Behavior, Biology and Chemistry Conference". Drug Alcohol Depend. 159: 9–16. doi:10.1016/j.drugalcdep.2015.11.014. PMC 4724540. PMID 26644139.
When considered together with the rapidly growing literature in the field a compelling case emerges in support of developing TAAR1-selective agonists as medications for preventing relapse to psychostimulant abuse.
- Jing L, Li JX (August 2015). "Trace amine-associated receptor 1: A promising target for the treatment of psychostimulant addiction". Eur. J. Pharmacol. 761: 345–52. doi:10.1016/j.ejphar.2015.06.019. PMC 4532615. PMID 26092759.
Taken together, the data reviewed here strongly support that TAAR1 is implicated in the functional regulation of monoaminergic systems, especially dopaminergic system, and that TAAR1 serves as a homeostatic "brake" system that is involved in the modulation of dopaminergic activity. Existing data provided robust preclinical evidence supporting the development of TAAR1 agonists as potential treatment for psychostimulant abuse and addiction. ... Given that TAAR1 is primarily located in the intracellular compartments and existing TAAR1 agonists are proposed to get access to the receptors by translocation to the cell interior (Miller, 2011), future drug design and development efforts may need to take strategies of drug delivery into consideration (Rajendran et al., 2010).
- Liu JF, Li JX (December 2018). "Drug addiction: a curable mental disorder?". Acta Pharmacologica Sinica. 39 (12): 1823–1829. doi:10.1038/s41401-018-0180-x. PMC 6289334. PMID 30382181.
- Zalewska-Kaszubska J (November 2015). "Is immunotherapy an opportunity for effective treatment of drug addiction?". Vaccine. 33 (48): 6545–51. doi:10.1016/j.vaccine.2015.09.079. PMID 26432911.
- Laudenbach M, Baruffaldi F, Vervacke JS, Distefano MD, Titcombe PJ, Mueller DL, Tubo NJ, Griffith TS, Pravetoni M (June 2015). "The frequency of naive and early-activated hapten-specific B cell subsets dictates the efficacy of a therapeutic vaccine against prescription opioid abuse". J. Immunol. 194 (12): 5926–36. doi:10.4049/jimmunol.1500385. PMC 4458396. PMID 25972483.
Translation of therapeutic vaccines for addiction, cancer, or other chronic noncommunicable diseases has been slow because only a small subset of immunized subjects achieved effective Ab levels.
- Painter A. (2019) "Researchers working to develop vaccines to fight opioid addiction" Vtnews.vt.edu
- Cao DN, Shi JJ, Hao W, Wu N, Li J (March 2016). "Advances and challenges in pharmacotherapeutics for amphetamine-type stimulants addiction". Eur. J. Pharmacol. 780: 129–35. doi:10.1016/j.ejphar.2016.03.040. PMID 27018393.
- Moeller SJ, London ED, Northoff G (February 2016). "Neuroimaging markers of glutamatergic and GABAergic systems in drug addiction: Relationships to resting-state functional connectivity". Neurosci Biobehav Rev. 61: 35–52. doi:10.1016/j.neubiorev.2015.11.010. PMC 4731270. PMID 26657968.
- Agabio R, Colombo G (April 2015). "[GABAB receptor as therapeutic target for drug addiction: from baclofen to positive allosteric modulators]". Psychiatr. Pol. (in Polish). 49 (2): 215–23. doi:10.12740/PP/33911. PMID 26093587.
- Filip M, Frankowska M, Sadakierska-Chudy A, Suder A, Szumiec L, Mierzejewski P, Bienkowski P, Przegaliński E, Cryan JF (January 2015). "GABAB receptors as a therapeutic strategy in substance use disorders: focus on positive allosteric modulators". Neuropharmacology. 88: 36–47. doi:10.1016/j.neuropharm.2014.06.016. PMID 24971600. S2CID 207229988.
- McCowan TJ, Dhasarathy A, Carvelli L (February 2015). "The Epigenetic Mechanisms of Amphetamine". J. Addict. Prev. 2015 (Suppl 1). PMC 4955852. PMID 27453897.
Epigenetic modifications caused by addictive drugs play an important role in neuronal plasticity and in drug-induced behavioral responses. Although few studies have investigated the effects of AMPH on gene regulation (Table 1), current data suggest that AMPH acts at multiple levels to alter histone/DNA interaction and to recruit transcription factors which ultimately cause repression of some genes and activation of other genes. Importantly, some studies have also correlated the epigenetic regulation induced by AMPH with the behavioral outcomes caused by this drug, suggesting therefore that epigenetics remodeling underlies the behavioral changes induced by AMPH. If this proves to be true, the use of specific drugs that inhibit histone acetylation, methylation or DNA methylation might be an important therapeutic alternative to prevent and/or reverse AMPH addiction and mitigate the side effects generate by AMPH when used to treat ADHD.
- Primary references involving sodium butyrate:
• Kennedy PJ, Feng J, Robison AJ, Maze I, Badimon A, Mouzon E, Chaudhury D, Damez-Werno DM, Haggarty SJ, Han MH, Bassel-Duby R, Olson EN, Nestler EJ (April 2013). "Class I HDAC inhibition blocks cocaine-induced plasticity by targeted changes in histone methylation". Nat. Neurosci. 16 (4): 434–40. doi:10.1038/nn.3354. PMC 3609040. PMID 23475113.While acute HDAC inhibition enhances the behavioral effects of cocaine or amphetamine1,3,4,13,14, studies suggest that more chronic regimens block psychostimulant-induced plasticity3,5,11,12. ... The effects of pharmacological inhibition of HDACs on psychostimulant-induced plasticity appear to depend on the timecourse of HDAC inhibition. Studies employing co-administration procedures in which inhibitors are given acutely, just prior to psychostimulant administration, report heightened behavioral responses to the drug1,3,4,13,14. In contrast, experimental paradigms like the one employed here, in which HDAC inhibitors are administered more chronically, for several days prior to psychostimulant exposure, show inhibited expression3 or decreased acquisition of behavioral adaptations to drug5,11,12. The clustering of seemingly discrepant results based on experimental methodologies is interesting in light of our present findings. Both HDAC inhibitors and psychostimulants increase global levels of histone acetylation in NAc. Thus, when co-administered acutely, these drugs may have synergistic effects, leading to heightened transcriptional activation of psychostimulant-regulated target genes. In contrast, when a psychostimulant is given in the context of prolonged, HDAC inhibitor-induced hyperacetylation, homeostatic processes may direct AcH3 binding to the promoters of genes (e.g., G9a) responsible for inducing chromatin condensation and gene repression (e.g., via H3K9me2) in order to dampen already heightened transcriptional activation. Our present findings thus demonstrate clear cross talk among histone PTMs and suggest that decreased behavioral sensitivity to psychostimulants following prolonged HDAC inhibition might be mediated through decreased activity of HDAC1 at H3K9 KMT promoters and subsequent increases in H3K9me2 and gene repression.
• Simon-O'Brien E, Alaux-Cantin S, Warnault V, Buttolo R, Naassila M, Vilpoux C (July 2015). "The histone deacetylase inhibitor sodium butyrate decreases excessive ethanol intake in dependent animals". Addict Biol. 20 (4): 676–89. doi:10.1111/adb.12161. PMID 25041570. S2CID 28667144.Altogether, our results clearly demonstrated the efficacy of NaB in preventing excessive ethanol intake and relapse and support the hypothesis that HDACi may have a potential use in alcohol addiction treatment.
• Castino MR, Cornish JL, Clemens KJ (April 2015). "Inhibition of histone deacetylases facilitates extinction and attenuates reinstatement of nicotine self-administration in rats". PLOS ONE. 10 (4): e0124796. Bibcode:2015PLoSO..1024796C. doi:10.1371/journal.pone.0124796. PMC 4399837. PMID 25880762.treatment with NaB significantly attenuated nicotine and nicotine + cue reinstatement when administered immediately ... These results provide the first demonstration that HDAC inhibition facilitates the extinction of responding for an intravenously self-administered drug of abuse and further highlight the potential of HDAC inhibitors in the treatment of drug addiction.
- Kyzar EJ, Pandey SC (August 2015). "Molecular mechanisms of synaptic remodeling in alcoholism". Neurosci. Lett. 601: 11–19. doi:10.1016/j.neulet.2015.01.051. PMC 4506731. PMID 25623036.
Increased HDAC2 expression decreases the expression of genes important for the maintenance of dendritic spine density such as BDNF, Arc, and NPY, leading to increased anxiety and alcohol-seeking behavior. Decreasing HDAC2 reverses both the molecular and behavioral consequences of alcohol addiction, thus implicating this enzyme as a potential treatment target (Fig. 3). HDAC2 is also crucial for the induction and maintenance of structural synaptic plasticity in other neurological domains such as memory formation [115]. Taken together, these findings underscore the potential usefulness of HDAC inhibition in treating alcohol use disorders ... Given the ability of HDAC inhibitors to potently modulate the synaptic plasticity of learning and memory [118], these drugs hold potential as treatment for substance abuse-related disorders. ... Our lab and others have published extensively on the ability of HDAC inhibitors to reverse the gene expression deficits caused by multiple models of alcoholism and alcohol abuse, the results of which were discussed above [25,112,113]. This data supports further examination of histone modifying agents as potential therapeutic drugs in the treatment of alcohol addiction ... Future studies should continue to elucidate the specific epigenetic mechanisms underlying compulsive alcohol use and alcoholism, as this is likely to provide new molecular targets for clinical intervention.
- Kheirabadi GR, Ghavami M, Maracy MR, Salehi M, Sharbafchi MR (2016). "Effect of add-on valproate on craving in methamphetamine depended patients: A randomized trial". Advanced Biomedical Research. 5: 149. doi:10.4103/2277-9175.187404. PMC 5025910. PMID 27656618.
- "Gene Therapy For Addiction: Flooding Brain With 'Pleasure Chemical' Receptors Works On Cocaine, As On Alcohol".
- "Gene Transfer Therapy for Cocaine Addiction Passes Tests in Animals". National Institute on Drug Abuse. 14 January 2016.
- Murthy V, Gao Y, Geng L, LeBrasseur NK, White TA, Parks RJ, Brimijoin S (2014). "Physiologic and metabolic safety of butyrylcholinesterase gene therapy in mice". Vaccine. 32 (33): 4155–62. doi:10.1016/j.vaccine.2014.05.067. PMC 4077905. PMID 24892251.
- "Using Adeno-Associated Virus (AAV) Mediated Sustained Expression of an Anti-methamphetamine Antibody Fragment to Alter Methamphetamine Disposition in Mice" (PDF). Archived from the original (PDF) on 3 March 2018. Retrieved 25 June 2017.
- "ATTC – Addiction Science Made Easy". www.attcnetwork.org. Archived from the original on 27 September 2018. Retrieved 25 June 2017.
- Chen CC, Yin SJ (October 2008). "Alcohol abuse and related factors in Asia". International Review of Psychiatry. 20 (5): 425–433. doi:10.1080/09540260802344075. PMID 19012127. S2CID 24571763.
- Mak KK, Lai CM, Watanabe H, Kim DI, Bahar N, Ramos M, et al. (November 2014). "Epidemiology of internet behaviors and addiction among adolescents in six Asian countries". Cyberpsychology, Behavior and Social Networking. 17 (11): 720–728. doi:10.1089/cyber.2014.0139. PMID 25405785.
- Slade T, Johnston A, Teesson M, Whiteford H, Burgess P, Pirkis J, Saw S (May 2009). "The Mental Health of Australians 2: Substance Use Disorders in Australia" (PDF). Department of Health and Ageing, Canberra.
- Peacock A, Leung J, Larney S, Colledge S, Hickman M, Rehm J, et al. (October 2018). "Global statistics on alcohol, tobacco and illicit drug use: 2017 status report". Addiction. 113 (10): 1905–1926. doi:10.1111/add.14234. PMID 29749059. S2CID 13674349.
- Merikangas KR, McClair VL (June 2012). "Epidemiology of Substance Use Disorders". Hum. Genet. 131 (6): 779–89. doi:10.1007/s00439-012-1168-0. PMC 4408274. PMID 22543841.
- Manubay JM, Muchow C, Sullivan MA (March 2011). "Prescription drug abuse: epidemiology, regulatory issues, chronic pain management with narcotic analgesics". Primary Care. 38 (1): 71–90. doi:10.1016/j.pop.2010.11.006. PMC 3328297. PMID 21356422.
- "American Board of Medical Specialties recognizes the new subspecialty of addiction medicine" (PDF). American Board of Addiction Medicine. 14 March 2016. Archived from the original (PDF) on 21 March 2021. Retrieved 3 April 2016.
Sixteen percent of the non-institutionalized U.S. population age 12 and over – more than 40 million Americans – meets medical criteria for addiction involving nicotine, alcohol or other drugs. This is more than the number of Americans with cancer, diabetes or heart conditions. In 2014, 22.5 million people in the United States needed treatment for addiction involving alcohol or drugs other than nicotine, but only 11.6 percent received any form of inpatient, residential, or outpatient treatment. Of those who do receive treatment, few receive evidence-based care. (There is no information available on how many individuals receive treatment for addiction involving nicotine.)
Risky substance use and untreated addiction account for one-third of inpatient hospital costs and 20 percent of all deaths in the United States each year, and cause or contribute to more than 100 other conditions requiring medical care, as well as vehicular crashes, other fatal and non-fatal injuries, overdose deaths, suicides, homicides, domestic discord, the highest incarceration rate in the world and many other costly social consequences. The economic cost to society is greater than the cost of diabetes and all cancers combined. Despite these startling statistics on the prevalence and costs of addiction, few physicians have been trained to prevent or treat it. - Volkow N (31 March 2016). "A Major Step Forward for Addiction Medicine". National Institute on Drug Abuse. National Institutes of Health. Retrieved 3 April 2016.
Only about 10 percent of the 21 million Americans who meet the need for care for an alcohol or drug use disorder receive any form of treatment, and much of the treatment available does not meet standards for evidence-based care. There are many attitudinal and systemic reasons for this treatment gap, including stigma against treating people with addictions and institutional barriers to providing or funding addiction treatment. ... A major milestone was reached on March 14, 2016, when the American Board of Medical Specialties (ABMS) formally announced recognition of the field of Addiction Medicine as a medical subspecialty. ... In a statement issued to mark this milestone, ABAM President Robert J. Sokol summed up its significance: 'This landmark event, more than any other, recognizes addiction as a preventable and treatable disease, helping to shed the stigma that has long plagued it. It sends a strong message to the public that American medicine is committed to providing expert care for this disease and services designed to prevent the risky substance use that precedes it.'
- Gramlich J (26 October 2017). "Nearly half of Americans have a family member or close friend who's been addicted to drugs". Pew Research Center. Retrieved 14 January 2018.
- "We were addicted to their pill, but they were addicted to the money". The Washington Post. Retrieved 22 July 2019.
- Hasin, Deborah S.; Saha, Tulshi D.; Kerridge, Bradley T.; Goldstein, Risë B.; Chou, S. Patricia; Zhang, Haitao; Jung, Jeesun; Pickering, Roger P.; Ruan, W. June; Smith, Sharon M.; Huang, Boji; Grant, Bridget F. (1 December 2015). "Prevalence of Marijuana Use Disorders in the United States Between 2001-2002 and 2012-2013". JAMA Psychiatry. 72 (12): 1235. doi:10.1001/jamapsychiatry.2015.1858. ISSN 2168-622X. PMC 5037576. PMID 26502112.
- World Drug Report 2012 (PDF). United Nations Office on Drugs and Crime. United Nations. June 2012. ISBN 978-92-1-148267-6.
- Pacurucu-Castillo SF, Ordóñez-Mancheno JM, Hernández-Cruz A, Alarcón RD (April 2019). "World opioid and substance use epidemic: a Latin American perspective". Psychiatric Research and Clinical Practice. 1 (1): 32–8. doi:10.1176/appi.prcp.20180009. PMC 9175731. PMID 36101564.
- Crocq MA (December 2007). Thibaut F (ed.). "Historical and cultural aspects of man's relationship with addictive drugs". Dialogues in Clinical Neuroscience. Laboratoires Servier. 9 (4): 355–361. doi:10.31887/DCNS.2007.9.4/macrocq. OCLC 62869913. PMC 3202501. PMID 18286796. S2CID 12682928.
- Lemon R (2018). "Introduction: Addiction in (Early) Modernity". Addiction and Devotion in Early Modern England. Haney Foundation Series. Philadelphia: University of Pennsylvania Press. pp. 1–23. ISBN 978-0-8122-4996-5.
- Rosenthal R, Faris S (February 2019). "The etymology and early history of 'addiction'". Addiction Research & Theory. Taylor & Francis. 27 (5): 437–449. doi:10.1080/16066359.2018.1543412. ISSN 1476-7392. S2CID 150418396.
- Institute of Medicine (1996). Pathways of Addiction: Opportunities in Drug Abuse Research. Washington: National Academies Press.
- Bettinardi-Angres K, Angres DH (July 2010). Alexander M (ed.). "Understanding the Disease of Addiction". Journal of Nursing Regulation. Elsevier on behalf of the National Council of State Boards of Nursing. 1 (2): 31–37. doi:10.1016/S2155-8256(15)30348-3. ISSN 2155-8256. S2CID 143289528.
- Rau BL (September 2014). "The Oxford Handbook of Evidence-Based Management, Rousseau DM 2012. 432 pages, hardcover. New York, NY: Oxford University Press". Academy of Management Learning & Education. 13 (3): 485–487. doi:10.5465/amle.2013.0309. ISSN 1537-260X.
- Daley DC (December 2013). "Family and social aspects of substance use disorders and treatment". Journal of Food and Drug Analysis. 21 (4): S73–S76. doi:10.1016/j.jfda.2013.09.038. PMC 4158844. PMID 25214748.
- Saad M, de Medeiros R, Mosini AC (October 2017). "Are We Ready for a True Biopsychosocial-Spiritual Model? The Many Meanings of "Spiritual"". Medicines. 4 (4): 79. doi:10.3390/medicines4040079. PMC 5750603. PMID 29088101.
- Farmer P, Kleinman A, Kim J, Basilico M, eds. (31 December 2019). Reimagining Global Health: An Introduction. University of California Press. doi:10.1525/9780520954632. ISBN 978-0-520-95463-2. S2CID 168489288.
- Weakland JH (October 1961). "The Essence of Anthropological Education". American Anthropologist. 63 (5): 1094–1097. doi:10.1525/aa.1961.63.5.02a00130. ISSN 0002-7294.
- Bourgois P (23 December 2002). In Search of Respect: Selling Crack in El Barrio (2 ed.). Cambridge University Press. doi:10.1017/cbo9780511808562. ISBN 978-0-521-01711-4.
- Singer M (October 2012). "Anthropology and addiction: an historical review". Addiction. 107 (10): 1747–1755. doi:10.1111/j.1360-0443.2012.03879.x. PMID 22962955.
- Heath DB (September 1958). "Drinking patterns of the Bolivian Camba". Quarterly Journal of Studies on Alcohol. 19 (3): 491–508. doi:10.15288/qjsa.1958.19.491. PMID 13579177.
- Heath DB (January 1995). "Changes in Drinking Patterns in Bolivian Cultures: A Cautionary Tale About Historical Approaches". Addiction Research. 2 (3): 307–318. doi:10.3109/16066359509005215. ISSN 1058-6989.
- Burraway J (October 2020). Stein F, Diemberger H, Stasch R, Robbins J, Sanchez A, Lazar S, Candea M (eds.). "Addiction". Cambridge Encyclopedia of Anthropology. doi:10.29164/20addiction. S2CID 241689890.
- Preble E, Casey JJ (January 1969). "Taking Care of Business—The Heroin User's Life on the Street". International Journal of the Addictions. 4 (1): 1–24. doi:10.3109/10826086909061998. ISSN 0020-773X.
- Golub A, Johnson BD, Dunlap E (May 2005). "Subcultural evolution and illicit drug use". Addiction Research & Theory. 13 (3): 217–229. doi:10.1080/16066350500053497. PMC 3690817. PMID 23805068.
- Malenka RC, Nestler EJ, Hyman SE (2009). "Chapter 1: Basic Principles of Neuropharmacology". In Sydor A, Brown RY (eds.). Molecular Neuropharmacology: A Foundation for Clinical Neuroscience (2nd ed.). New York: McGraw-Hill Medical. p. 4. ISBN 978-0-07-148127-4.
Drug abuse and addiction exact an astoundingly high financial and human toll on society through direct adverse effects, such as lung cancer and hepatic cirrhosis, and indirect adverse effects –for example, accidents and AIDS – on health and productivity.
- "Economic consequences of drug abuse" (PDF). International Narcotics Control Board Report: 2013 (PDF). United Nations – International Narcotics Control Board. 2013. ISBN 978-92-1-148274-4. Retrieved 28 September 2018.
- "Overdose Death Rates". National Institute on Drug Abuse. 9 August 2018. Retrieved 17 September 2018.
- "Overdose Deaths Accelerating During Covid-19". Centers For Disease Control Prevention. 18 December 2020. Retrieved 10 February 2021.
- jetcopter
- Online Etymology Dictionary : alcohol
Further reading
- Szalavitz M (2016). Unbroken Brain. St. Martin's Press. ISBN 978-1-250-05582-8.
External links
- "The Science of Addiction: Genetics and the Brain". learn.genetics.utah.edu. Learn.Genetics – University of Utah.
- Why do our brains get addicted? – a TEDMED 2014 talk by Nora Volkow, the director of the National Institute on Drug Abuse at NIH.
- Gordon HW (April 2016). "Laterality of Brain Activation for Risk Factors of Addiction". Current Drug Abuse Reviews. 9 (1): 1–18. doi:10.2174/1874473709666151217121309. PMC 4811731. PMID 26674074.
Kyoto Encyclopedia of Genes and Genomes (KEGG) signal transduction pathways: