Local anesthetic
A local anesthetic (LA) is a medication that causes absence of pain sensation. In the context of surgery, a local anesthetic creates an absence of pain in a specific location of the body without a loss of consciousness, as opposed to a general anesthetic. When it is used on specific nerve pathways (local anesthetic nerve block), paralysis (loss of muscle power) also can be achieved.
Examples
Short Duration & Low Potency
Procaine
Chloroprocaine
Medium Duration & Potency
Prilocaine
High Duration & Potency
Tetracaine
Bupivacaine
Cinchocaine
Ropivacaine
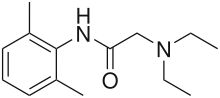
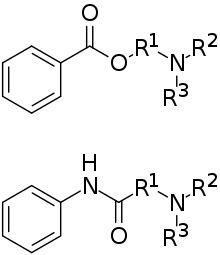
Clinical LAs belong to one of two classes: aminoamide and aminoester local anesthetics. Synthetic LAs are structurally related to cocaine. They differ from cocaine mainly in that they have a very low abuse potential and do not produce hypertension or (with few exceptions) vasoconstriction.
They are used in various techniques of local anesthesia such as:
- Topical anesthesia (surface)
- Topical administration of cream, gel, ointment, liquid, or spray of anaesthetic dissolved in DMSO or other solvents/carriers for deeper absorption
- Infiltration
- Brachial plexus block
- Epidural (extradural) block
- Spinal anesthesia (subarachnoid block)
- Iontophoresis
The suffix "-caine" at the ends of these medication names was extracted from the word "cocaine", because cocaine was formerly used as a local anesthetic.
Medical uses
Acute pain
Acute pain may occur due to trauma, surgery, infection, disruption of blood circulation, or many other conditions in which tissue injury occurs. In a medical setting, pain alleviation is desired when its warning function is no longer needed. Besides improving patient comfort, pain therapy can also reduce harmful physiological consequences of untreated pain.
Acute pain can often be managed using analgesics. However, conduction anesthesia may be preferable because of superior pain control and fewer side effects. For purposes of pain therapy, LA drugs are often given by repeated injection or continuous infusion through a catheter. LA drugs are also often combined with other agents such as opioids for synergistic analgesic action.[1] Low doses of LA drugs can be sufficient so that muscle weakness does not occur and patients may be mobilized.
Some typical uses of conduction anesthesia for acute pain are:
- Labor pain (epidural anesthesia, pudendal nerve blocks)
- Postoperative pain (peripheral nerve blocks, epidural anesthesia)
- Trauma (peripheral nerve blocks, intravenous regional anesthesia, epidural anesthesia)
Chronic pain
Chronic pain is a complex and often serious condition that requires diagnosis and treatment by an expert in pain medicine. LAs can be applied repeatedly or continuously for prolonged periods to relieve chronic pain, usually in combination with medication such as opioids, NSAIDs, and anticonvulsants. Though it can be easily performed, repeated local anaesthetic blocks in chronic pain conditions are not recommended as there is no evidence of long-term benefits.[2]
Surgery
Virtually every part of the body can be anesthetized using conduction anesthesia. However, only a limited number of techniques are in common clinical use. Sometimes, conduction anesthesia is combined with general anesthesia or sedation for the patient's comfort and ease of surgery. However, many anaesthetists, surgeons, patients and nurses believe that it is safer to perform major surgeries under local anesthesia than general anesthesia.[3] Typical operations performed under conduction anesthesia include:
- Dentistry (surface anesthesia, infiltration anesthesia or intraligamentary anesthesia during restorative operations such as fillings, crowns, and root canals,[4] or extractions, and regional nerve blocks during extractions and surgeries)
- Podiatry (cutaneous, nail avulsions, matricectomy, bunionectomy, hammertoe repair [4] and various other podiatric procedures)
- Eye surgery (surface anesthesia with topical anesthetics or retrobulbar block during cataract removal or other ophthalmic procedures[4])
- ENT operations, head and neck surgery (infiltration anesthesia, field blocks, or peripheral nerve blocks, plexus anesthesia)
- Shoulder and arm surgery (plexus anesthesia or intravenous regional anesthesia)[5]
- Heart and lung surgery (epidural anesthesia combined with general anesthesia)
- Abdominal surgery (epidural anesthesia/spinal anesthesia, often combined with general anesthesia during inguinal hernia repair or other abdominal surgery [4])
- Gynecological, obstetrical, and urological operations (spinal/epidural anesthesia)
- Bone and joint surgery of the pelvis, hip, and leg (spinal/epidural anesthesia, peripheral nerve blocks, or intravenous regional anesthesia)
- Surgery of skin and peripheral blood vessels (topical anesthesia, field blocks, peripheral nerve blocks, or spinal/epidural anesthesia)
Diagnostic tests
Diagnostic tests such as bone marrow aspiration, lumbar puncture (spinal tap) and aspiration of cysts or other structures are made to be less painful upon administration of local anesthetic before insertion of larger needles.[4]
Other uses
Local anesthesia is also used during insertion of IV devices, such as pacemakers and implantable defibrillators, ports used for giving chemotherapy medications and hemodialysis access catheters.[4]
Topical anesthesia, in the form of lidocaine/prilocaine (EMLA) is most commonly used to enable relatively painless venipuncture (blood collection) and placement of intravenous cannulae. It may also be suitable for other kinds of punctures such as ascites drainage and amniocentesis.
Surface anesthesia also facilitates some endoscopic procedures such as bronchoscopy (visualization of the lower airways) or cystoscopy (visualization of the inner surface of the bladder)
Side effects
Localized side effects
Edema of tongue, pharynx and larynx may develop as a side effect of local anaesthesia. This could be caused by a variety of reasons including trauma during injection, infection, an allergic reaction, haematoma or injection of irritating solutions such as cold-sterilisation solutions. Usually there is tissue swelling at the point of injection. This is due to puncturing of the vein which allows the blood to flow into loose tissues in the surrounding area. Blanching of the tissues in the area where the local anaesthetic is deposited is also common. This gives the area a white appearance as the blood flow is prevented due to vasoconstriction of arteries in the area. The vasoconstriction stimulus gradually wears off and subsequently the tissue returns to normal in less than 2 hours.[6]
The side effects of inferior alveolar nerve block include feeling tense, clenching of the fists and moaning.[7]
The duration of soft tissue anaesthesia is longer than pulpal anaesthesia and is often associated with difficulty eating, drinking and speaking.[7]
Risks
The risk of temporary or permanent nerve damage varies between different locations and types of nerve blocks.[8]
There is risk of accidental damage to local blood vessels during injection of the local anaesthetic solution. This is referred to as Haematoma and could result in pain, trismus, swelling and/or discolouration of the region. The density of tissues surrounding the injured vessels is an important factor for Haematoma. There is greatest chance of this occurring in a posterior superior alveolar nerve block or in a pterygomandibular block.
Giving local anaesthesia to patients with liver disease can have significant consequences. Thorough evaluation of the disease should be carried out to assess potential risk to the patient as in significant liver dysfunction, the half-life of amide local anaesthetic agents may be drastically increased thus increasing the risk of overdose.
Local anaesthetics and vasoconstrictors may be administered to pregnant patients however it is very important to be extra cautious when giving a pregnant patient any type of drug. Lidocaine can be safely used but bupivacaine and mepivacaine should be avoided. Consultation with the obstetrician is vital before administrating any type of local anaesthetic to a pregnant patient.[6]
Recovery
Permanent nerve damage after a peripheral nerve block is rare. Symptoms are likely to resolve within a few weeks. The vast majority of those affected (92%–97%) recover within four to six weeks; 99% of these people have recovered within a year. An estimated one in 5,000 to 30,000 nerve blocks results in some degree of permanent persistent nerve damage.[8]
Symptoms may continue to improve for up to 18 months following injury.
Potential side effects
General systemic adverse effects are due to the pharmacological effects of the anesthetic agents used. The conduction of electric impulses follows a similar mechanism in peripheral nerves, the central nervous system, and the heart. The effects of local anesthetics are, therefore, not specific for the signal conduction in peripheral nerves. Side effects on the central nervous system and the heart may be severe and potentially fatal. However, toxicity usually occurs only at plasma levels which are rarely reached if proper anesthetic techniques are adhered to. High plasma levels might arise, for example, when doses intended for epidural or intrasupport tissue administration are accidentally delivered as intravascular injection.
Emotional reactions
When patients are emotionally affected in the form of nervousness or fear, it can lead to vasovagal collapse. This is the anticipation of pain during administration that activates the parasympathetic nervous system while inhibiting the orthosympathetic nervous system.[9] What results is a dilation of arteries in muscles which can lead to a reduction in circulating blood volume inducing a temporary shortness of blood flow to the brain. Notable symptoms include restlessness, visibly looking pale, perspiration and possible loss of consciousness. In severe cases, clonic cramps resembling an epileptic insult may occur.[9]
On the other hand, fear of administration can also result in accelerated, shallow breathing, or hyperventilation. The patient may feel a tingling sensation in hands and feet or a sense of light-headedness and increased chest pressure.
Hence, it is crucial for the medical professional administrating the local anaesthesia, especially in the form of an injection, to ensure that the patient is in a comfortable setting and has any potential fears alleviated in order to avoid these possible complications.
Central nervous system
Depending on local tissue concentrations of local anesthetics, excitatory or depressant effects on the central nervous system may occur.
Initial symptoms of systemic toxicity include ringing in the ears (tinnitus), a metallic taste in the mouth, tingling or numbness of the mouth, dizziness and/or disorientation.
At higher concentrations, a relatively selective depression of inhibitory neurons results in cerebral excitation, which may lead to more advanced symptoms include motor twitching in the periphery followed by grand mal seizures. It is reported that seizures are more likely to occur when bupivacaine is used, particularly in combination with chloroprocaine.[10]
A profound depression of brain functions may occur at even higher concentrations which may lead to coma, respiratory arrest, and death.[11] Such tissue concentrations may be due to very high plasma levels after intravenous injection of a large dose.
Another possibility is direct exposure of the central nervous system through the cerebrospinal fluid, i.e., overdose in spinal anesthesia or accidental injection into the subarachnoid space in epidural anesthesia.
Cardiovascular system
Cardiac toxicity can result from improper injection of agent into a vessel. Even with proper administration, it is inevitable for some diffusion of agent into the body from the site of application due to unforeseeable anatomical idiosyncrasies of the patient.[10] This may affect the nervous system or cause the agent to enter into general circulation. However, infections are very seldom transmitted.
Cardiac toxicity associated with overdose of intravascular injection of local anesthetic is characterized by hypotension, atrioventricular conduction delay, idioventricular rhythms, and eventual cardiovascular collapse. Although all local anesthetics potentially shorten the myocardial refractory period, bupivacaine blocks the cardiac sodium channels, thereby making it most likely to precipitate malignant arrhythmias. Even levobupivacaine and ropivacaine (single-enantiomer derivatives), developed to ameliorate cardiovascular side effects, still harbor the potential to disrupt cardiac function.[12] Toxicity from anesthetic combinations is additive.[10]
Endocrine
Endocrine and metabolic systems only have slightly adverse effects with most cases being without clinical repercussions.[10]
Immunologic allergy
Adverse reactions to local anesthetics (especially the esters) are not uncommon, but legitimate allergies are very rare. Allergic reactions to the esters is usually due to a sensitivity to their metabolite, para-aminobenzoic acid, and does not result in cross-allergy to amides.[13][14] Therefore, amides can be used as alternatives in those patients. Nonallergic reactions may resemble allergy in their manifestations. In some cases, skin tests and provocative challenge may be necessary to establish a diagnosis of allergy. Also cases of allergy to paraben derivatives occur, which are often added as preservatives to local anesthetic solutions.
Methemoglobinemia
Methemoglobinemia is a process where iron in hemoglobin is altered, reducing its oxygen-carrying capability, which produces cyanosis and symptoms of hypoxia. Exposure to aniline group chemicals such as benzocaine, lidocaine, and prilocaine can produce this effect, especially benzocaine.[13][14] The systemic toxicity of prilocaine is comparatively low, but its metabolite, o-toluidine, is known to cause methemoglobinemia.
Second-generation effects
Application of local anesthetics during oocyte removal during in vitro fertilisation has been up to debate. Pharmacological concentrations of anesthetic agents have been found in follicular fluid.[10] Clinical trials have not concluded any effects on pregnant women. However, there is some concern with the behavioral effects of lidocaine on offspring in rats.[10]
During pregnancy, it is not common for local anesthetics to have any adverse effect on the fetus. Despite this, risks of toxicity may be higher in pregnancy due to an increase in unbound fraction of local anesthetic and physiological changes increase the transfer of local anesthetic into the central nervous system.[10] Hence, it is recommended that pregnant women use a lower dose of local anesthetic to reduce any potential complications.
Treatment of overdose: "Lipid rescue"
This method of toxicity treatment was invented by Dr. Guy Weinberg in 1998, and was not widely used until after the first published successful rescue in 2006. Evidence indicates Intralipid, a commonly available intravenous lipid emulsion, can be effective in treating severe cardiotoxicity secondary to local anesthetic overdose, including human case reports of successful use in this way (lipid rescue).[15][16][17][18][19] However, the evidence at this point is still limited.[20]
Though most reports to date have used Intralipid, a commonly available intravenous lipid emulsion, other emulsions, such as Liposyn and Medialipid, have also been shown effective.
Ample supporting animal evidence[15][16] and human case reports show successful use in this way.[18][19] In the UK, efforts have been made to publicise this use more widely[17] and lipid rescue has now been officially promoted as a treatment by the Association of Anaesthetists of Great Britain and Ireland.[21] One published case has been reported of successful treatment of refractory cardiac arrest in bupropion and lamotrigine overdose using lipid emulsion.[22]
The design of a 'homemade' lipid rescue kit has been described.[23]
Although lipid rescue mechanism of action is not completely understood, the added lipid in the blood stream may act as a sink, allowing for the removal of lipophilic toxins from affected tissues. This theory is compatible with two studies on lipid rescue for clomipramine toxicity in rabbits[24][25] and with a clinical report on the use of lipid rescue in veterinary medicine to treat a puppy with moxidectin toxicosis.[26]
Mechanism of action
All LAs are membrane-stabilizing drugs; they reversibly decrease the rate of depolarization and repolarization of excitable membranes (like nociceptors). Though many other drugs also have membrane-stabilizing properties, not all are used as LAs (propranolol, for example, though it has LA properties). LA drugs act mainly by inhibiting sodium influx through sodium-specific ion channels in the neuronal cell membrane, in particular the so-called voltage-gated sodium channels. When the influx of sodium is interrupted, an action potential cannot arise and signal conduction is inhibited. The receptor site is thought to be located at the cytoplasmic (inner) portion of the sodium channel. Local anesthetic drugs bind more readily to sodium channels in an activated state, thus onset of neuronal blockade is faster in rapidly firing neurons. This is referred to as state-dependent blockade.
LAs are weak bases and are usually formulated as the hydrochloride salt to render them water-soluble. At a pH equal to the protonated base's pKa, the protonated (ionized) and unprotonated (unionized) forms of the molecule exist in equimolar amounts, but only the unprotonated base diffuses readily across cell membranes. Once inside the cell, the local anesthetic will be in equilibrium, with the formation of the protonated (ionized) form, which does not readily pass back out of the cell. This is referred to as "ion-trapping". In the protonated form, the molecule binds to the LA binding site on the inside of the ion channel near the cytoplasmic end. Most LAs work on the internal surface of the membrane - the drug has to penetrate the cell membrane, which is achieved best in the nonionised form. This is exemplified by the permanently ionised LA RAC 421-II which cannot diffuse across the cell membrane but, if injected into the cytosol of a nerve fibre, can induce NaKATPase blockage and anaesthetic effects.
Acidosis such as caused by inflammation at a wound partly reduces the action of LAs. This is partly because most of the anesthetic is ionized and therefore unable to cross the cell membrane to reach its cytoplasmic-facing site of action on the sodium channel.
All nerve fibers are sensitive to LAs, but due to a combination of diameter and myelination, fibers have different sensitivities to LA blockade, termed differential blockade. Type B fibers (sympathetic tone) are the most sensitive followed by type C (pain), type A delta (temperature), type A gamma (proprioception), type A beta (sensory touch and pressure), and type A alpha (motor). Although type B fibers are thicker than type C fibers, they are myelinated, thus are blocked before the unmyelinated, thin C fiber.[27]
Techniques
Local anesthetics can block almost every nerve between the peripheral nerve endings and the central nervous system. The most peripheral technique is topical anesthesia to the skin or other body surface. Small and large peripheral nerves can be anesthetized individually (peripheral nerve block) or in anatomic nerve bundles (plexus anesthesia). Spinal anesthesia and epidural anesthesia merge into the central nervous system.
Injection of LAs is often painful. A number of methods can be used to decrease this pain, including buffering of the solution with bicarbonate and warming.[28]
Clinical techniques include:
- Surface anesthesia is the application of an LA spray, solution, or cream to the skin or a mucous membrane; the effect is short lasting and is limited to the area of contact.
- Infiltration anesthesia is infiltration of LA into the tissue to be anesthetized; surface and infiltration anesthesia are collectively topical anesthesia
- Field block is subcutaneous injection of an LA in an area bordering on the field to be anesthetized.
- Peripheral nerve block is injection of LA in the vicinity of a peripheral nerve to anesthetize that nerve's area of innervation.
- Plexus anesthesia is injection of LA in the vicinity of a nerve plexus, often inside a tissue compartment that limits the diffusion of the drug away from the intended site of action. The anesthetic effect extends to the innervation areas of several or all nerves stemming from the plexus.
- Epidural anesthesia is an LA injected into the epidural space, where it acts primarily on the spinal nerve roots; depending on the site of injection and the volume injected, the anesthetized area varies from limited areas of the abdomen or chest to large regions of the body.
- Spinal anesthesia is an LA injected into the cerebrospinal fluid, usually at the lumbar spine (in the lower back), where it acts on spinal nerve roots and part of the spinal cord; the resulting anesthesia usually extends from the legs to the abdomen or chest.
- Intravenous regional anesthesia (Bier's block) is when blood circulation of a limb is interrupted using a tourniquet (a device similar to a blood-pressure cuff), then a large volume of LA is injected into a peripheral vein. The drug fills the limb's venous system and diffuses into tissues, where peripheral nerves and nerve endings are anesthetized. The anesthetic effect is limited to the area that is excluded from blood circulation and resolves quickly once circulation is restored.
- Local anesthesia of body cavities includes intrapleural anesthesia and intra-articular anesthesia.
- Transincision (or transwound) catheter anesthesia uses a multilumen catheter inserted through an incision or wound and aligned across it on the inside as the incision or wound is closed, providing continuous administration of local anesthetic along the incision or wounds[29]
Dental-specific techniques include:
Vazirani-Alkinosi Technique
The Vazirani-alkinosi technique is also known as the closed-mouth mandibular nerve block. It is mostly used in patients who have limited opening of the mandible or in those that have trismus; spasm of the muscles of mastication. The nerves which are anesthetised in this technique are the inferior alveolar, incisive, mental, lingual and mylohyoid nerves.
Dental needles are available in 2 lengths; short and long. As Vazirani-akinosi is a local anaesthetic technique which requires penetration of a significant thickness of soft tissues, a long needle is used. The needle is inserted into the soft tissue which covers the medial border of the mandibular ramus, in region of the inferior alveolar, lingual and mylohyoid nerves. The positioning of the bevel of the needle is very important as it must be positioned away from the bone of the mandibular ramus and instead towards the midline.[30]
Intraligamentary Infiltration
Intraligamentary infiltration, also known as periodontal ligament injection or intraligamentary injection (ILIs), is known as "the most universal of the supplemental injections". ILIs are usually administered when inferior alveolar nerve block techniques are inadequate or ineffective.[31] ILIs are purposed for:
1. Single-tooth anesthesia
2. Low anesthetic dose
3. Contraindication for systemic anesthesia
4. Presence of systemic health problems[32]
ILI utilization is expected to increase because dental patients prefer fewer soft tissue anesthesia and dentists aim to reduce administration of traditional inferior alveolar nerve block (INAB) for routine restorative procedures.[33]
Injection methodology: The periodontal ligament space provides an accessible route to the cancellous alveolar bone, and the anesthetic reaches the pulpal nerve via natural perforation of intraoral bone tissue.[34][35]
Advantages of ILI over INAB: rapid onset (within 30 seconds), small dosage required (0.2-1.0 mL), limited area of numbness,[36][37] lower intrinsic risks such as neuropathy, hematoma, trismus/jaw sprain[38][39] and self-inflicted periodontal tissue injury,[40][41] as well as decreased cardiovascular disturbances.[42] Its usage as a secondary or supplementary anesthesia on the mandible has reported a high success rate of above 90%.[43][44]
Disadvantages: Risk of temporary periodontal tissue damage, likelihood of bacteriemia and endocarditis for at-risk populations,[45] appropriate pressure and correct needle placement are imperative for anesthetic success, short duration of pulpal anesthesia limits the use of ILIs for several restorative procedures that require longer duration,[45] postoperative discomfort, and injury on unerupted teeth such as enamel hypoplasia and defects.
Technique description:
- All plaque and calculus to be eradicated, optimally before the operative visit to assist gingival tissue healing.
- Before injection, disinfect gingival sulcus with 0.2% chlorhexidine solution.[46]
- Administration of soft tissue anesthesia is recommended prior to ILI administration. This helps to enhance patient comfort.
- Needle gauges of sizes 27-gauge short or 30-gauge ultra-short needle are usually utilized.[47]
- The needle is inserted along the long axis, at a 30-degree angle, of the mesial or distal root for single rooted teeth and on the mesial and distal roots of multi-rooted teeth. Bevel orientation toward the root provides easier advancement of the needle apically.[48]
- When the needle reaches between the root and crestal bone, significant resistance is experience.
- Anesthetic deposition is recommended at 0.2 mL, per root or site, over minimally 20 seconds.
- For its success, the anesthetic must be administered under pressure. It must not leak out of the sulcus into the mouth.
- Withdraw needle for minimally 10–15 seconds to permit complete deposition of solution. This can be slower than other injections as there is pressure build-up from the anesthetic administration.
- Blanching of the tissue is observed and may be more evident when vasoconstrictors are used. It is caused by a temporary obstruction of blood flow to the tissue.[48]
Syringes:
- Standard syringes can be used.
- The intraligamentary syringe offers mechanical advantage by using a trigger-grasp or click apparatus to employ a gear or lever that improves control and results in increased force to push the anesthetic cartridge's rubber stopper forward for medication deposition with greater ease.
- C-CLADs (computer controlled local anesthetic delivery devices) can be used. Its usage of computer microprocessors allows for control of fluid dynamics and anesthetic deposition. This minimizes subjective flow rates and variability in pressure. This thereby results in enhanced hydrodynamic diffusion of solution into bone or the target area of deposition,[49][50] thus permitting larger amounts of anesthetic solution to be delivered during ILIs without increased tissue damage.[51][52][53]
Things to note:
- ILIs are not recommended for patients with active periodontal inflammation.
- ILIs should not be administered at tooth sites with 5mm or more of periodontal attachment loss.
Gow-Gates Technique
Gow-Gates technique is used to provide anesthetics to the mandible of the patient's mouth. With the aid of extra and intraoral landmarks, the needle is injected into the intraoral latero-anterior surface of the condyle, steering clear below the insertion of the lateral pterygoid muscle.[54] The extraoral landmarks used for this technique are the lower border of the ear tragus, corners of the mouth and the angulation of the tragus on the side of the face.[54]
Biophysical forces (pulsation of the maxillary artery, muscular function of jaw movement) and gravity will aid with the diffusion of anesthetic to fill the whole pterygomandibular space. All three oral sensory parts of the mandibular branch of the trigeminal nerve and other sensory nerves in the region will come in contact with the anesthetic and this reduces the need to anesthetise supplementary innervation.[54]
In comparison to other regional block methods of anestheising the lower jaw, the Gow-Gates technique has a higher success rate in fully anesthetising the lower jaw. One study found that out of 1,200 patients receiving injections through the Gow-Gate technique, only 2 of them did not obtain complete anesthesia.[54]
Types

Local anesthetic solutions for injection typically consist of:[55]
- The local anesthetic agent itself
- A vehicle, which is usually water-based or just sterile water
- Vasoconstrictor possibly (see below)
- Reducing agent (antioxidant), e.g. if epinephrine is used, then sodium metabisulfite is used as a reducing agent
- Preservative, e.g. methylparaben
- Buffer
Esters are prone to producing allergic reactions, which may necessitate the use of an amide. The names of each locally clinical anesthetic have the suffix "-caine". Most ester LAs are metabolized by pseudocholinesterase, while amide LAs are metabolized in the liver. This can be a factor in choosing an agent in patients with liver failure,[56] although since cholinesterases are produced in the liver, physiologically (e.g. very young or very old individual) or pathologically (e.g. cirrhosis) impaired hepatic metabolism is also a consideration when using esters.
Sometimes, LAs are combined, e.g.:
- Lidocaine/prilocaine (EMLA, eutectic mixture of local anesthetic)
- Lidocaine/tetracaine (Rapydan)
- TAC
LA solutions for injection are sometimes mixed with vasoconstrictors (combination drug) to increase the duration of local anesthesia by constricting the blood vessels, thereby safely concentrating the anesthetic agent for an extended duration, as well as reducing hemorrhage.[57] Because the vasoconstrictor temporarily reduces the rate at which the systemic circulation removes the local anesthetic from the area of the injection, the maximum doses of LAs when combined with a vasoconstrictor is higher compared to the same LA without any vasoconstrictor. Occasionally, cocaine is administered for this purpose. Examples include:
- Prilocaine hydrochloride and epinephrine (trade name Citanest Forte)
- Lidocaine, bupivacaine, and epinephrine (recommended final concentrations of 0.5, 0.25, and 0.5%, respectively)
- Iontocaine, consisting of lidocaine and epinephrine
- Septocaine (trade name Septodont), a combination of articaine and epinephrine
One combination product of this type is used topically for surface anaesthesia, TAC (5-12% tetracaine,1/2000 (0.05%, 500 ppm, 1⁄2 per mille) adrenaline, 4 or 10% cocaine).
Using LA with vasoconstrictor is safe in regions supplied by end arteries. The commonly held belief that LA with vasoconstrictor can cause necrosis in extremities such as the nose, ears, fingers, and toes (due to constriction of end arteries), is invalidated, since no case of necrosis has been reported since the introduction of commercial lidocaine with epinephrine in 1948.[58]
Ester group
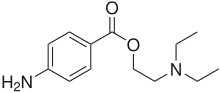
- Benzocaine
- Chloroprocaine
- Cocaine
- Cyclomethycaine
- Dimethocaine (Larocaine)
- Piperocaine
- Propoxycaine
- Procaine (Novocaine)
- Proparacaine
- Tetracaine (Amethocaine)
Amide group
- Articaine
- Bupivacaine
- Cinchocaine (Dibucaine)
- Etidocaine
- Levobupivacaine
- Lidocaine (Lignocaine)
- Mepivacaine
- Prilocaine
- Ropivacaine
- Trimecaine
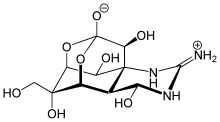
Naturally derived
- Saxitoxin
- Neosaxitoxin
- Tetrodotoxin
- Menthol
- Eugenol
- Cocaine
- Spilanthol
Most naturally occurring local anesthetics with the exceptions of menthol, eugenol and cocaine are neurotoxins, and have the suffix -toxin in their names. Cocaine binds the intracellular side of the channels while saxitoxin, neosaxitoxin and tetrodotoxin bind to the extracellular side of sodium channels.
History
In Peru, the ancient Incas are believed to have used the leaves of the coca plant as a local anaesthetic in addition to its stimulant properties.[59] It was also used for slave payment and is thought to play a role in the subsequent destruction of Incas culture when Spaniards realized the effects of chewing the coca leaves and took advantage of it.[59] Cocaine was first used as a local anesthetic in 1884. The search for a less toxic and less addictive substitute led to the development of the aminoester local anesthetics stovaine in 1903 and procaine in 1904. Since then, several synthetic local anesthetic drugs have been developed and put into clinical use, notably lidocaine in 1943, bupivacaine in 1957, and prilocaine in 1959.
The invention of clinical use of local anaesthesia is credited to the Vienna School which included Sigmund Freud (1856-1939), Carl Koller (1857-1944) and Leopold Konigstein (1850-1942). They introduced local anaesthesia, using cocaine, through 'self-experimation' on their oral mucosa before introducing it to animal or human experimentation. The Vienna school first started using cocaine as local anaesthesia in ophthalmology and it was later incorporated into ophthalmologic practice. Dr. Halsted and Dr. Hall, in the United States in 1885 described an intraoral anaesthetic technique of blocking the inferior alveolar nerve and the antero-superior dental nerve using 4% cocaine.{[60]
Shortly after the first use of cocaine for topical anesthesia, blocks on peripheral nerves were described. Brachial plexus anesthesia by percutaneous injection through axillary and supraclavicular approaches was developed in the early 20th century. The search for the most effective and least traumatic approach for plexus anesthesia and peripheral nerve blocks continues to this day. In recent decades, continuous regional anesthesia using catheters and automatic pumps has evolved as a method of pain therapy.
Intravenous regional anesthesia was first described by August Bier in 1908. This technique is still in use and is remarkably safe when drugs of low systemic toxicity such as prilocaine are used.
Spinal anesthesia was first used in 1885, but not introduced into clinical practice until 1899, when August Bier subjected himself to a clinical experiment in which he observed the anesthetic effect, but also the typical side effect of postpunctural headache. Within a few years, spinal anesthesia became widely used for surgical anesthesia and was accepted as a safe and effective technique. Although atraumatic (noncutting-tip) cannulae and modern drugs are used today, the technique has otherwise changed very little over many decades.
Epidural anesthesia by a caudal approach had been known in the early 20th century, but a well-defined technique using lumbar injection was not developed until 1921, when Fidel Pagés published his article "Anestesia Metamérica". This technique was popularized in the 1930s and 1940s by Achile Mario Dogliotti. With the advent of thin, flexible catheters, continuous infusion and repeated injections have become possible, making epidural anesthesia still a highly successful technique. Besides its many uses for surgery, epidural anesthesia is particularly popular in obstetrics for the treatment of labor pain.
See also
- Amylocaine
- Anesthetic
- General anesthetic
- List of cocaine analogues
- List of local anesthetics
References
- Ryan, T (2019). "Tramadol as an adjunct to intra‐articular local anaesthetic infiltration in knee arthroscopy: a systematic review and meta‐analysis". ANZ Journal of Surgery. 89 (7–8): 827–832. doi:10.1111/ans.14920. PMID 30684306. S2CID 59275648.
- "Current world literature. Drugs in anaesthesia". Current Opinion in Anesthesiology. 16 (4): 429–36. August 2003. doi:10.1097/00001503-200308000-00010. PMID 17021493.
- Bodenham AR, Howell SJ (December 2009). "General anaesthesia vs local anaesthesia: an ongoing story". British Journal of Anaesthesia. 103 (6): 785–9. doi:10.1093/bja/aep310. PMID 19918020.
- Torpy JM, Lynm C, Golub RM (September 2011). "JAMA patient page. Local anesthesia". JAMA. 306 (12): 1395. doi:10.1001/jama.306.12.1395. PMID 21954483.
- Brown AR, Weiss R, Greenberg C, Flatow EL, Bigliani LU (1993). "Interscalene block for shoulder arthroscopy: comparison with general anesthesia". Arthroscopy. 9 (3): 295–300. doi:10.1016/S0749-8063(05)80425-6. PMID 8323615.
- P., Chitre, A. (2016). Manual of local anaesthesia in dentistry. [Place of publication not identified]: Jaypee Brothers Medical P. ISBN 978-9352501984. OCLC 930829770.
- Al., Reader (12 September 2014). Successful local anesthesia for restorative dentistry and endodontics. Nusstein, John., Drum, Melissa. Chicago. ISBN 9780867156157. OCLC 892911544.
- "Nerve damage associated with peripheral nerve block" (PDF). Risks Associated with Your Anaesthetic. Section 12. January 2006. Archived from the original (PDF) on 2007-10-09. Retrieved 2007-10-10.
- Baart JA, Brand HS (2017-06-07). Local Anaesthesia in Dentistry. Springer. ISBN 9783319437057.
- Aronson, Jeffrey K. (2008-10-07). Meyler's Side Effects of Drugs Used in Anesthesia. Elsevier. ISBN 9780444532701.
- Mulroy MF (2002). "Systemic toxicity and cardiotoxicity from local anesthetics: incidence and preventive measures". Regional Anesthesia and Pain Medicine. 27 (6): 556–61. doi:10.1053/rapm.2002.37127. PMID 12430104. S2CID 36915462.
- Stiles P, Prielipp RC (Spring 2009). "Intralipid Treatment Of Bupicavaine Toxicity". Anesthesia Patient Safety Foundation. 24 (1). Retrieved 12 June 2013.
- Dolan R (2003-10-17). Facial plastic, reconstructive, and trauma surgery. Marcel Dekker. ISBN 978-0-8247-4595-0.
- Univ. of Wisconsin, Local Anesthesia and Regional Anesthetics
- Weinberg GL, VadeBoncouer T, Ramaraju GA, Garcia-Amaro MF, Cwik MJ (April 1998). "Pretreatment or resuscitation with a lipid infusion shifts the dose-response to bupivacaine-induced asystole in rats". Anesthesiology. 88 (4): 1071–5. doi:10.1097/00000542-199804000-00028. PMID 9579517. S2CID 1661916.
- Weinberg G, Ripper R, Feinstein DL, Hoffman W (2003). "Lipid emulsion infusion rescues dogs from bupivacaine-induced cardiac toxicity". Regional Anesthesia and Pain Medicine. 28 (3): 198–202. doi:10.1053/rapm.2003.50041. PMID 12772136. S2CID 6247454.
- Picard J, Meek T (February 2006). "Lipid emulsion to treat overdose of local anaesthetic: the gift of the glob". Anaesthesia. 61 (2): 107–9. doi:10.1111/j.1365-2044.2005.04494.x. PMID 16430560. S2CID 29843241.
- Rosenblatt MA, Abel M, Fischer GW, Itzkovich CJ, Eisenkraft JB (July 2006). "Successful use of a 20% lipid emulsion to resuscitate a patient after a presumed bupivacaine-related cardiac arrest". Anesthesiology. 105 (1): 217–8. doi:10.1097/00000542-200607000-00033. PMID 16810015. S2CID 40214528.
- Litz RJ, Popp M, Stehr SN, Koch T (August 2006). "Successful resuscitation of a patient with ropivacaine-induced asystole after axillary plexus block using lipid infusion". Anaesthesia. 61 (8): 800–1. doi:10.1111/j.1365-2044.2006.04740.x. PMID 16867094. S2CID 43125067.
- Cave G, Harvey M (September 2009). "Intravenous lipid emulsion as antidote beyond local anesthetic toxicity: a systematic review". Academic Emergency Medicine. 16 (9): 815–24. doi:10.1111/j.1553-2712.2009.00499.x. PMID 19845549.
- "Association of Anesthesists of Great Britain and Ireland home page" (PDF).
- Sirianni AJ, Osterhoudt KC, Calello DP, Muller AA, Waterhouse MR, Goodkin MB, Weinberg GL, Henretig FM (April 2008). "Use of lipid emulsion in the resuscitation of a patient with prolonged cardiovascular collapse after overdose of bupropion and lamotrigine". Annals of Emergency Medicine. 51 (4): 412–5, 415.e1. doi:10.1016/j.annemergmed.2007.06.004. PMID 17766009.
- "lipidrescue - Sample LipidRescue Kit". lipidrescue.squarespace.com.
- Harvey M, Cave G (February 2007). "Intralipid outperforms sodium bicarbonate in a rabbit model of clomipramine toxicity". Annals of Emergency Medicine. 49 (2): 178–85, 185.e1–4. doi:10.1016/j.annemergmed.2006.07.016. PMID 17098328.
- Harvey M, Cave G, Hoggett K (February 2009). "Correlation of plasma and peritoneal diasylate clomipramine concentration with hemodynamic recovery after intralipid infusion in rabbits". Academic Emergency Medicine. 16 (2): 151–6. doi:10.1111/j.1553-2712.2008.00313.x. PMID 19133855.
- Crandell DE, Weinberg GL (April 2009). "Moxidectin toxicosis in a puppy successfully treated with intravenous lipids". Journal of Veterinary Emergency and Critical Care. 19 (2): 181–6. doi:10.1111/j.1476-4431.2009.00402.x. PMID 19691569.
- Sandner-Kiesling A, Li X, Eisenach JC (December 2001). "Morphine-induced spinal release of adenosine is reduced in neuropathic rats". Anesthesiology. 95 (6): 1455–9. doi:10.1097/00000542-200112000-00026. PMID 11748405. S2CID 11365339.
- "BestBets: The Effect of Warming Local Anaesthetics on Pain of Infiltration". bestbets.org.
- Kampe S, Warm M, Kasper SM, Diefenbach C (July 2003). "Concept for postoperative analgesia after pedicled TRAM flaps: continuous wound instillation with 0.2% ropivacaine via multilumen catheters. A report of two cases". British Journal of Plastic Surgery. 56 (5): 478–83. doi:10.1016/S0007-1226(03)00180-2. PMID 12890461.
- Malamed SF (2013). Handbook of local anesthesia (6th ed.). St. Louis, Missouri: Elsevier. ISBN 9780323074131. OCLC 769141511.
- Meechan JG (December 1992). "Intraligamentary anaesthesia". Journal of Dentistry. 20 (6): 325–32. doi:10.1016/0300-5712(92)90018-8. PMID 1452871.
- Blanton PL, Jeske AH (June 2003). "The key to profound local anesthesia: neuroanatomy". Journal of the American Dental Association. 134 (6): 753–60. doi:10.14219/jada.archive.2003.0262. PMID 12839412.
- Boynes SG (1 June 2018). "Intraligamentary Injections in Dentistry" (PDF). Dental Academy of Continuing Education.
- Meechan JG (November 2002). "Supplementary routes to local anaesthesia". International Endodontic Journal. 35 (11): 885–96. doi:10.1046/j.1365-2591.2002.00592.x. PMID 12453016.
- D'Souza JE, Walton RE, Peterson LC (March 1987). "Periodontal ligament injection: an evaluation of the extent of anesthesia and postinjection discomfort". Journal of the American Dental Association. 114 (3): 341–4. doi:10.14219/jada.archive.1987.0080. PMID 3470356.
- Shastry SP, Kaul R, Baroudi K, Umar D (December 2014). "Hemophilia A: Dental considerations and management". Journal of International Society of Preventive & Community Dentistry. 4 (Suppl 3): S147–52. doi:10.4103/2231-0762.149022. PMC 4304051. PMID 25625071.
- Nazif M (January 1970). "Local anesthesia for patients with hemophilia". ASDC Journal of Dentistry for Children. 37 (1): 79–84. PMID 4904493.
- Moore PA, Haas DA (October 2010). "Paresthesias in dentistry". Dental Clinics of North America. 54 (4): 715–30. doi:10.1016/j.cden.2010.06.016. PMID 20831934.
- Shabazfar N, Daubländer M, Al-Nawas B, Kämmerer PW (2014). "Periodontal intraligament injection as alternative to inferior alveolar nerve block--meta-analysis of the literature from 1979 to 2012". Clinical Oral Investigations. 18 (2): 351–8. doi:10.1007/s00784-013-1113-1. PMID 24077785. S2CID 9525498.
- Nelson PW. Injection system. J Am Dent Assoc. 1981.
- Galili D, Kaufman E, Garfunkel AD, et al. Intraligamental anesthesia – a histological study. International Journal of Oral and Maxillofacial Surgery. 1984.
- Pashley D (October 1986). "Systemic effects of intraligamental injections". Journal of Endodontics. 12 (10): 501–4. doi:10.1016/s0099-2399(86)80206-0. PMID 3465856.
- Walton RE, Abbott BJ (October 1981). "Periodontal ligament injection: a clinical evaluation". Journal of the American Dental Association. 103 (4): 571–5. doi:10.14219/jada.archive.1981.0307. PMID 6945341.
- Smith GN, Walton RE, Abbott BJ (December 1983). "Clinical evaluation of periodontal ligament anesthesia using a pressure syringe". Journal of the American Dental Association. 107 (6): 953–6. doi:10.14219/jada.archive.1983.0357. PMID 6581222.
- Roberts GJ, Holzel HS, Sury MR, Simmons NA, Gardner P, Longhurst P (January 1997). "Dental bacteremia in children". Pediatric Cardiology. 18 (1): 24–7. doi:10.1007/s002469900103. PMID 8960488. S2CID 7178684.
- Kaufman E, Galili D, Garfunkel AA (March 1983). "Intraligamentary anesthesia: a clinical study". The Journal of Prosthetic Dentistry. 49 (3): 337–9. doi:10.1016/0022-3913(83)90273-1. PMID 6573480.
- Malamed SF (February 1982). "The periodontal ligament (PDL) injection: an alternative to inferior alveolar nerve block". Oral Surgery, Oral Medicine, and Oral Pathology. 53 (2): 117–21. doi:10.1016/0030-4220(82)90273-0. PMID 6949113.
- Meechan JG (January 1999). "How to overcome failed local anaesthesia". British Dental Journal. 186 (1): 15–20. doi:10.1038/sj.bdj.4800006. PMID 10028738. S2CID 6618968.
- Walton RE, Garnick JJ (January 1982). "The periodontal ligament injection: histologic effects on the periodontium in monkeys". Journal of Endodontics. 8 (1): 22–6. doi:10.1016/S0099-2399(82)80312-9. PMID 6948904.
- Hochman MN, Friedman MJ, Williams W, Hochman CB (June 2006). "Interstitial tissue pressure associated with dental injections: a clinical study". Quintessence International. 37 (6): 469–76. PMID 16752703.
- Aggarwal V, Singla M, Miglani S, Kohli S, Sharma V, Bhasin SS (January 2018). "Does the volume of supplemental intraligamentary injections affect the anaesthetic success rate after a failed primary inferior alveolar nerve block? A randomized-double blind clinical trial". International Endodontic Journal. 51 (1): 5–11. doi:10.1111/iej.12773. PMID 28370327.
- Berlin J, Nusstein J, Reader A, Beck M, Weaver J (March 2005). "Efficacy of articaine and lidocaine in a primary intraligamentary injection administered with a computer-controlled local anesthetic delivery system". Oral Surgery, Oral Medicine, Oral Pathology, Oral Radiology, and Endodontics. 99 (3): 361–6. doi:10.1016/j.tripleo.2004.11.009. PMID 15716846.
- Froum SJ, Tarnow D, Caiazzo A, Hochman MN (September 2000). "Histologic response to intraligament injections using a computerized local anesthetic delivery system. A pilot study in mini-swine". Journal of Periodontology. 71 (9): 1453–9. doi:10.1902/jop.2000.71.9.1453. PMID 11022775.
- Gow-Gates GA (April 1998). "The Gow-Gates mandibular block: regional anatomy and analgesia". Australian Endodontic Journal. 24 (1): 18–9. doi:10.1111/j.1747-4477.1998.tb00251.x. PMID 11431805.
- "Allergic Reactions". Cleveland Clinic. Retrieved 11 April 2014.
- Arnold Stern (2002). Pharmacology: PreTest self-assessment and review. New York: McGraw-Hill, Medical Pub. Division. ISBN 978-0-07-136704-2.
- Yagiela JA (1995). "Vasoconstrictor agents for local anesthesia". Anesthesia Progress. 42 (3–4): 116–20. PMC 2148913. PMID 8934977.
- Nielsen LJ, Lumholt P, Hölmich LR (October 2014). "[Local anaesthesia with vasoconstrictor is safe to use in areas with end-arteries in fingers, toes, noses and ears]". Ugeskrift for Laeger. 176 (44): 44. PMID 25354008.
- "Cocaine's use: From the Incas to the U.S." Boca Raton News. 4 April 1985. Retrieved 2 February 2014.
- López-Valverde A, de Vicente J, Martínez-Domínguez L, de Diego RG (July 2014). "Local anaesthesia through the action of cocaine, the oral mucosa and the Vienna group". British Dental Journal. 217 (1): 41–3. doi:10.1038/sj.bdj.2014.546. PMID 25012333.