Uterus
| Uterus | |
|---|---|
 Image showing different structures around and relating to the human uterus. | |
| Details | |
| Precursor | Paramesonephric duct |
| System | Reproductive system |
| Artery | Ovarian artery and uterine artery |
| Vein | Uterine veins |
| Lymph | Body and cervix to internal iliac lymph nodes, fundus to para-aortic lymph nodes, lumbar and superficial inguinal lymph nodes. |
| Identifiers | |
| Latin | uterus |
| Greek | ὑστέρα (hystéra) |
| MeSH | D014599 |
| TA98 | A09.1.03.001 |
| TA2 | 3500 |
| FMA | 17558 |
| Anatomical terminology | |

The uterus (from Latin "uterus", plural uteri) or womb (/wuːm/) is the main female hormone-responsive, secondary sex organ of the reproductive system in humans and most other mammals. Things occurring in the uterus are described with the term in utero. In the human, the lower end of the uterus, the cervix, opens into the vagina, while the upper end, the fundus, is connected to the fallopian tubes. It is within the uterus that the fetus develops during gestation. In the human embryo, the uterus develops from the paramesonephric ducts which fuse into the single organ known as a simplex uterus. The uterus has different forms in many other animals and in some it exists as two separate uteri known as a duplex uterus.
In medicine, and related professions the term uterus is consistently used, while the Germanic-derived term womb is commonly used in everyday contexts.
Structure
The uterus is located within the pelvic region immediately behind and almost overlying the bladder, and in front of the sigmoid colon. The human uterus is pear-shaped and about 7.6 cm (3.0 in) long, 4.5 cm (1.8 in) broad (side to side), and 3.0 cm (1.2 in) thick.[1][2] A typical adult uterus weighs about 60 grams. The uterus can be divided anatomically into four regions: the fundus – the uppermost rounded portion of the uterus, the corpus (body), the cervix, and the cervical canal. The cervix protrudes into the vagina. The uterus is held in position within the pelvis by ligaments, which are part of the endopelvic fascia. These ligaments include the pubocervical ligaments, the cardinal ligaments, and the uterosacral ligaments. It is covered by a sheet-like fold of peritoneum, the broad ligament.[3]
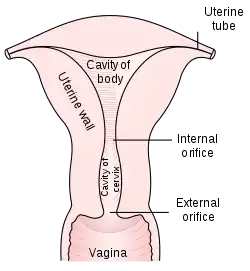
From outside to inside, regions of the uterus include:
- Cervix uteri – "neck of uterus"
- External orifice of the uterus
- Cervical canal
- Internal orifice of the uterus
- Body (Latin: Corpus)
- Uterine cavity
- Fundus
Layers
| Location | Mean (mm) | Range (mm) |
|---|---|---|
| Anterior wall | 23 | 17 - 25 |
| Posterior wall | 21 | 15 - 25 |
| Fundus | 20 | 15 - 22 |
| Isthmus | 10 | 8 - 22 |
The uterus has three layers, which together form the uterine wall. From innermost to outermost, these layers are the endometrium, myometrium, and perimetrium.[5]
The endometrium is the inner epithelial layer, along with its mucous membrane, of the mammalian uterus. It has a basal layer and a functional layer; the functional layer thickens and then is sloughed during the menstrual cycle or estrous cycle. During pregnancy, the uterine glands and blood vessels in the endometrium further increase in size and number and form the decidua. Vascular spaces fuse and become interconnected, forming the placenta, which supplies oxygen and nutrition to the embryo and fetus.[6][7]
The myometrium of the uterus mostly consists of smooth muscle. The innermost layer of myometrium is known as the junctional zone, which becomes thickened in adenomyosis.[8]
The perimetrium is a serous layer of visceral peritoneum. It covers the outer surface of the uterus.[9]
Surrounding the uterus is a layer or band of fibrous and fatty connective tissue called the parametrium that connects the uterus to other tissues of the pelvis.
Commensal organisms are present in the uterus and form the uterine microbiome.[10][11][12][13]
 Vertical section of mucous membrane of human uterus.
Vertical section of mucous membrane of human uterus.
Support

The uterus is primarily supported by the pelvic diaphragm, perineal body, and urogenital diaphragm. Secondarily, it is supported by ligaments, including the peritoneal ligament and the broad ligament of uterus.[14]
Major ligaments
It is held in place by several peritoneal ligaments, of which the following are the most important (there are two of each):
| Name | From | To |
|---|---|---|
| Uterosacral ligaments | Posterior cervix | Anterior face of sacrum |
| Cardinal ligaments | Side of the cervix | Ischial spines |
| Pubocervical ligaments[14] | Side of the cervix | Pubic symphysis |
Axis
Normally, the uterus lies in anteversion and anteflexion. In most women, the long axis of the uterus is bent forward on the long axis of the vagina, against the urinary bladder. This position is referred to as anteversion of the uterus. Furthermore, the long axis of the body of the uterus is bent forward at the level of the internal os with the long axis of the cervix. This position is termed anteflexion of the uterus.[15] The uterus assumes an anteverted position in 50% of women, a retroverted position in 25% of women, and a midposed position in the remaining 25% of women.[1]
Position
The uterus is in the middle of the pelvic cavity in frontal plane (due to broad ligament of the uterus). The fundus does not surpass the linea terminalis, while the vaginal part of the cervix does not extend below the interspinal line. The uterus is mobile and moves posteriorly under the pressure of a full bladder, or anteriorly under the pressure of a full rectum. If both are full, it moves upwards. Increased intra-abdominal pressure pushes it downwards. The mobility is conferred to it by musculo-fibrous apparatus that consists of suspensory and sustentacular part. Under normal circumstances the suspensory part keeps the uterus in anteflexion and anteversion (in 90% of women) and keeps it "floating" in the pelvis. The meaning of these terms are described below:
| Distinction | More common | Less common |
|---|---|---|
| Position tipped | "Anteverted": Tipped forward | "Retroverted": Tipped backwards |
| Position of fundus | "Anteflexed": Fundus is pointing forward relative to the cervix | "Retroflexed": Fundus is pointing backward |
The sustentacular part supports the pelvic organs and comprises the larger pelvic diaphragm in the back and the smaller urogenital diaphragm in the front.
The pathological changes of the position of the uterus are:
- retroversion/retroflexion, if it is fixed
- hyperanteflexion – tipped too forward; most commonly congenital, but may be caused by tumors
- anteposition, retroposition, lateroposition – the whole uterus is moved; caused by parametritis or tumors
- elevation, descensus, prolapse
- rotation (the whole uterus rotates around its longitudinal axis), torsion (only the body of the uterus rotates around)
- inversion
In cases where the uterus is "tipped", also known as retroverted uterus, the woman may have symptoms of pain during sexual intercourse, pelvic pain during menstruation, minor incontinence, urinary tract infections, fertility difficulties,[16] and difficulty using tampons. A pelvic examination by a doctor can determine if a uterus is tipped.[17]
Blood supply

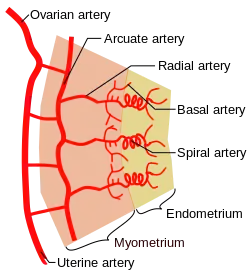
The uterus is supplied by arterial blood both from the uterine artery and the ovarian artery. Another anastomotic branch may also supply the uterus from anastomosis of these two arteries.
Nerve supply
Afferent nerves supplying the uterus are T11 and T12. Sympathetic supply is from the hypogastric plexus and the ovarian plexus. Parasympathetic supply is from the S2, S3 and S4 nerves.
Development
Bilateral Müllerian ducts form during early fetal life. In males, anti-müllerian hormone (AMH) secreted from the testes leads to their regression. In females, these ducts give rise to the Fallopian tubes and the uterus. In humans the lower segments of the two ducts fuse to form a single uterus, however, in cases of uterine malformations this development may be disturbed. The different uterine forms in various mammals are due to various degrees of fusion of the two Müllerian ducts.
Various congenital conditions of the uterus can develop in utero. Though uncommon some of these are a double uterus, didelphic uterus, bicornate uterus and others.[18]
Function
The reproductive function of the uterus is to accept a fertilized ovum which passes through the utero-tubal junction from the fallopian tube. The fertilized ovum divides to become a blastocyst, which implants into the endometrium and derives nourishment from blood vessels, which develop exclusively for this purpose. The fertilized ovum becomes an embryo, attaches to a wall of the uterus, creates a placenta, and develops into a fetus (gestates) until childbirth. Due to anatomical barriers such as the pelvis, the uterus is pushed partially into the abdomen due to its expansion during pregnancy. Even during pregnancy the mass of a human uterus amounts to only about a kilogram (2.2 pounds).
The uterus also plays a role in sexual response, by directing blood flow to the pelvis and ovaries, and to the external genitals, including the vagina, labia, and clitoris.
There is also some evidence that the uterus plays a role in cognition in a similar way to the ovaries. A study on rat models found that when the uterus was removed, the rats performed more poorly on spatial memory tasks. Prof. Bimonte-Nelson, the co-author of the study, explained: "the body's autonomic nervous system, which regulates 'automated' metabolic processes, such as heart rate, breathing, digestion, and sexual arousal, also has links to the uterus and brain."[19] No similar studies have yet been conducted on humans.
Clinical significance
A hysterectomy is the surgical removal of the uterus which may be carried out for a number of reasons including the ridding of tumours both benign and malignant. A complete hysterectomy involves the removal of the body, fundus, and cervix of the uterus. A partial hysterectomy may just involve the removal of the uterine body while leaving the cervix intact. It is the most commonly performed gynecological surgical procedure.
During pregnancy the growth rate of the fetus can be assessed by measuring the fundal height.
Some pathological states include:
- Prolapse of the uterus
- Carcinoma of the cervix – malignant neoplasm
- Carcinoma of the uterus – malignant neoplasm
- Fibroids – benign neoplasms
- Adenomyosis – ectopic growth of endometrial tissue within the myometrium
- Endometritis, infection at the uterine cavity
- Pyometra – infection of the uterus, most commonly seen in dogs
- Uterine malformations mainly congenital malformations including Uterine Didelphys, bicornuate uterus and septate uterus. It also includes congenital absence of the uterus Rokitansky syndrome
- Asherman's syndrome, also known as intrauterine adhesions, occurs when the basal layer of the endometrium is damaged by instrumentation (e.g., D&C) or infection (e.g., endometrial tuberculosis) resulting in endometrial scarring followed by adhesion formation that partially or completely obliterates the uterine cavity
- Hematometra, which is accumulation of blood within the uterus.[20]

- Accumulation of fluids other than blood or of unknown constitution. One study came to the conclusion that postmenopausal women with endometrial fluid collection on gynecologic ultrasonography should undergo endometrial biopsy if the endometrial lining is thicker than 3 mm or if the endometrial fluid is echogenic. In cases of a lining 3 mm or less and clear endometrial fluid, endometrial biopsy was not regarded to be necessary, but endocervical curettage to rule out endocervical cancer was recommended.[21]
- Myometritis – inflammation of the muscular uterine wall.[22]
Other animals
Most animals that lay eggs, such as birds and reptiles, including most ovoviviparous species, have an oviduct instead of a uterus. However, recent research into the biology of the viviparous (not merely ovoviviparous) skink Trachylepis ivensi has revealed development of a very close analogue to eutherian mammalian placental development.[23]
In monotremes, mammals which lay eggs, namely the platypus and the echidnas, either the term uterus or oviduct is used to describe the same organ, but the egg does not develop a placenta within the mother and thus does not receive further nourishment after formation and fertilization.
Marsupials have two uteri, each of which connect to a lateral vagina and which both use a third, middle "vagina" which functions as the birth canal.[24][25] Marsupial embryos form a choriovitelline placenta (which can be thought of as something between a monotreme egg and a "true" placenta), in which the egg's yolk sac supplies a large part of the embryo's nutrition but also attaches to the uterine wall and takes nutrients from the mother's bloodstream. However, bandicoots also have a rudimentary chorioallantoic placenta, similar to those of placental mammals.
The fetus usually develops fully in placental mammals and only partially in marsupials including kangaroos and opossums. In marsupials the uterus forms as a duplex organ of two uteri. In monotremes (egg-laying mammals) such as the platypus, the uterus is duplex and rather than nurturing the embryo, secretes the shell around the egg. It is essentially identical with the shell gland of birds and reptiles, with which the uterus is homologous.[26]
In mammals, the four main forms of the uterus are: duplex, bipartite, bicornuate and simplex.[27]
- Duplex
- There are two wholly separate uteri, with one fallopian tube each. Found in marsupials (such as kangaroos, Tasmanian devils, opossums, etc.), rodents (such as mice, rats, and guinea pigs), and lagomorpha (rabbits and hares).
- Bipartite
- The two uteri are separate for most of their length, but share a single cervix. Found in ruminants (deer, moose, elk etc.), hyraxes, cats, and horses.
- Bicornuate
- The upper parts of the uterus remain separate, but the lower parts are fused into a single structure. Found in dogs, pigs, elephants, whales, dolphins,[28] and tarsiers, and strepsirrhine primates among others.
- Simplex
- The entire uterus is fused into a single organ. Found in higher primates (including humans and chimpanzees). Occasionally, some individual females (including humans) may have a bicornuate uterus, a uterine malformation where the two parts of the uterus fail to fuse completely during fetal development.
Two uteri usually form initially in a female and usually male fetus, and in placental mammals they may partially or completely fuse into a single uterus depending on the species. In many species with two uteri, only one is functional. Humans and other higher primates such as chimpanzees, usually have a single completely fused uterus, although in some individuals the uteri may not have completely fused.
Additional images
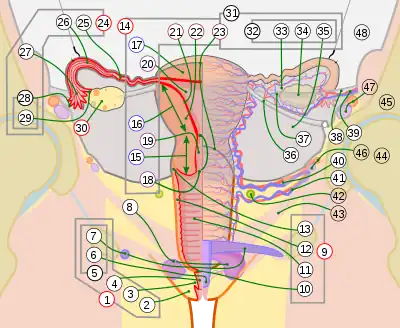
14. Uterus: Parts: 15. Cervix; 16. Body and 17. Fundus. 18. Orifices: External and Internal; 19. Cervical canal; 20. Uterine cavity; Layers: 21. Endometrium; 22. Myometrium and 23. Perimetrium
24. Fallopian tube
30. Ovary
31. Visceral pelvic peritoneum: 32. Broad ligament (with 35. Mesometrium)
Ligaments: 36. Round
Blood vessels: 40. Uterine artery and veins
Other: 42. Ureter; 46. Internal iliac vessels (anterior branches); 48. Abdominal cavity
 Schematic frontal view of female anatomy
Schematic frontal view of female anatomy
 Sectional plan of the gravid uterus in the third and fourth month.
Sectional plan of the gravid uterus in the third and fourth month. Fetus in utero, between fifth and sixth months.
Fetus in utero, between fifth and sixth months. Female pelvis and its contents, seen from above and in front.
Female pelvis and its contents, seen from above and in front. The arteries of the internal organs of generation of the female, seen from behind.
The arteries of the internal organs of generation of the female, seen from behind. Median sagittal section of female pelvis.
Median sagittal section of female pelvis.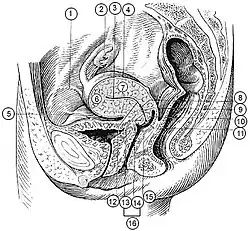 (Description located on image page)
(Description located on image page) Uterus
Uterus
See also
References
- 1 2 Manual of Obstetrics. (3rd ed.). Elsevier 2011. pp. 1–16. ISBN 9788131225561.
- ↑ Donita, D'Amico (2015). Health & physical assessment in nursing. Barbarito, Colleen (3rd ed.). Boston: Pearson. p. 645. ISBN 9780133876406. OCLC 894626609.
- ↑ Gray's Anatomy for Students, 2nd edition
- ↑ Nandita Palshetkar; Rishma Dhillon Pai; Hrishikesh D Pai (2012-09-30). Textbook of Hysteroscopy. JP Medical Ltd. pp. 135–. ISBN 978-93-5025-781-4.
- ↑ Tortora, G; Derrickson, B (2011). Principles of anatomy & physiology (13th. ed.). Wiley. p. 1105. ISBN 9780470646083.
- ↑ Blue Histology - Female Reproductive System Archived 2007-02-21 at the Wayback Machine. School of Anatomy and Human Biology — The University of Western Australia Accessed 20061228 20:35
- ↑ Guyton AC, Hall JE, eds. (2006). "Chapter 81 Female Physiology Before Pregnancy and Female Hormones". Textbook of Medical Physiology (11th ed.). Elsevier Saunders. pp. 1018ff. ISBN 9780721602400.
- ↑ "NCI Dictionary of Cancer Terms". National Cancer Institute. Archived from the original on 2017-12-26. Retrieved 2017-12-27.
- ↑ Ross, Michael H.; Pawlina, Wojciech. Histology, a text and atlas (Sixth ed.). p. 848.
- ↑ Franasiak, Jason M.; Scott, Richard T. (2015). "Reproductive tract microbiome in assisted reproductive technologies". Fertility and Sterility. 104 (6): 1364–1371. doi:10.1016/j.fertnstert.2015.10.012. ISSN 0015-0282. PMID 26597628.
- ↑ Verstraelen, Hans; Vilchez-Vargas, Ramiro; Desimpel, Fabian; Jauregui, Ruy; Vankeirsbilck, Nele; Weyers, Steven; Verhelst, Rita; De Sutter, Petra; Pieper, Dietmar H.; Van De Wiele, Tom (2016). "Characterisation of the human uterine microbiome in non-pregnant women through deep sequencing of the V1-2 region of the 16S rRNA gene". PeerJ. 4: e1602. doi:10.7717/peerj.1602. ISSN 2167-8359. PMC 4730988. PMID 26823997.
- ↑ Mor, Gil; Kwon, Ja-Young (2015). "Trophoblast-microbiome interaction: a new paradigm on immune regulation". American Journal of Obstetrics and Gynecology. 213 (4): S131–S137. doi:10.1016/j.ajog.2015.06.039. ISSN 0002-9378. PMC 6800181. PMID 26428492.
- ↑ Payne, Matthew S.; Bayatibojakhi, Sara (2014). "Exploring Preterm Birth as a Polymicrobial Disease: An Overview of the Uterine Microbiome". Frontiers in Immunology. 5: 595. doi:10.3389/fimmu.2014.00595. ISSN 1664-3224. PMC 4245917. PMID 25505898.
- 1 2 The Pelvis University College Cork Archived from the original on 2008-02-27
- ↑ Snell, Clinical Anatomy by regions, 8th edition
- ↑ "Retroverted Uterus: What it is & How it Affects Pregnancy". www.womens-health.co.uk. Archived from the original on 2013-10-05.
- ↑ Tipped Uterus:Tilted Uterus Archived 2011-02-24 at the Wayback Machine AmericanPregnancy.org. Accessed 25 March 2011
- ↑ "Surgical Correction of Uterovaginal Anomalies | GLOWM". www.glowm.com. Archived from the original on 2017-12-28. Retrieved 2017-12-27.
- ↑ "The uterus plays a role in memory, study finds". Medical News Today. medicalnewstoday.com. 14 December 2018. Retrieved 24 September 2019.
- ↑ "Cervical Stenosis - Women's Health Issues - Merck Manuals Consumer Version". Merck Manuals Consumer Version. Retrieved 2018-11-07.
- ↑ Takacs P, De Santis T, Nicholas MC, Verma U, Strassberg R, Duthely L (November 2005). "Echogenic endometrial fluid collection in postmenopausal women is a significant risk factor for disease". J Ultrasound Med. 24 (11): 1477–81. doi:10.7863/jum.2005.24.11.1477. PMID 16239648. S2CID 20258522.
- ↑ "Myometritis - Medical Definition from MediLexicon". www.medilexicon.com. Archived from the original on 2016-12-29.
- ↑ Blackburn, D. G.; Flemming, A. F. (2011). "Invasive implantation and intimate placental associations in a placentotrophic African lizard, Trachylepis ivensi (scincidae)". Journal of Morphology. 273 (2): 137–59. doi:10.1002/jmor.11011. PMID 21956253. S2CID 5191828.
- ↑ Hugh Tyndale-Biscoe; Marilyn Renfree (30 January 1987). Reproductive Physiology of Marsupials. Cambridge University Press. ISBN 978-0-521-33792-2.
- ↑ Ronald M. Nowak (7 April 1999). Walker's Mammals of the World. JHU Press. ISBN 978-0-8018-5789-8.
- ↑ Romer, Alfred Sherwood; Parsons, Thomas S. (1977). The Vertebrate Body. Philadelphia, Pennsylvania: Holt-Saunders International. pp. 390–392. ISBN 0-03-910284-X.
- ↑ Lewitus, Eric, and Christophe Soligo. "Life-history correlates of placental structure in eutherian evolution Archived 2017-09-06 at the Wayback Machine." Evolutionary Biology 38.3 (2011): 287-305.
- ↑ Bernd Würsig; William F. Perrin; J.G.M. Thewissen (26 February 2009). Encyclopedia of Marine Mammals. Academic Press. ISBN 978-0-08-091993-5.
External links
| Look up womb or uterus in Wiktionary, the free dictionary. |
| Wikimedia Commons has media related to uterus. |
- Anatomy photo:43:01-0102 at the SUNY Downstate Medical Center – "The Female Pelvis: Organs in the Female and male Pelvis in situ"
- Encyclopedia.com
- Uterus Anatomy
- Uterus Pregnancy