Parathyroid Glands
The parathyroid glands are small endocrine glands that produce parathyroid hormone. Most people have four parathyroid glands; however, the number can vary from two to six. These glands are located on the posterior surface of the thyroid gland. Normally, there is a superior gland and an inferior gland associated with each of the thyroid's two lobes . Each parathyroid gland is covered by connective tissue and contains many secretory cells that are associated with a capillary network. There are two major types of cells that make up parathyroid tissue: oxyphil cells and chief cells, the latter of which actually produce parathyroid hormone. The function of oxyphil cells is unknown.
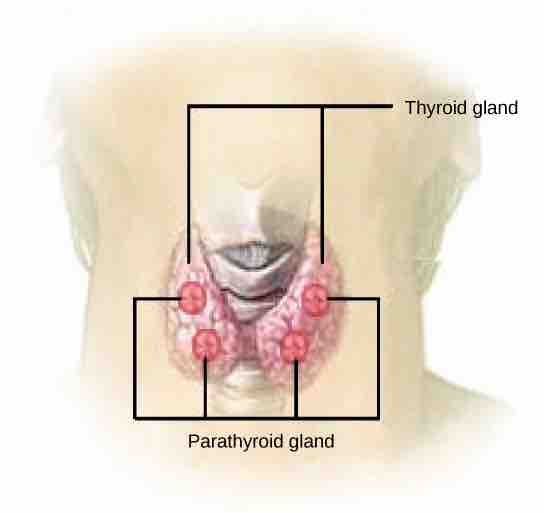
Parathyroid glands
The parathyroid glands are located on the posterior of the thyroid gland. The parathyroid glands produce parathyroid hormone (PTH) which increases blood calcium concentrations when calcium ion levels fall below normal.
One of the parathyroid glands' most important functions is to regulate the body's calcium and phosphorus levels. Another function of the parathyroid glands is to secrete parathyroid hormone, which causes the release of the calcium present in bone to extracellular fluid.
Parathyroid hormone (PTH), also known as parathormone, is released directly into the bloodstream, traveling to its target cells, which are often quite far away. It then binds to a receptor (found either inside or on the surface of the target cells). Receptors bind a specific hormone, resulting in a specific physiologic (normal) response of the body.
Parathyroid Glands and Calcium Regulation
PTH opposes the effect of thyrocalcitonin (or calcitonin), a hormone produced by the thyroid gland that regulates calcium levels. It does this by removing calcium from its storage sites in bones and releasing it into the bloodstream. It also signals the kidneys to reabsorb more of this mineral, transporting it into the blood. PTH can also signal the small intestine to absorb calcium by transporting it from the diet into the blood. Calcium is important for metabolization to occur. Blood cannot clot without sufficient calcium. Skeletal muscles require this mineral in order to contract. A deficiency of PTH can lead to tetany, a condition characterized by muscle weakness due to lack of available calcium in the blood.
More specifically, PTH increases blood calcium concentrations when calcium ion levels fall below normal. First, PTH enhances reabsorption of calcium by the kidneys; it then stimulates osteoclast activity and inhibits osteoblast activity. Finally, PTH stimulates synthesis and secretion of calcitriol by the kidneys, which enhances Ca2+ absorption by the digestive system. PTH and calcitonin work in opposition to one another to maintain homeostatic calcium levels in body fluids.